MONEY
As The Beatles sing: “money, money, money, money, monnneeeyyyy;” money makes the world go round, they say. Money is the necessary evil. And yet money is what puts food on the table, it’s what allows us to rent or own our place of service, hire our outstanding team, order the necessary supplies, and pay laboratory cases. Money is necessary and needed to create the outstanding experiences our patients crave and it’s needed to heal and help our patients.
However, as necessary as money is, and will continue to be, on our journey to become dentists, we learn very little about money, about overhead, about accounting, payroll, taxes, tax write-offs, practice loans, or profit and loss statements. It’s been a long time, too long to mention, but I don’t’ remember having a class in dental school where us, the young, bright eyed and bushy tailed future dentists, would find out what it actually takes to practice dentistry, logistically.
I learned about Krebs cycle (already covered in undergrad) and about placing class 2 amalgam restorations (never to be placed in private practice). Yet, I’d learned nothing about how much procedures cost or how to calculate what they should cost. I’d learned nothing about what overhead is, the cost of lab work or supplies, about payroll, about expectation of income for myself or any other team member in my practice. To this day, I still remember setting up several carps of anesthetic and needles, 10+ so-flex disks, 5+ resin carpules in my 3rd year clinic, only to dispose of them all, entirely untouched and unused when the patient failed the appointment. No one told me otherwise.
No one told me I was throwing out close to $50+ worth of supplies per patient. I cringe at the thought. In the last 15+ years, I have done a lot of learning on this subject, have taken many practice management courses, worked with several accountants, bookkeepers, and even hired consultants and coaches to now have a very secure and thorough understanding on what it’s like to run a profitable business. Profitable not just for me, but more importantly…for my team members.
CAN WE COMPETE?
The intent of this article is to shed light on how, in a PPO driven practice, such as my own, with write-offs, contractual fees, insurance maximums and the such, it is possible to generate enough production to pay our co-provider, the hygienist, the newly revised hourly wage. Pre-covid times, allotted high $30’s, low $40’s as an hourly wage for a hygienist in an insurance driven practice, while today, more and more hygienists are looking for an hourly wage closer to $50+ an hour.
This leaves many practice owners, most of whom accept some form of insurance payment, scratching their heads at how to make ends meet, how to go from paying $38/an hour to $55/an hour with no increase in our own reimbursement. The shortage of hygienists and an increased expectation of wage has also left many dentists without our perio co-therapist, most likely impacting patient experiences, pushing off recall visits, and likely reducing the overall production of the practice.
The reason why finances are an important part of the conversation in healing the previously discussed divide between the contemporary RDH and dentist is partly because many RDH’s feel the reward they receive is no longer worth the effort. One of the greatest concerns is not just a stagnant salary, one that may not have increased in years, but also lack of benefits.
Dentists have noticed the great resignation in the workforce and of 1,200 polled, 4 in 10 are still on the look out for clinical team members, hygienists being at the front of that need. Those dentists looking have also noticed a general upward trend in what is being asked in terms of compensation. So, again, from the 1200 polled, 8 of 10 have given out salary increases, benefits and paid time off to their teams, in keeping up with the condition.
The average increase among those polled has hovered at 3-6% which is significantly lower than what I am seeing in my geographic area.
Another aspect driving up the requested RDH salary in the market is the increasing presence of DSO’s. These large organizations have the ability to increase their reimbursement by negotiating on behalf of bulks of practices and providers; they reduce costs further by negotiating supplies and laboratory fees.
With all of those savings on the table, DSO’s have the cash to guarantee not just a higher level of income for the hygienists but also benefits such as medical insurance and paid time off. And if our burnt-out co-provider has come to a place where they desire a higher wage with great benefits, how can a private practice with a much higher overhead compete?
A MISUNDERSTANDING IN MONEY
When our contemporary hygienists are looking for this 30%+ increase in wage, they are unaware of all the moving parts that involve running a practice, just as we (dentists) were unaware post-graduation. In their eyes, they have new non-negotiables for accepting employment opportunities, and they feel they are worth that significant jump.
What they may not understand in that ask, is how numbers go into creating that reality for them. And if we, as dental students, as potential practice owners, aren’t taught much about crunching those numbers, the likelihood is that neither are the hygienists. They don’t know that as practice providers in the insurance game, our reimbursement rates have not gone up in the past decade. In fact, in some instances, they have gone down, especially taking inflation into consideration.
They may not know that most supply companies have raised their fees. Ultradent sent out an email earlier in the year informing a fee increase of 6% across the board (email sent out 3/30/33). They may not know that gloves and masks have more than doubled in cost. And in making an equation work, if our overhead costs listed have gone up, but our reimbursements have either stayed the same or gone down, how can private practice owners afford a 30% increase in salary, plus medical insurance and paid time off?
Not everyone finds the discussion of numbers exciting but let us gently move into that, because it is an integral part of the equation we are trying to create when finding the funds to increase RDH salaries. Christine Uhen, Investment Grade Practice Business Advisor at Productive Dentist Academy is helping me with this part of the article.
Her expertise tells us:
“The reality is that overhead in a dental practice can vary widely based on multiple factors. Average overhead nationwide as reported by the ADA in 2020 is at 61.8% but can vary between 60-75%, not including the doctor’s salary or benefits. This is the true cost of doing business. Compensation to a dentist as a provider/employee ranges from 25-40% of their net production.”
That is gross production, which is the full fee or standard fee minus write-offs.
Christine continues, “Team expenses are typically the largest portion of a dental practice’s overhead expenses. Prior to 2020, the ideal team compensation (including wages, benefits and payroll taxes) was 25% or less of collections. Today we often see team expenses closer to 28%. This presents a new challenge when it comes to practice profitability.”
“A rudimentary and accurate gauge for the first level of profitability in a hygiene department is that the net production for a hygienist should be 3 times their salary. So, for a hygienist who is earning $50/hour, their average hourly net production needs to be at $150 to cover their salary, benefits, PTO, and general overhead expenses. In a heavy PPO environment, that can be difficult to do.”
NUMBER CRUNCHING
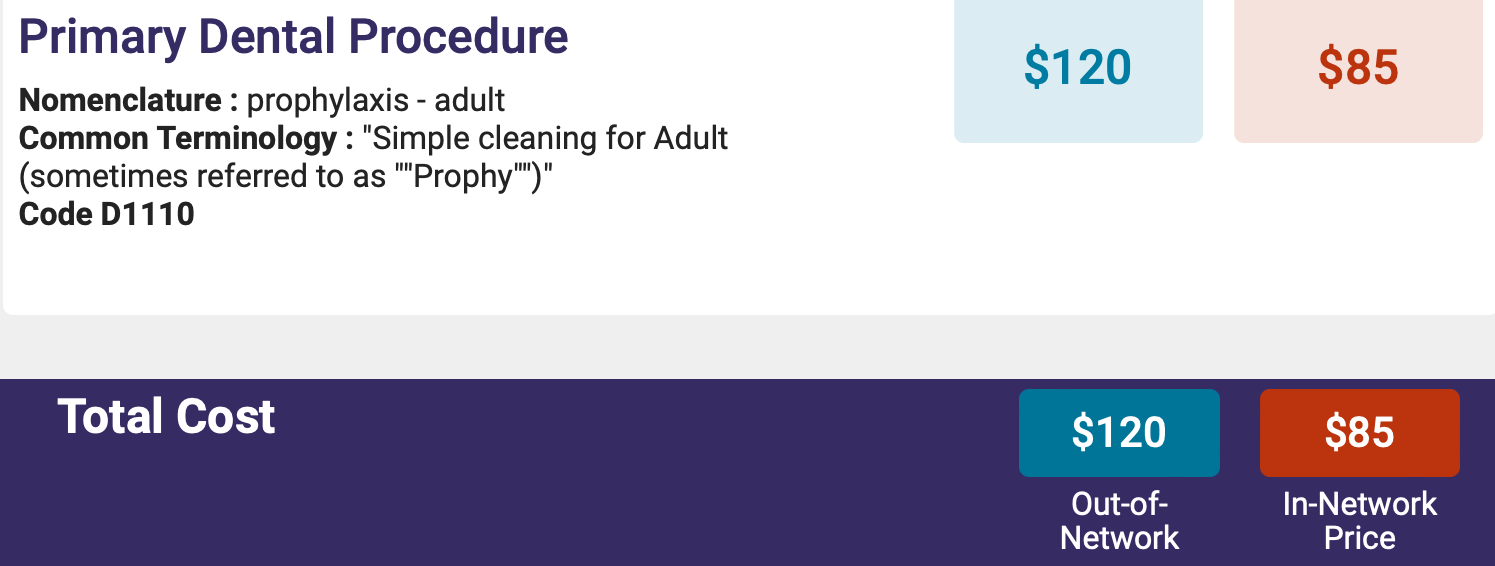
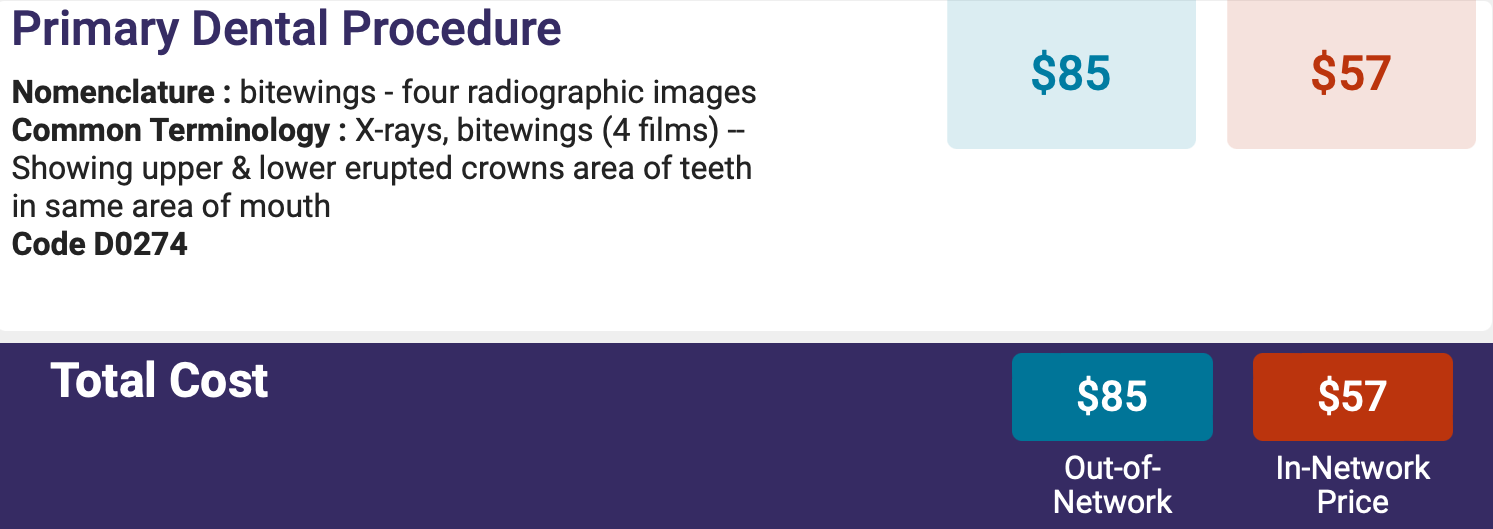
Before we move forward, let’s take a closer look at how likely it is for a hygienist in a PPO given practice to generate $150 per hour. In my office, a prophylaxis code (D1110) is at an average of $77 and x-rays generate a reimbursement of $50[7]. If two appointments are needed for a healthy patient annually, the average recall appointment for the year hovers around $102. The patient deserves an entire hour appointment, despite the industry wide trend to slash these appointments to 40 minutes.
If the production coming out of that chair is at ~$100 per hour, there doesn’t appear to be much wiggle room for that $50+ hourly pay.
To circumvent this you can add chair-side procedures which are generally not covered by insurance such as arestin, adult fluoride, laser therapy, VELscope, saliva testing, nutritional counseling, smoking cessation counseling, and myotherapy.
Those procedures are not a fit for every practice.
Back to Christine: “True practice profitability is not exclusive to the hygiene department. When the overall practice focus is on the best care for the patients, both the hygiene department and the entire practice will be profitable. A valuable hygienist customizes care for the patient and knows how to tee-up the dentist for comprehensive diagnosis. For example, patients who consider themselves healthy may have clinical evidence of additional dental disease. In addition to potential periodontal disease, hygienists can identify the early warning signs of decay, occlusal trauma and oral cancer. When a hygienist has advanced training, they become co-diagnosticians on all comprehensive dental care. This philosophy of care primarily benefits the patient but also can benefit the practice long-term creating the opportunity for an abundance of dental treatments.“
But that kind of hygienist—well-trained and focused—comes at a price.
A price of $50+ an hour.
THE SOLUTION – THINKING OUTSIDE THE BOX
Uhen specifies: “Historically, a second doctor chair has been used for patient overflow, post-operative checks, crown seats, bite adjustments, and emergency visits.”
With the kind of change we’ve been experiencing in dentistry, both past and ahead, perhaps this ought to be rethought. A new outlook would allow this second, well-equipped, and properly scheduled operatory to generate the extra income needed to close the RDH salary gap. This second chair would now be utilized by the dentist for minor production. It could potentially add 30-50% more personal production to the schedule per doctor. The chair would also require a dedicated, well trained, dental assistant.
Hear me out: The average production for a dentist in the United States hovers at less than $500 an hour. Most dentists produce out of a single chair with additional 1-2 chairs dedicated to the hygienist and recall visits. Looking at this very conservatively, in the new model of running a second doctor chair, 1 or 2 direct restorations per hour would bring in additional $250+ per hour. And this would take no more than 10-15 minutes of doctor time, not chair time, not assistant time, just doctor time.
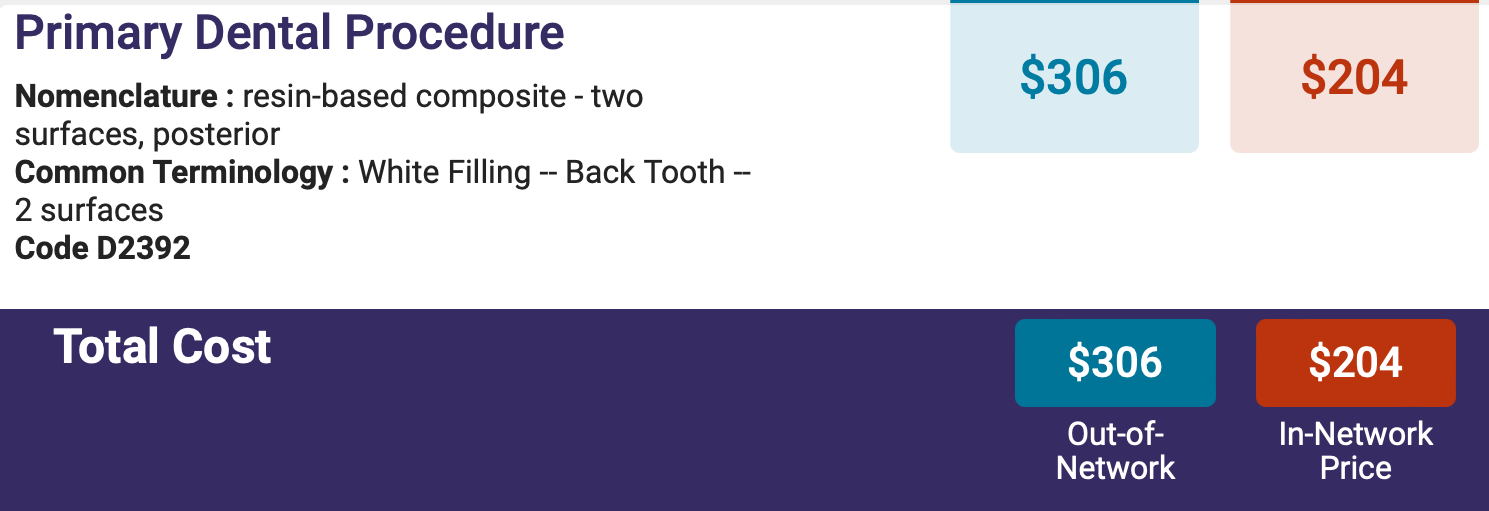
As you can see below, one posterior direct restoration could increase production by $160-$204 per hour.
$250+ additional hourly production:
- 30% ($75) for provider
- 5% ($12.5) for variable costs
- $20-25/per hour for dental assistant
- Total overhead: $107.50 – $112.50
- Total profit: $142.50 – $137.50
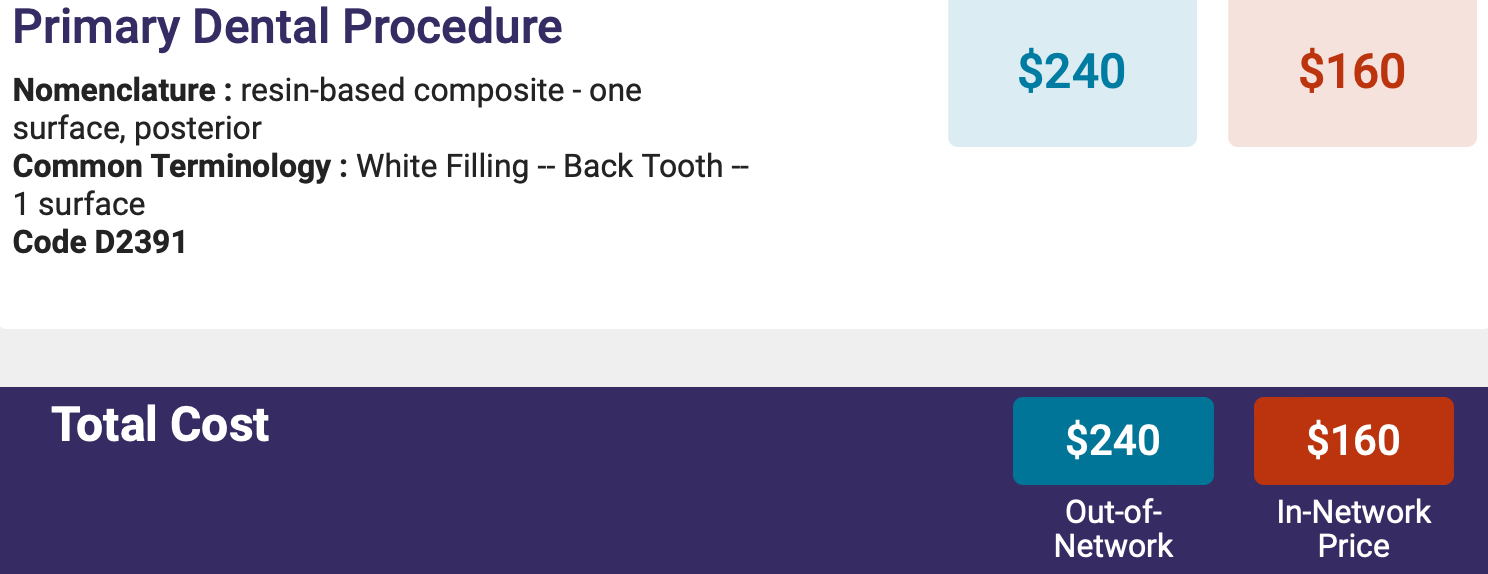
The only increase in overhead, in this scenario, is an additional assistant and the variable expenses, because all fixed costs have already been paid for. If 30% of production goes to provider ($75), 5% in variable costs ($12.5), $20-25 to the assistant per hour, you’re left with $142.50 to $137.50 of additional income.
This additional income is what would be used to level out the RDH salary. Problem solved.
Christine challenges you: “Imagine what a second chair will look and feel like in your practice: What services do you love to provide? How many hours can you schedule in that chair? The reality is the second chair will accelerate growth in the practice but only when the office as a whole is diagnosing and achieving greater case acceptance. This is where the value of a hygienist as a co-diagnostic partner is vital.”
Now, I know what you’re thinking, only because I’ve thought of the same thing: why do I have to stretch myself to work in another chair to supplement the income of an RDH?
The answer is very simple – having a well-compensated co-therapist is a tremendous asset to the practice. It’s also a tremendous asset to the provider, as it reduces workload in the hygiene department.
Christine explains, “Business growth is possible only when the office is diagnosing and achieving enough case acceptance to fill the schedule. This is where the value of a hygienist not just as a provider of services, but as a co-diagnostic partner is vital. In highly successful general dental practices 50% of the doctors’ production comes from existing patients. Those patients are most often seen by the hygienist. Doctors that invest time and training to create alignment of clinical philosophy and patient care with their hygienists make them invaluable. The result of this congruency is that the patient will choose the best care for themselves because they are confident in the recommendations from their entire dental co-diagnostic team. When they are willing to elevate their knowledge, diagnostic and communication skills to help patients move toward ideal dental health, dental hygienists elevate themselves as true partners in care with the dentist and remain vital and necessary component of a successful dental practice.”
The truth is there is justification and ability for meeting the salary increases the hygiene team is asking for. I sincerely hope that this information stays with you. It wasn’t over night that I understood, bought into, or considered it as a solution. It took me much time and much processing to come to place where I was willing to incorporate it into my practice.
And since I have, it’s worked, beautifully.
REFERENCES
- https://www.dentistrytoday.com/bridging-the-gap-difficult-conversations-between-dentist-hygienist/
- https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/jun2022_hpi_economic_outlook_dentistry_report_main.pdf?rev=37ad42b6e24643ada7ea989282a8ce2e&hash=09B92E4451DF79B5AB72DC89EE93429F
- https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/jun2022_hpi_economic_outlook_dentistry_report_main.pdf?rev=37ad42b6e24643ada7ea989282a8ce2e&hash=09B92E4451DF79B5AB72DC89EE93429F
- https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/jun2022_hpi_economic_outlook_dentistry_report_main.pdf?rev=37ad42b6e24643ada7ea989282a8ce2e&hash=09B92E4451DF79B5AB72DC89EE93429F
- https://www.aae.org/specialty/communique/dental-benefits-and-reimbursements/
- ADA Health Policy Institute, Survey of Dental Practice – https://www.ada.org/resources/research/health-policy-institute/dental-practice-research
- I am here using my own negotiated insurance rates, as I am in a PPO driven practice. You will also find images/screenshots from the Fair Health Website, for my zip code, showing the in network and out of network average fee for a procedure. Though not directly related to this article, you will see that my negotiated fees are still lower than what is considered average for my area.
- https://www.mgeonline.com/2020/how-much-should-a-general-dentist-produce-per-day/
ABOUT THE AUTHORS
Dr. Maggie Augustyn is a general dentist and writer in Elmhurst, Illinois. She earned her DDS degree from the University of Illinois Chicago, and has completed the course sequence in the Dawson Academy’s continuum in oral equilibration and cosmetic dentistry. Dr. Augustyn can be reached at maggie.augustyn@gmail.com.
Christine Uhen, GDH, BA, is an Investment Grade Practice Business Advisor and coach with Productive Dentist Academy optimizing practices and helping dentists build a business that supports their current lifestyle while creating an asset for their future. She began her dental journey 35 years ago providing comprehensive dental care in various roles such as clinical dental hygienist, surgical assistant, practice administrator and office manager. Today, Christine is a renowned dental speaker, author and practice management consultant.
She can be reached at christine@productivedentist.com.












