INTRODUCTION
In functional dentistry, structural integrity is directly linked to clinical performance and long-term prognosis. Anterior teeth are often the most susceptible first points of impact in traumatic dental incidents. Both direct and indirect modes of trauma and their sequelae must be considered. This extends beyond the initial salient structure loss, if any, and points to the long-term implications of a simple root canal treatment, particularly if the patient presents at a young age with hypertrophic pulp anatomy. While endodontic therapy is highly predictable, the restorative support and function of residual tooth structure is not. In individuals featuring existing Class III caries or restorations, further compromise of this structure augments the impact on the residual elastic modulus of the weakened tooth, which has a role in anterior guidance during dynamic occlusion function. To add insult to injury, there are often hemoglobin-derived residues present in the lumen of dentinal tubules, typically in the form of hemosiderin, which is dark in value and, thus, impacts the overall perceived brightness of the tooth. Aesthetic concerns often emotionally outweigh functional considerations in these individuals, the latter of which must not be overlooked when deciding the course of ideal treatment.
Functional aesthetics is a discipline with a focus on restoring functional parameters as a priority with a supplemental goal of enhancing the cosmetic appearance of the dentition.
Not all surfaces of an anterior tooth are equal in resisting bending or moment forces during function. Magne and Tan1 measured a 23% and 34% reduction in incisor flexural rigidity with moderate to aggressive Class III preparations. After bonded composite restorations were placed, 85% of the original crown stiffness was recovered. In the same study, a conservative endodontic access reduced the coronal stiffness by an insignificant margin in contrast to an aggressive endodontic access preparation, whereas a veneer preparation resulted in a 91% decrease in flexural integrity. The idea that anatomy imparts resistance to harmful forces during function has a direct correlation to areas with a localized bulk of enamel. On an incisor, these areas comprise the cingulum, lingual and facial marginal ridges, and facial cervical convexity.2 Finite element analysis studies found that compressive stresses, which are normally low and countered well in an intact tooth, are magnified up to an additional 150 MPa when the facial enamel is removed. The concept of minimizing enamel reduction in the cingulum is extended to bonded indirect veneer design, where margin designs chamfered on the palatal aspect extending in the area of the cingulum exhibited the highest tensile stresses. A veneer with a palatal butt joint or one with minimal overlap showed negligible tensile or even compressive stresses on the interface with tooth structure.3 It is always the aim to increase the height of natural ferrule on the palatal aspect, as this can significantly elevate the fracture resistance of preparations.4,5 A 1-mm increase in coronal dentin height has been established to double the fracture toughness of an endodontically treated tooth.6
From a naturomimetic standpoint, bonded porcelain restorations are best poised to replace missing enamel due to a closely matched elastic modulus relative to composite resin. This concept extends to the placement or replacement of Class III restorations in conjunction with veneer design. When a veneer is bonded in place and a significant Class III composite restoration is cured, the contractile stress from polymerization stresses the veneer-tooth interface. When thermal loads are applied, the designs with the lowest stresses are reflected in the variations with the maximal replacement of interdental composite by porcelain (ie, porcelain overlap).7 Hence, palatal prep-through designs for restorations with moderate to large Class III restorations are ideal for function.
CASE REPORT
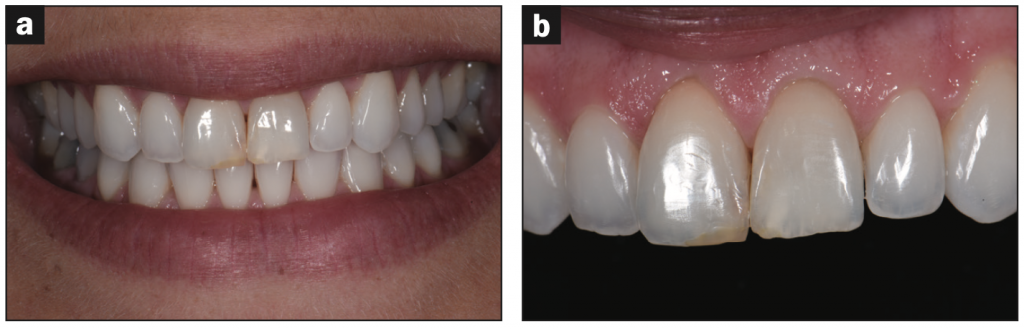
A healthy, ASA I, 22-year-old female presented to my practice, traveling from a distance for functional and aesthetic enhancement of teeth Nos. 8 and 9 (Figure 1). These teeth had been involved in dental trauma at an early age and thus had both been endodontically treated. The access cavities noted were excessive in size and linked to the presence of large Class III composite restorations proximally. The patient was concerned about the progressive darkening of the teeth. Clinically, her facial enamel shell was intact. Discussions revolved around the functional strength of the teeth and, in particular, the current compromise due to structure loss in critical areas. The patient was interested in composite veneers for the teeth, but as they were ideal in a buccopalatal location, additive resin layering would have resulted in prominent teeth in buccoversion, away from the ideal curve of the arch. The strategy for treatment involved lifting the color value of the teeth with a combination of internal bleaching and restorative effects to allow minimal preparation on the facial surfaces. In this way, a maximal volume of residual enamel and dentin would be preserved, maximizing the residual prognosis of the teeth. Instructions were given to the patient to return to her dentist for internal bleaching of the teeth before the palatal restorations and access cavities were restored with composite resin.
The patient returned to the practice 4 months later, with the internal bleaching result still exhibiting a lower value relative to the adjacent, healthy teeth. The patient reported that this was the final effort by the dentist and that she did not want to continue internally bleaching. The patient was warned about the potential need to compromise a greater volume of enamel with possible dentin exposure in order to effect a lift in value, a procedure that would compromise the flexural modulus of the tooth further.
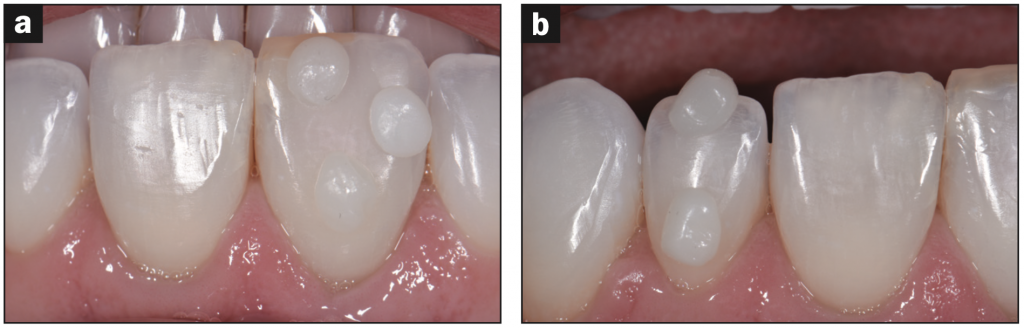
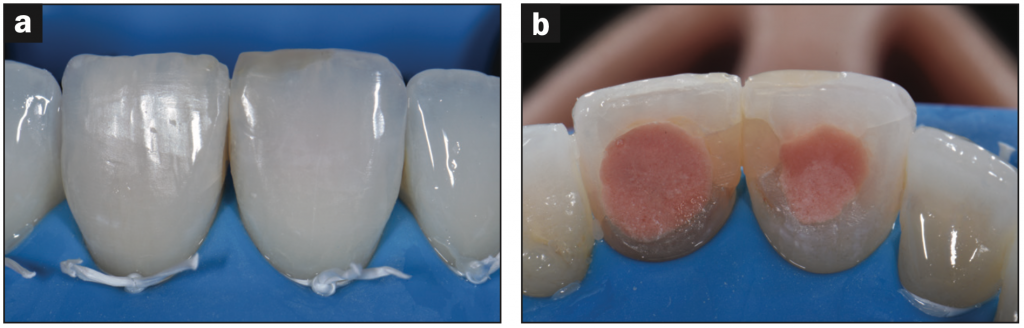
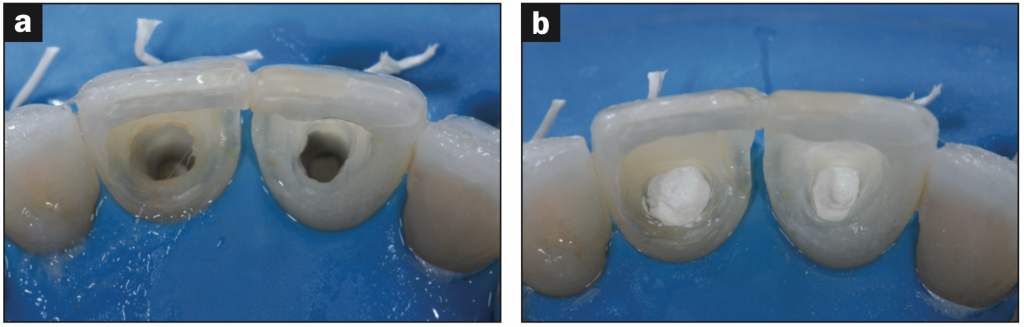
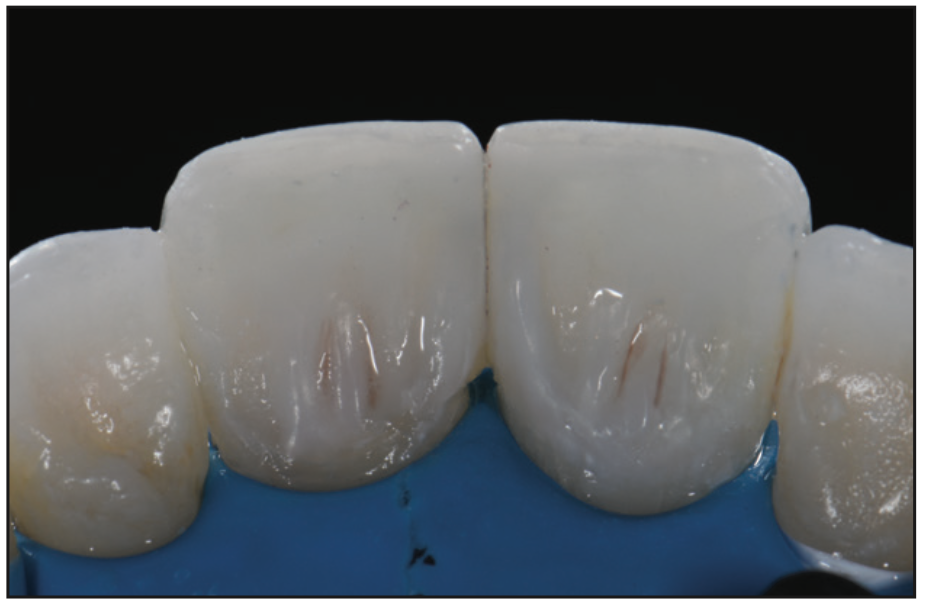
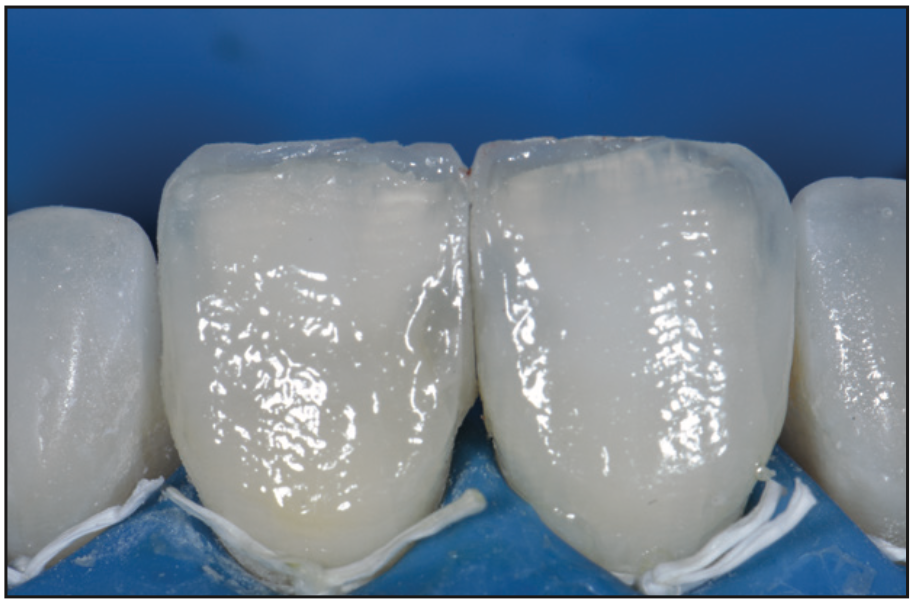
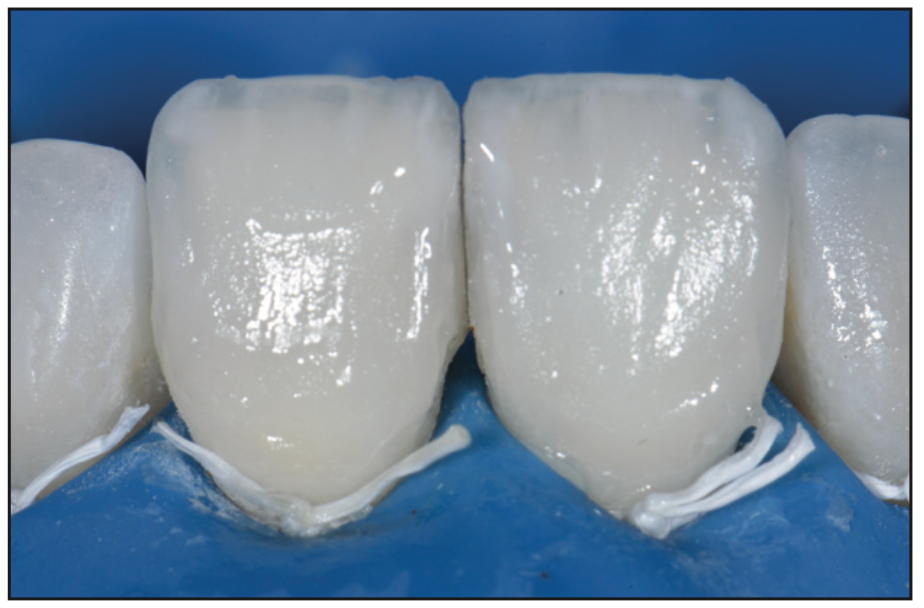
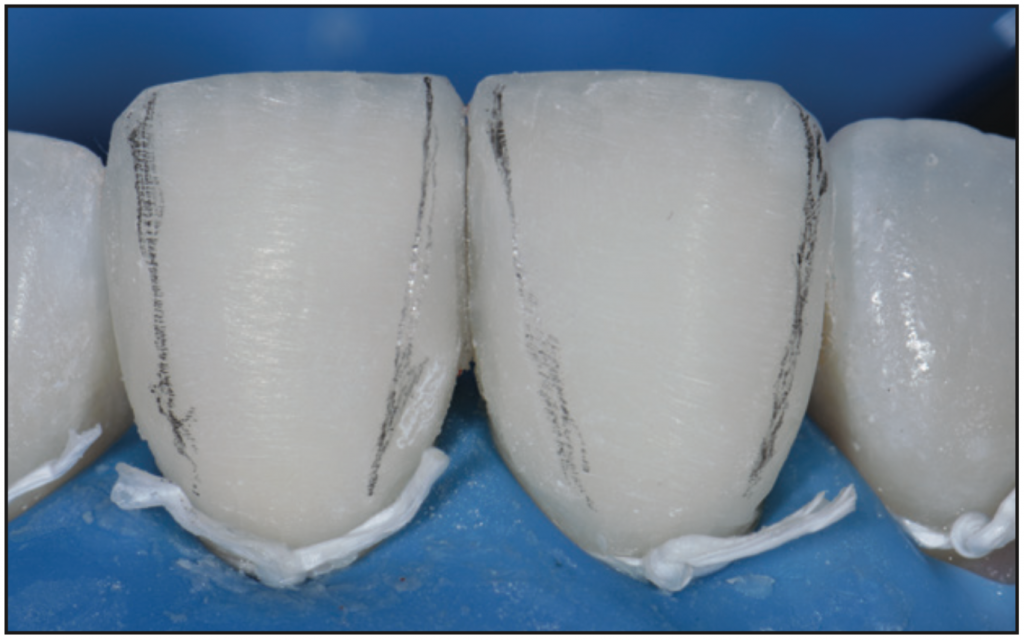
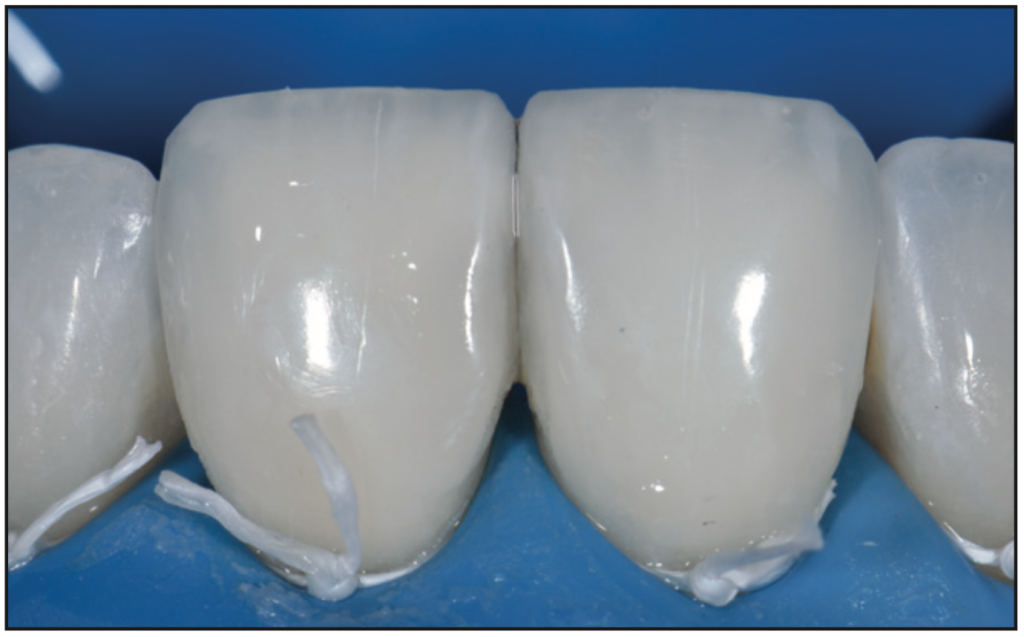
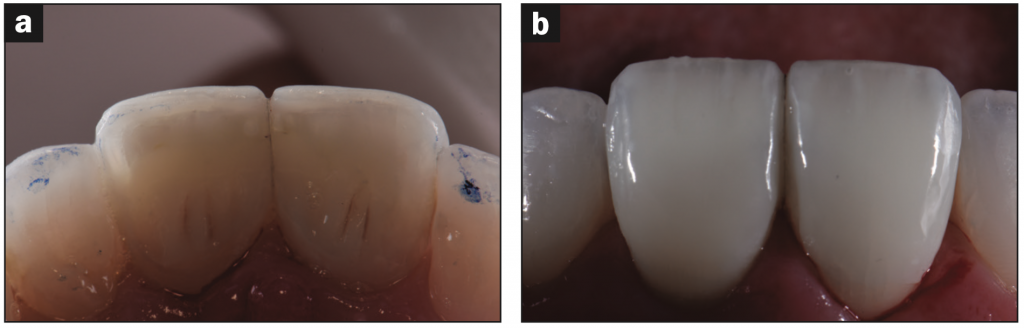
The desired facial composite shades were selected prior to any dehydration of the teeth (Figure 2). The patient was anesthetized, and a rubber dam affixed with floss ties (Figure 3). Endodontic access cavities were opened, and old Class III restorations were excavated, revealing a severe extent of missing pericervical dentin and axial wall structure (Figure 4). The gutta-percha was reduced to crestal level before sealing the orifice aspects using Fuji VII white (GC America) (Figure 5). After setting, the palatal aspect was micro air abraded using a 27-µm aluminum oxide powder at 2 bar of pressure (PrepStart [Zest Dental Solutions]). A total-etch adhesive approach was utilized (OptiBond Solo Plus [Kerr Dental]) before the buccal-facing surface internally was microlayered with a white opaque flowable composite (XL2, Herculite Ultra Flow Refill [Kerr Dental]) before more superficial layers were restored using micro-layers of A2 GrandioSO flowable (VOCO) (Figure 6). The residual facial wall was now as “white” as possible, with the value restoratively lifted. The shade exhibited increased opacity, likely due to the visibility of the white opaque material against the thin facial wall, with less depth of translucency relative to an intact tooth (Figure 7). The palatal anatomy was reconstructed focusing on initially layering the palatal marginal ridges and ensuring a natural convexity in their design. A single shade of A2 (GrandioSO) was utilized due to its exceptional flexural strength and wear resistance (Figure 8). The cingulum was completed next, along with secondary anatomy in the region, striving to re-create the bulk of cervical convexity with coronal extensions of the secondary lobes, also slightly convex and reaching into the palatal concavity.




The facial surface was lightly prepared (0.2 mm) to provide a minimal buccolingual volume for composite layering. After a total-etch adhesive approach (Figure 9 indicates the application of 33% orthophosphoric acid to the facioincisal aspect of the tooth, which was subsequently spread across the entire surface, not only in the pattern shown), the dentin, effect, and enamel shades were layered in typical fashion, and primary/secondary anatomy was established. The overall effect was a value-lifted, well-characterized composite veneer that was slightly opaque and high in value, which typifies the challenges with cases with a structural or positional compromise (Figures 10 to 16).


DISCUSSION
The goal of biomimetic dentistry is the re-creation of missing tooth structure in its attendant proportions and composition. This case featured central incisors with a severe paucity in structure, particularly on the palatal aspect, which is the area most responsible for the flexural resistance of an intact tooth. Elements that are critical for reconstruction of this area are a dentin-like and an enamel-like restorative material. Ideally, the elastic modulus of dentin, depending on if it’s peri-pulpal, peritubular, or intertubular, ranges from 5 to 30 GPa.8 It is best matched to composite resins, the bulk moduli of which range from 12.79 to 22.43 GPa, with a positive correlation noted between flexural modulus and filler volume fraction.9 From a biomimetic standpoint, the modulus of elasticity of proposed direct restoratives can thus even be matched with lower flexural modulus subtypes for deep dentin and higher modulus variants for superficial dentin. The advent of fiber-reinforced composite resin materials in the last decade now allows modern composite resins to have elevated fracture toughness that approximates or exceeds that of native dentin relative to regular composite. This is beneficial in minimizing the risk of crack propagation in structurally compromised teeth. Glass fiber-reinforced composites need to be contained internally via a closed sandwich technique as ambient moisture may be wicked internally into the restoration, accelerating hydrolytic degradation. Although not utilized in this specific case, the use of glass fiber-reinforced composites would have allowed a bolstering of residual tooth structure and, by increasing the fracture toughness, would have potentially biased a coronal fracture in a more favorable, reparable manner.
Idealizing the value and chroma of the teeth prior to composite layering is the Achilles heel of this case. Had the value been corrected fully via internal bleaching, the need to use overly white and opaque restorative materials would have been avoided, along with the minimization of the need to reduce facially. This would have translated into restorations that exhibited a greater depth of translucency—indeed, invisible restorations. This case demonstrates what is possible adherent with what limitations exist using modern direct restoratives in the reconstruction and aesthetic enhancement of severely structurally compromised teeth.
It is needless to say that a bonded indirect solution may have added greater flexural support to the residual tooth structure, but given the patient’s age and financial priorities, a direct option was the most feasible at the time. The direct restorative material chosen, GrandioSO, ranks amongst the highest in flexural strength and elastic modulus in composite materials today. Indeed, the flexural strength of 187 MPa exceeds that of native dentin (165.6 MPa), and the elastic modulus is rated at 16.65 GPa (average dentin ranges from 16.55 to 18.62 GPa). Such super composites allow greater confidence in large-volume direct reconstructions, especially in cases where minimal invasion is sought. It is critical to reconstruct both facial and palatal anatomy with materials that best match the corresponding missing layers of tooth structure for maximal prognosis and predictable performance.
REFERENCES
1. Magne P, Tan DT. Incisor compliance following operative procedures: a rapid 3-D finite element analysis using micro-CT data. J Adhes Dent. 2008;10(1):49-56.
2. Magne P, Versluis A, Douglas WH. Rationalization of incisor shape: experimental-numerical analysis. J Prosthet Dent. 1999;81(3):345–55. doi:10.1016/s0022-3913(99)70279-9
3. Magne P, Douglas WH. Design optimization and evolution of bonded ceramics for the anterior dentition: a finite-element analysis. Quintessence Int. 1999;30(10):661–72.
4. Milot P, Stein RS. Root fracture in endodontically treated teeth related to post selection and crown design. J Prosthet Dent. 1992;68(3):428–35. doi:10.1016/0022-3913(92)90405-y
5. Zhang YY, Peng MD, Wang YN, et al. The effects of ferrule configuration on the anti-fracture ability of fiber post-restored teeth. J Dent. 2015;43(1):117–25. doi:10.1016/j.jdent.2014.10.003
6. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63(5):529–36. doi:10.1016/0022-3913(90)90070-s
7. Magne P, Douglas WH. Interdental design of porcelain veneers in the presence of composite fillings: finite element analysis of composite shrinkage and thermal stresses. Int J Prosthodont. 2000;13(2):117–24.
8. Kinney JH, Balooch M, Marshall SJ, et al. Hardness and Young’s modulus of human peritubular and intertubular dentine. Arch Oral Biol. 1996;41(1):9-13. doi:10.1016/0003-9969(95)00109-3
9. Masouras K, Silikas N, Watts DC. Correlation of filler content and elastic properties of resin-composites. Dent Mater. 2008;24(7):932–9. doi:10.1016/j.dental.2007.11.007
ABOUT THE AUTHOR
Dr. Tam received her DDS degree and completed her general practice residency in pediatric dentistry at the University of Western Ontario and the University of Toronto, respectively. Her practice has a focus on restorative and cosmetic dentistry. She is well-published in both the local and international dental press, writing articles, reviewing submissions, and developing prototype products and techniques in clinical dentistry. She frequently and continually lectures internationally. Dr. Tam is the immediate past chairperson and director of the New Zealand Academy of Cosmetic Dentistry. She is one of 2 dentists in Australasia who are board-certified, accredited members of the American Academy of Cosmetic Dentistry. Moreover, she maintains Fellowship status with the International Academy for Dental and Facial Esthetics. She sits on the board of Smiles for the Pacific, an educational trust and charity that aims to expand professional dentistry services across the South Pacific region. She can be reached at clarence.tam@gmail.com.
Disclosure: Dr. Tam receives financial compensation from VOCO America.


