The presence of palatal tori complicate the restoration of the maxilla when implant treatment or surgical removal of the tori are not viable options. In this article, a treatment approach is offered for replacement of a partially edentulous posterior segement where no distal abutment is present and a palatal torus precludes placement of a traditional removable partial denture.
The term torus (latin for bull) is used for these structures and refers to the bulbous shape and the fact that tori comprise hard, dense bone. A torus may be identified as a bony growth found at the midline of the palate, the lingual surface of the mandible in the premolar region, or on the buccal aspect of either the maxilla or mandible. Palatal tori may be either unilobular (with a smooth surface) or multilobular in form. Growth is very slow, and they are considered a normal anatomical feature. Histologically, tori consist of compact cortical bone—an extension of the normal underlying bone with a thin mucosal covering.1
Tori are common and are seen with increasing prevalence in aging populations.2,3 They have been identified in ancient skulls, indicating they are not a feature confined to modern man.4 References to tori have been in the literature for at least 180 years.4 Palatal tori can complicate prosthetic treatment to replace posterior teeth when implant placement or surgical removal of the tori are not options.5,6 Systemic health, financial, and personal issues may eliminate the im-plant option in some patients who have palatal tori. If there is no posterior abutment tooth or teeth, a removable partial denture is the prosthetic approach to replacing the missing posterior teeth.
Surgical removal of palatal tori involves a midpalatal incision and reflection of the soft tissue. Rotary surgical burs are utilized to create longitudinal grooves in the exostosis. A chisel and mallet are used to dislodge the segments of bone. The resulting surface irregularities are smoothed with rotary instruments and/or bone files.7 Because it is difficult to determine the distance between the nasal fossa and the superior border of the tori with radiographs, a potential surgical complication is a nasal communication. Another potential com-plication—hematoma under the palatal flap—may result from sagging of the tissue during healing. Placement of a surgical stent during the healing period will minimize hema-toma formation.
Fabrication of a traditional removable partial denture (RPD) can be difficult when a torus is present. The soft tissue overlaying the torus tends to be thin and can ulcerate easily when subjected to the pressure of a removable prosthesis. A Kennedy class II arch (unilateral posterior edentulous area) traditionally requires a major connector extending to the opposite side of the arch to gain retention of the RPD. The majority of distal extension attachments such as the ERA or Locator would not offer stability for a unilateral RPD without cross-arch stabilization. Palatal tori can prevent the usual placement of the major connector, resulting in disruption of speech and/or function. A distal extension intracoronal or extracoronal attachment will provide increased retention, but its stability requires a cross-arch connector. Should a bar-type attachment (such as a Hader or Dolder bar) be selected without a cross-arch connector, stability is sacrificed and the occlusal load is transferred to the abutment teeth.
A double-bar attachment (the Branson bar) eliminates rotation on the bar, increasing stability and allowing load trans-fer to the underlying ridge without the need for a cross-arch connector.
When considering a RPD for a patient with a maxillary torus, it must be remembered that acrylic resin materials used for denture bases shrink during polymerization.8 Shrinkage during polymerization will affect how well the saddles fit the underlying residual ridge.9,10 Light-curable resins shrink less than heat-cured acrylic resins. Methylmethacrylate can shrink up to 7% by volume, whereas a monomer-free resin that is light curable demonstrates significantly less shrinkage.11
In the case presented in this article, a RPD was fabricated for a patient with a maxillary torus. A Branson bar attachment was used with a denture resin system that significantly decreases polymerization shrinkage.
THE BRANSON BAR ATTACHMENT
 |
| Figure 1. A cross-sectional drawing illustrating the spacing between the Branson metal components and the contact with the lateral walls of the ridge. |
The Branson bar (Andrews Restorative Systems) is a unilateral distal extension attachment developed by Dr. Jim Andrews more than 30 years ago.12 The attachment is a cantilever double bar with matching metal sleeve that retains a tissue-supported RPD.13,14 A space is placed between the double bar (occlusal surface) and the metal sleeve so that when the RPD is loaded, occlusal forces are not placed on the cantilevered attachment. Retentive contact is only between the vertical surfaces of the bar and sleeve. The RPD is supported by the residual ridge around the bar (buccal and palatal) and the entire tuberosity, with the bar serving only as a retentive element. The design prevents loading of the bar segment when the RPD is in place. Masticatory forces on the RPD are transferred to the edentulous ridge15-17 (Figure 1).
ECLIPSE DENTURE SYSTEM
Eclipse (DENTSPLY Trubyte), a thermoformable, light-curable denture resin system that eliminates the need for flasking and packing acrylic, was introduced in 2003. The system consists of a baseplate resin, set-up resin, and contour resin. The material is suited for traditional full dentures and partial dentures, and for use with cast partial frameworks. The baseplate resin is cured on a master cast and can be tried in prior to setting teeth to check fit and/or collect oc-clusal records. This baseplate becomes part of the final prosthesis, so the fit at the initial try-in appointment is identical to the fit at completion. The set-up resin is used to attach the denture teeth to the cured baseplate with the consistency of a hard wax prior to curing. Contour resin is overlayed on the baseplate, exposed set-up resin, and necks of the denture teeth. This material is highly polishable and easily carved prior to being cured. Eclipse material has strength that is similar to Lucitone 199 (DENTSPLY Trubyte), but polymerization shrink-age is decreased by more than 50%, increasing the accuracy of the final fit.18
CASE PRESENTATION
Treatment Planning
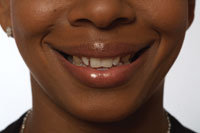
 |
| Figure 2. A large palatal tori adjacent to a partially edentulous posterior segment of the maxilla. |
A 75-year-old female patient presented with a mobile fixed maxillary prosthesis with abutments on the right first molar and second premolar. There were no clinically significant findings on the remaining maxillary teeth. Both of the abutment teeth on the right side had a poor periodontal prognosis. The patient was aware of the poor condition of the existing fixed bridge. It was noted that a palatal torus was causing a slight speech impediment (lisp) due to its size and inferior extent—level with the incisal edges of the anterior teeth (Figure 2). Placement of any part of a prosthesis covering the palate could worsen the speech impediment and possibly irritate the soft tissue covering the torus. The torus extended to the posterior border of the hard palate, making it impossible to achieve a posterior palatal seal or place a RPD connector anterior, posterior, or lateral to the torus with-out surgical removal of the torus.
One treatment option that was discussed was implant placement after augmentation of the right maxillary sinus. Prosthetic treatment would include a fixed, 3-unit bridge. This approach was not acceptable to the patient for financial reasons. An alternative treatment plan would involve surgical removal of the torus followed by placement of a conventional RPD. The patient expressed that due to her age and the long-standing nature of the torus, she did not want to have the surgical procedure.
A third treatment option involved an appliance that would avoid the torus. The remaining maxillary teeth demonstrated no mobility and were judged to be salvageable. Prep-aration of the 2 teeth adjacent to the edentulous space (the cuspid and lateral incisor) and placement of a fixed prosthesis with a cantilevered at-tachment (a Branson bar) was suggested. A RPD would then be placed that utilized the attachment for retention only and would be supported by the residual ridge that was buccal, lingual, and distal to the edentulous area.
The patient returned 2 months after the initial treatment-planning appointment. The fixed prosthesis and 2 abutment teeth had been removed from her mouth. She indicated that she wished to proceed with the Branson bar treatment approach.
TREATMENT PROCEDURE
The cuspid and lateral incisor were prepared for full-coverage porcelain-fused-to-metal restorations. A full-arch impression was made using a polyvinyl siloxane material (Correct, Pen-tron). An opposing full-arch impression was made with alginate (KromoPan, Lascod USA), and a PVS bite (Correct-bite, Pentron) was taken. Temporary restorations (Revotek, GC America) were fabricated for the prepared teeth and luted with Durelon cement (3M ESPE).
 |
 |
| Figure 3. Master model fabricated after a “pick-up” impression of the fixed prosthesis portion of the prosthetics. The metal sleeve is present on the Branson cantilever bar. | Figure 4. An occlusal view demonstrating the Branson bar. The pencil line indicates the coverage that the tissue-borne removable portion will cover. |
The fixed portion of the prosthesis was returned from the laboratory. Following removal of the temporary restorations, the prosthesis was tried in the mouth. A full-arch impression was made to capture the fixed prosthesis and its position relative to the edentulous area. A water-soluble lubricant was then brushed into the interior of the fixed units, and the temporary restorations were again luted on the teeth with Durelon. Dental stone was mixed and poured into the pick-up impression. After the stone set, the master cast and impression were separated. The fixed prosthesis remained on the master cast (Figure 3). A pencil was used to outline the extent of the saddle area for RPD coverage (Figure 4). The metal Branson sleeve was placed on the double bar, a PVS putty was mixed, and all undercuts around the Branson bar were blocked out.
 |
 |
| Figure 5. Eclipse baseplate resin is adapted over the Branson bar to cover the buccal and lingual sides of the ridge and the entire tuberosity. | Figure 6. An occlusal view of the uncured Esthet-X and Eclipse material. Note aesthetic blockout of the underlying bar in the premolar region. |
 |
 |
| Figure 7. Removal of the fixed and RPD segments of the prosthesis after curing. | Figure 8. Separation of the RPD and fixed segments of the prosthesis. Note the metal sleeve is incorporated into the RPD segment. |
The saddle areas of the edentulous space were carefully brushed with Al-Cote (DENTSPLY Trubyte), and the master cast was placed into the Eclipse conditioning oven, warming to 55ºC. The master cast was removed from the conditioning oven, and Eclipse baseplate resin was molded over the bar/sleeve and saddle area. Special care was taken to press the soft resin into the retention grooves of the metal sleeve (Figure 5). Because of limited available vertical space in the premolar region (due to the position of the attachment), it was decided to sculpt the premolars by hand from composite resin rather than adapt denture teeth in this area. A piece of Esthet-X opaque composite (shade W-O, DENTSPLY Caulk) was placed in the premolar area on the uncured Eclipse baseplate resin to block show-through of the underlying attachment (Figure 6). Air barrier coating (ABC, DENTSPLY Trubyte) was brushed over the resin to prevent an air-inhibited layer from forming on the exposed Eclipse resin as it was cured. The master cast was then placed into the Eclipse processing unit and cured for 10 minutes. Upon completion of cure the master cast was removed from the unit and soaked in water to aid in separation of the prosthesis from the cast. The entire prosthesis was removed and trimmed of any excess resin along the flanges (Figures 7 and 8). Care was taken to trim the palatal border so that the prosthesis did not impinge on the torus. The nontissue side of the RPD was roughened with a laboratory carbide bur to create a taper at the borders. The fixed and RPD segments were returned to the master cast and assembled.
 |
 |
| Figure 9. Esthet-X composite (shade C-3) was applied to simulate the body of the premolars. | Figure 10. Occlusal view showing rough anatomy to simulate pits and fissures. |
 |
| Figure 11. A darker shade was applied to the cervical region (shade D-3), and translucent Esthet-X (shade G-E) was overlayed to develop the final aesthetics. |
Prosthetically, 3 teeth would be placed on the RPD segment. A brown tinting resin, applied to simulate occlusal fissures, was cured with a hand-held light. A body shade of Esthet-X composite (shade C-3) was applied over the opaque resin and cured with a hand-held light (Figure 9). A diamond bur in a high-speed handpiece was used to roughly shape the premolars (Figure 10). Next, the cervical region of the premolars was covered with a darker shade of Esthet-X composite (shade D-3), and translucent Esthet-X (shade G-E) was placed to accomplish final shaping of the premolar teeth (Figure 11).
 |
 |
| Figure 12. Diatoric retention was developed in a molar denture tooth. | Figure 13. The molar denture tooth was attached to the baseplate with Eclipse set-up resin, overlayed with Eclipse contour resin, and festooned. |
 |
| Figure 14. An occlusal view of the prosthesis prior to final curing. |
 |
 |
| Figure 15. The prosthesis in the Eclipse processing unit prior to curing. Note the very pale pink appearance of the Eclipse resin. | Figure 16. Final processed Eclipse RPD. Note the gingival tone compared to the uncured set-up/contour resin in Figure 15. Cervical staining has been added with composite tinting resin to improve the aesthetics. |
A molar denture tooth was adapted to fit the space distal to the composite teeth. Retentive diatorics were placed on the denture tooth, and Eclipse set-up resin was applied to lute it to the baseplate (Figure 12). Eclipse contour resin was applied to cover the exposed baseplate and the cervical aspect of the composite teeth and denture tooth. Festooning was accomplished, and the RPD was ready for final processing (Figures 13 and 14). ABC was applied to all resin surfaces. Eclipse gel was applied to the RPD’s flanges to prevent warping during the final curing (Figure 15). The master cast was placed into the processing unit and cured for 10 minutes. The RPD was then removed from the master cast, and a laboratory carbide bur was used to remove any Eclipse gel from the flanges of the RPD. Cervical staining was added with composite tinting resin to improve the aesthetics (Figure 16). The RPD was then polished.
 |
 |
| Figure 17. A lateral view of the completed prosthesis. | Figure 18. An occlusal view of the luted fixed portion of the prosthesis demonstrating the double-bar design of the Branson attachment. |
 |
| Figure 19. An occlusal view of the completed prosthesis. |
The patient was then seen, and the temporary restorations were removed. The fixed portion of the prosthesis was placed, and the RPD was tried in. Proper fit and absence of movement of the RPD were verified. The fixed portion was then luted to the abutment teeth with a resin-reinforced glass ionomer agent (Fuji-Cem, GC America). Excess luting agent was removed, and again the RPD was tried in to check for stability (Figures 17 to 19). The occlusion was checked and adjusted as needed, and the patient was dismissed.
CONCLUSION
Anatomical features can complicate the replacement of missing teeth. Alternative treatment plans need to be developed when other options (surgical correction of the anatomical problem or implant placement) are not possible due to financial or personal reasons.
The Branson bar permits treatment of the edentulous ridge, stabilizing the RPD segment and eliminating rotational movements around the attachments. The result is transfer of the load to the underlying ridge. This decreases the load on the abutment teeth and improves long-term function. The Eclipse system permits fabrication of an accurately fitting prosthesis, due in large part to minimal polymerization shrinkage. The more intimate the fit of the RPD segment, the better the load transfer to the edentulous ridge.
References
1. Chew CL, Tan PH. Torus palatinus. A clinical study. Aust Dent J. 1984;29:245-248.
2. Chohayeb AA, Volpe AR. Occurrence of torus palatinus and mandibularis among women of different ethnic groups. Am J Dent. 2001;14:278-280.
3. Sonnier KE, Horning GM, Cohen ME. Palatal tubercles, palatal tori, and mandibular tori: prevalence and anatomical features in a U.S. population. J Periodontol. 1999;70:329-336.
4. Seah YH. Torus palatinus and torus mandibularis: a review of the literature. Aust Dent J. 1995;40:318-321.
5. Sawyer DR, Allison MJ, Elzay RP, Pezzia A. A study of torus palatinus and torus mandibularis in Pre-Columbian Peruvians. Am J Phys Anthropol. 1979;50:525-526.
6. MacInnis EL, Hardie J, Baig M, al-Sanea RA. Gigantiform Torus palatinus: review of the literature and report of a case. Int Dent J. 1998;48:40-43.
7. Sailer HF, Pajarola GF. Oral Surgery for the General Dentist (Color Atlas of Dental Medicine). Thieme Publishing, New York. 1999 296-97.
8. Patel MP, Braden M, Davy KW. Polymerization shrinkage of methacrylate esters. Biomaterials. 1987;8:53-56.
9. Ruyter IE, Oysaed H. Conversion in denture base polymers. J Biomed Mater Res. 1982;16:741-754.
10. Pow EH, Chow TW, Clark RK. Linear dimensional change of heat-cured acrylic resin complete dentures after reline and rebase. J Prosthet Dent. 1998;80:238-245.
11. Collard SM, Karimzadeh A, Smith LT, Parikh U. Polymerization shrinkage, impact strength and roughness of montmorillonite-modified denture base resins. Am J Dent. 1991;4:285-290.
12. Carlson AF. Introduction to the Andrews System of restorative dentistry. Quintessence Dent Technol. 1979;3:27-34.
13. Givan DA, Kolodney H Jr. Removable partial denture design with a splint bar and precision attachments. Compendium. 1993;14:670, 672, 674-676.
14. Andrews J. A unilateral, free-end, saddle bridge. Dent Today. 1998;17:120-121.
15. Andrews JA, Biggs WF. The Andrews bar-and-sleeve-retained bridge: a clinical report. Dent Today. 1999;18:94-96, 98-99.
16. Cheatham JL, Newland JR, Radentz WH, O’Brien R. The ‘fixed’ removable partial denture: report of case. J Am Dent Assoc. 1984;109:57-59.
17. Everhart RJ, Cavazos E Jr. Evaluation of a fixed removable partial denture: Andrews Bridge System. J Prosthet Dent. 1983;50:180-184.
18. Kurtzman GM, Melton, AB. Improving accuracy and simplifying treatment with full arch removable prosthetics. Dent Today. 2004;23:82-87.
Dr. Kurtzman is in private practice in Silver Spring, Md, and is an assistant clinical professor at the University of Maryland School of Dentistry, department of restorative dentistry. He is on the editorial board of the Journal of Oral Implantology, an assistant editor of the International Magazine of Oral Implantology, and editor of the Maryland Academy of General Dentistry. He has earned fellowships in the Academy of General Dentistry, the International Congress of Oral Implantologists, the Pierre Fauchard Academy, and American College of Dentists, and masterships in the Academy of General Dentistry and the Implant Prosthetic Section of the International Congress of Oral Implantologists. He can be contacted at dr_kurtzman@ maryland-implants.com.
Dr. Melton is a prosthodontist who graduated from Baylor University, College of Dentistry and received his training in fixed prosthetics from the University of Missouri-Kansas City. He is a member of the American College of Prosthodontics, the American Academy of Implant Dentistry, and the International Congress of Oral Implantology. He is a diplomat of the American Board of Oral Implantology/ Implant Dentistry, and the International Congress of Oral Implantology, and a fellow of the Academy of Dentistry International. His practice is located in Albuquerque and Santa Fe, NM, and is limited to prosthodontics and implant dentistry. He can be reached at (505) 883-7744.
To comment on this article, visit the discussion board at dentistrytoday.com.
|
Continuing Education Test No. 68.1
|
After reading this article, the individual will learn:
• the clinical complications posed by maxillary tori when restoring the partially edentulous maxilla, and
• a prosthetic approach to restoring the partially edentulous maxilla in the presence of a torus.
1. Tori are:
a. common.
b. rare.
c. seen with increasing prevalence in aging populations.
d. both a and c.
2. The following is (are) true for tori:
a. growth is fast.
b. growth is very slow.
c. tori are always unilobular.
d. both b and c.
3. Tori may be identified as a bony growth found at:
a. the midline of the palate.
b. the lingual surface of the mandible in the premolar region.
c. the buccal aspect of the maxilla or mandible.
d. all of the above.
4. What type of movement does the Branson bar eliminate?
a. vertical
b. horizontal
c. rotational
d. both a and b
5. What material has the least shrinkage during polymerization?
a. methylmethacrylate
b. Eclipse monomer-free resin
c. all light-curable resins
d. There is no shrinkage difference between resins.
6. Where is the retentive contact located in a Branson bar?
a. between the vertical surfaces of the bar and sleeves
b. only on the sleeves
c. only on the bar
d. none of the above
7. Polymerization shrinkage on Eclipse dentures is decreased by more than _____.
a. 20%
b. 30%
c. 40%
d. 50%
8. The Branson bar has what type of distal extension?
a. unilateral
b. bilateral
c. neither
d. can have both
To submit Continuing Education answers, download the answer sheet in PDF format (click Download Now button below). Print the answer sheet, identify the article (this one is Test 68.1), place an X in the box corresponding to the answer you believe is correct, and mail to Dentistry Today Department of Continuing Education (complete address is on the answer sheet).