For the past 15 years emphasis has moved away from resective periodontal surgery toward regenerative periodontal surgery. Infrabony defects have been treated with guided tissue regeneration (GTR) with or without the placement of materials that are allogeneic (a graft between genetically dissimilar members of the same species) or alloplastic (a graft being biocompatible or inert). In addition, it has been demonstrated that calcium sulfate (CS), when combined with demineralized freeze-dried bone allograft (DFDBA), can reduce the rapid resorption of both materials and can be used as a resorbable barrier for GTR.1 This is a variation of the original protocol, which employed calcium sulfate alone in osseous defects.2,3 Calcium sulfate is biodegradable, porous, noninflammatory, and readily available at a reduced expense compared to other regenerative materials.4,5 Calcium sulfate, useful as a binder, will harden when applied in periodontal defects and maintain its space by setting.6 However, CS does not induce bone regeneration due to rapid resorption and lack of chemotactic bioactivity.
In the case reports described in this article, calcium sulfate was mixed with a synthetic bioactive resorbable graft (SBRG) having a bioactive chemotactic response.7,8,9 This graft material has been used in a variety of bone augmentation cases alone or with DFDBA as a binder for sinus elevation procedures in which the material is well compacted.8,10
Results of one clinical and histologic study suggest that DFDBA alone may have little or no osteoinductive potential.11 Another study concluded that DFDBA does not induce bone regeneration, resorbs sporadically, and may in fact interfere with normal bone formation. After placement into a defect, the material maintains its sponge-like state and may act as an inhibitor to bone formation; thus it is not ideal for implant support.11,12 However, Garg reported that DFDBA, where the source may be cortical or trabecular bone, has osteoconductive and “possibly osteoinductive” properties, however, “they are not osteogenic.”13 In the particle size ranging from 150 to 1,000 µm, “DFDBA [grafts] are more effective and limited to periodontal defect applications.”13,14
The selection of synthetic materials (alloplasts), rather than organically derived materials, may be needed as a result of patients’ aversion to the use of human tissue and their concern for the risk of being infected with transmitted pathogens (ie, HIV, hepatitis) that escaped detection during testing and processing. DFDBA has been utilized safely in the treatment of periodontal defects for the past 15 years. Nevertheless, concerns have been raised about disease transmission when tissues or organs from one person are transplanted to another person. The safety of human-derived materials has recently been questioned due to transmission of the hepatitis C virus by tissue transplantation.15 Transmission of HIV infection from seronegative organ and tissue donors has occurred,16 and other potentially infectious agents (ie, the prion that is responsible for bovine spongiform encephalopathy) are extremely resistant to inactivation by normal disinfection or sterilization procedures.17 Although allogeneic or xenogeneic materials (human or bovine) used as grafts are treated with gamma radiation or by acid demineralization, and no incidents of disease transmission have been reported, the potential for disease transmission must be considered.17-19 This does not represent a problem for alloplastic graft material.
Synthetically derived materials have been utilized in periodontal surgery for more than 17 years. Although dense ceramic hydroxyapatite (CHA) may be biocompatible, clinical efficacy has been questioned.20,21 For example, a recent report suggests that epithelial down-growth observed with high-density materials of CHA may be attributed to lack of material consolidation relevant to the material’s density and chemical complexities.21 Further, the use of CHA has been associated with a lack of material resorption, leading to irregular infiltration of new bone as well as fibrous tissue encapsulation.21 Because of their chemical structure and/or physical density, nonresorbable graft materials and membranes break down, act as irritants, and sequester bone formation.21,22 Animal and human studies have demonstrated that fragmentation and transport of nonresorbable particulates spread into regional lymph nodes and other organs (lungs, spleen), which could interfere with the function of these tissues and organs, and could compromise the immune system.23,24
 |
 |
| Figure 1. SEM of OsteoGen showing one crystal cluster approximately 300 to 400 µm. | Figure 2. An x-ray diffraction pattern of OsteoGen demonstrating peaks for the hydroxylapatite groups as defined by the International Union of Crystallography and in cooperation with the American Society for Testing and Materials. |
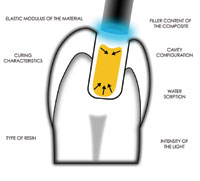
In contrast, studies indicate that SBRG (Figure 1) does not pose the problems that are associated with nonresorbable particulates. SBRG ionizes in situ into calcium and phosphate ions. For example, the 6-week and 12-week in vivo bone responses of low-temperature SBRG were studied and compared to CHA coatings, sputtered CHA coatings, and smooth and roughened titanium surfaces. Materials were analyzed by x-ray diffraction (Figure 2) and infrared spectrophotometry prior to implantation. The American Society for Testing and Materials has determined purity standards for ceramic hydroxyapatite. The analysis confirmed the presence of crystalline Ca10(PO4)6(OH)2 for SBRG particulates, which contained the hydroxyl groups (OH). This synthetic bioactive resorbable graft is chemically and crystallographically similar to human bone mineral and is different from high-temperature ceramic hydroxyapatites. Furthermore, it was found that there are no carbonate ions (CO3-2) in CHA as is seen for human bone (approximately 4% to 6%) and SBRG (approximately 2% to 3%).25 Undecalcified specimens were examined by light microscopy and microradiography. At each time interval, bone growth into titanium implant chambers was significantly greater with SBRG than with other materials. In addition, Ricci, et al concluded that the SBRG “materials showed bone directly surrounding and attaching to these materials without any visible interposing tissue.”26
In a study of sinus elevation by Artzi, et al,10 the author stated that all implants were successful. “Although rarely observed, fibrous encapsulation of some grafted (SBRG) particles could not be ruled out.” He also stated in his paper that implant studies by Fugazzotto had a 98% cumulative success rate over a 5-year period.
Due to a sintering process of CHA at high temperatures, it becomes OH deficient (dehydroxylated) and is classified as an oxyapatite (Ca10(PO4)6O2), not hydroxylapatite.27 In contrast, SBRG crystal growth and maturation is processed at lower temperatures and contains brushite (CaHPO4ï2H2O) and CaHPO4 (monetite) as a minor constituent. The chemical potentiality of brushite has been found to be the precursor phase to biologic hydroxylapatite in an embryonic environment, resulting in the first state of bone mineralization in situ.28,29 The minimal connective tissue migration observed with the low-temperature SBRG material is due mostly to brushite. The crystallographic morphology of SBRG (rectangular and hexagonal hydroxylapatite crystal formation) permits controlled dissolution of the brushite. In a study by Block and Meffert, it was observed that by grafting the crestal undercut portion of the implant neck, bone regeneration was observed. This technique was used “to prevent apical migration of the epithelium” due to the chemical potentiality of OsteoGen (Impladent Ltd), a synthetic bioactive resorbable graft. Further, SBRG has been associated with bone fill in human clinical trials.10,30,31
Alloplastic graft materials are readily available and inexpensive. These materials can be utilized as an alternative to autogenous donor material or allografts. Utilization of alloplastic materials is not associated with a potential immunologic response to antigens. Numerous animal and human studies have demonstrated histologic and clinical efficacy of low-temperature SBRG.32,33 In one such study involving grafts that were implanted into the ileum of rats, the SBRG material demonstrated a significant increase in bone formation as compared to the control of other graft materials when implanted for more than 7 days. Further, this study demonstrated that SBRG was associated with enhanced bone formation in bony voids as compared to plastic graft material, and that bone fill progressed over time. It
was concluded that SBRG also demonstrated a higher chemotactic response and cell-binding capacity when compared to plastic particulates.34 A study by Ruano, et al compared the effect of ceramic hydroxyapatite versus nonceramic hydroxylapatite (OsteoGen) for cell growth capacity and procollagen synthesis of cultured human gingival fibroblasts. The study showed that “viable cells were significantly fewer in numbers for cultures grown with ceramic hydroxylapatite when compared to OsteoGen.”35
In one recent human clinical study, sinus elevations, cyst cavities, and tooth extraction sites were grafted with SBRG particulate.36 No failures were reported. In another study, periapical abscess repair, ridge contouring, and bone formation were demonstrated using SBRG mixed with small quantities of collagen (Avitene [Davol, a subsidiary of C.R. Bard]) as a binder.36 At 4 and 14 months, histology demonstrated progressive bone ingrowth concurrent with replacement of the SBRG particles; ie, the granules were gradually resorbed and replaced with bone. In one case in which a defect was filled with SBRG and then covered with CHA, it was observed histologically that the CHA particles migrated downward from the crestal to the apical region. The nonresorbable CHA was fibroencapsulated and surrounded by macrophages and multinucleated giant cells in the same defect site. No such activity was evident around the remaining SBRG particulates.37,38
Human clinical studies indicate the clinical efficacy of SBRG.39,40 This material is chemically and mechanically similar to natural bone and is physically similar to bone in regard to trabeculation and resorption rate. Several studies have demonstrated that the material is consistenly radiolucent (at placement), however the material becomes radiopaque as progressive resorption and mineralization occurs (4 to 6 months postoperatively).10,41-44
In summary, nonceramic SBRG material offers a reasonable and inexpensive alternative to the placement of bone allograft materials for individuals who have concerns about allografts. As described previously, calcium sulfate, and in particular Capset (Lifecore Biomedical), has been used extensively in many dental applications. However, it is not well known that the material functions as a containment barrier to maintain graft particles in a defect site. It will function as a cell occlusive protective barrier to prevent unwanted cells, bacteria, and debris from occupying the defect space before bone regeneration can take place. In particular, rapid resorption has been associated with the common name of plaster of Paris. However, calcium sulfate of the alpha phase hemihydrate/hydroxypropyl methycellulose (hypromellose), when mixed with SBRG and hydrated with a limited solution of sterile water in a heavy consistency, will resorb in a controlled fashion.
SURGICAL PROTOCOL
With identification of an appropriate infrabony defect, local anesthesia is administered, and a full-thickness mucoperiosteal flap is reflected to visualize the defect. The area is debrided with hand and ultrasonic instrumentation to remove all granulomatous tissue and subgingival plaque and calculus. Based on studies that have demonstrated the potential of cementum and dentin to serve as reservoirs for tetracycline, it may be advantageous to treat the involved root surfaces prior to placement of the composite graft.45 In addition, tetracycline may positively affect cell adhesion, migration, and proliferation of fibroblasts, and may also be effective in removing the smear layer and opening dentin tubules,46,47 which a resorbable bioactive crystallite could fill.
Conditioning of the roots is performed by mixing one half of a 250-mg capsule of tetracycline with one half of a carpule (0.9 cc) of a local anesthetic that does not contain a vasoconstrictor (ie, epinephrine) in a dappen dish. Cotton pledgets are then placed in the mixture and allowed to soak for approximately 1 minute. Although the duration of root conditioning has been questioned, root burnishing for approximately 30 to 60 seconds is satisfactory.48 The area is then rinsed with sterile water or saline.49
The mixture of SBRG and calcium sulfate is prepared in a ratio of 4-to-1, respectively, and hydrated to a granular consistency with saline, water, or more effectively, the patient’s blood. This is transferred to the surgical site with a spatula, stainless steel syringe, or pre-filled syringe. An amalgam plugger or a blunt instrument, used with sterile gauze, is useful to compress and compact the mixture into the defect site. Bleeding at the site must be controlled prior to material delivery (eg, epinephrine or Avitene). It is important to avoid excessive bleeding, fluid contamination, and empty spaces due to insufficient compacting of the material, as bone does not bridge such spaces.
Once the osseous defect is overfilled with a mixture of SBRG and calcium sulfate, the mucoperiostal flaps are sutured. A protective periodontal dressing may be placed carefully over the surgical site without pressure to the graft; however, this is not mandatory. Postoperative instructions and a suitable analgesic are given to the patient; antibiotics and an antimicrobial mouthrinse (chlorhexidine) are also prescribed for 7 days. The patient is recalled the following week to remove the dressing and sutures. Patients are monitored for 1 month to detect any problems with healing, and maintenance therapy is continued every 3 months.
CASE PRESENTATIONS
Case 1
 |
 |
| Figure 3. Preoperative facial view reveals deep pocketing at the distal aspect of the lateral incisor. | Figure 4. Upon flap elevation, an infrabony defect is evident at the distal aspect of the lateral incisor. |
 |
 |
| Figure 5. Facial view 6 months postoperatively illustrates significant pocket reduction. | Figure 6. Two-year postoperative view demonstrates successful maintenance of pocket reduction. |
A 47-year-old male patient presented with deep pocketing in the interproximal area between the maxillary left lateral incisor and cuspid (Figure 3). Upon reflection of the mucoperiosteal flap, the infrabony defect was visualized (Figure 4). Once debridement was completed using hand and ultrasonic instrumentation, tetracycline was applied according to the aforementioned protocol. This process resulted in a “milk glass” appearance of the root surface. The combination graft of low-temperature synthetic bioactive resorbable material (OsteoGen) and calcium sulfate (Capset) was mixed and placed firmly within the defect with a slight overfilling prior to flap closure. The tissues were subsequently coapted with resorbable sutures. Significant pocket reduction was observed 6 months postoperatively (Figure 5); this trend continued over the course of a 2-year period (Figure 6).
Case 2
 |
 |
| Figure 7. Preoperative view reveals deep pocketing at the mesial aspect of the cuspid tooth. | Figure 8. Preoperative radiograph exhibits deep bone loss to apex. Extraneous amalgam particles line the apical portion of the defect. |
 |
 |
| Figure 9. The defect 2.5 years postoperatively displays significant reduction of the periodontal pocket. | Figure 10. Radiograph 2.5 years postoperatively indicates bone fill. |
A 51-year-old male patient was referred for treatment of a long-standing periodontal defect on the mesial surface of the mandibular left cuspid. A deep pocket with exudate was seen at the examination (Figure 7). An infrabony defect with amalgam particles at the apical extent was seen radiographically (Figure 8). The defect was treated via open flap debridement; the extraneous amalgam particles were removed, and the composite graft was placed. Significant reduction of the periodontal defect was observed clinically and radiographically 2.5 years postoperatively (Figures 9 and 10).
Case 3
 |
 |
| Figure 11. Facial view preoperatively. Note the presence of a deep pocket mesial to the incisors. | Figure 12. Presurgical radiograph demonstrates osseous defects mesial to the incisors. |
 |
 |
| Figure 13. Pocket depth is within acceptable limits 1 year postoperatively. | Figure 14. Radiographic view 2 years postoperatively confirms the osseous repair. |
A 63-year-old female patient presented with discomfort in the area of the maxillary right central incisor. Upon clinical evaluation, deep pocketing on the mesial aspect was detected (Figure 11). Endodontic evaluation confirmed the presence of a combined endodontic-periodontal lesion, and endodontic therapy was performed (Figure 12). Treatment of the residual defect was accomplished with placement of the composite graft following open debridement. The complete eradication of the infrabony defect was demonstrated clinically at 1 year and radiographically at 2 years (Figures 13 and 14).
Case 4
 |
 |
| Figure 15. Preoperative radiograph displays osseous loss to apex. Furcal involvement is also apparent. | Figure 16. Radiograph of the site 1 year postoperatively indicates osseous repair. |
A 63-year-old male patient with diabetes mellitus presented with pain and swelling in the area of the mandibular right first molar. Bone loss to the apex was noted in the preoperative radiograph (Figure 15). Furcation involvement was also noted. Following administration of local anesthesia, the area was debrided, and the composite graft was placed. An antibiotic was prescribed for 7 days. One year postoperatively the patient was asymptomatic, and marked resolution of the infrabony defect was evident (Figure 16).
CONCLUSION
Guided tissue regeneration (GTR) therapy has been described to treat periodontal infrabony defects.1,3-5 A new surgical technique adapts the principle of GTR therapy utilizing a synthetic bioactive resorbable graft (SBRG). Instead of using freeze-dried bone allograft and a membrane barrier, SBRG (Osteo-Gen) is used, which is mixed with calcium sulfate (Capset) in a 4-to-1 ratio, respectively. The advantages of this technique over more traditional techniques include a simplified surgical procedure, easy delivery, and a significant decrease in treatment time and cost without the risks associated with a second surgery, which is required if a nonresorbable GTR membrane is used. Specific patient concerns related to the use of biological materials is also addressed.
References
1. Sottosanti JS. Aesthetic extractions with calcium sulfate and the principles of guided tissue regeneration. Pract Periodontics Aesthet Dent. 1993;5:61-69.
2. Bahn SL. Plaster: a bone substitute. Oral Surg Oral Med Oral Pathol. 1966;21:672-681.
3. Shaffer CD, App GR. The use of plaster of paris in treating infrabony periodontal defects in humans. J Periodontol. 1971;42:685-690.
4. Anson D. Calcium sulfate: a 4-year observation of its use as a resorbable barrier in guided tissue regeneration of periodontal defects. Compend Contin Educ Dent. 1996;17:895-899.
5. Sottosanti J. Calcium sulfate: a biodegradable and biocompatible barrier for guided tissue regeneration. Compendium. 1992;13:226-234.
6. Alderman NE. Sterile plaster of paris as an implant in the infrabony environment: a preliminary study. J Periodontol. 1969;40:11-13.
7. Valen M, Ganz SD. A synthetic bioactive resorbable graft for predictable implant reconstruction: part one. J Oral Implantol. 2002:28:167-177.
8. Ganz SD, Valen M. Predictable synthetic bone grafting procedures for implant reconstruction: part two. J Oral Implantol. 2002;28:178-183.
9. Block CM, Tillmanns HW, Meffert RM, et al. Histologic evaluation of the LaminOss osteocompressive dental screw: a pilot study. Compend Contin Educ Dent. 1997;18:676-685.
10. Artzi Z, Nemcovsky CE, Dayan D. Nonceramic hydroxylapatite bone derivative in sinus augmentation procedures: clinical and histomorphometric observations in 10 consecutive cases. Int J Periodontics Restorative Dent. 2003;23:381-389.
11. Becker W, Urist M, Becker BE, et al. Clinical and histologic observations of sites implanted with intraoral autologous bone grafts or allografts. 15 human case reports. J Periodontol. 1996;67:1025-1033.
12. Becker W, Becker BE, Caffesse R. A comparison of demineralized freeze-dried bone and autologous bone to induce bone formation in human extraction sockets. J Periodontol. 1994;65:1128-1133.
13. Garg AK. Review of bone-grafting materials. In: Bywaters LC, Harmon L, eds. Bone Biology, Harvesting, and Grafting for Dental Implants: Rationale and Clinical Applications. Chicago, Ill: Quintessence Publishing Co; 2004:21-23.
14. Rummelhart JM, Mellonig JT, Gray JL, et al. A comparison of freeze-dried bone allograft and demineralized freeze-dried bone allograft in human periodontal osseous defects. J Periodontol. 1989;60:655-663.
15. Conrad EU, Gretch DR, Obermeyer KR, et al. Transmission of the hepatitis-C virus by tissue transplantation. J Bone Joint Surg Am. 1995;77:214-224.
16. Simonds RJ, Holmberg SD, Hurwitz RL, et al. Transmission of human immunodeficiency virus type 1 from a seronegative organ and tissue donor. N Engl J Med. 1992;326:726-732.
17. Friedman MA. Letter to manufacturers of FDA-regulated drug/biologic/device products, May 9, 1996. Food and Drug Administration Web site. Available at: www.fda.gov/cber/ltr/fdareg050996.pdf. Accessed December 2005.
18. FDA Strengthens Tissue Transplantation Regulations. AAOMS Digest, February (6), 1994.
19. Gross N. Mad cows and humans. Business Week. December 22, 1997;80-82.
20. Lovelace TB, Mellonig JT, Jones AA, et al. Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J Periodontol. 1998;69:1027-1035.
21. Zablotsky M. The surgical management of osseous defects associated with endosteal hydroxyapatite-coated and titanium dental implants. Dent Clin North Am. 1992;36:117-149.
22. Kossovsky N, Millett D, Juma S, et al. In vivo characterization of the inflammatory properties of poly(tetrafluoroethylene) particulates [published correction appears in J Biomed Mater Res. 1992;26:269]. J Biomed Mater Res. 1991;25:1287-1301.
23. DiCarlo EF, Bullough PG. The biologic responses to orthopedic implants and their wear debris. Clin Mater. 1992;9:235-260.
24. El Sharkawy HM, Meffert RM. Biodegradation and Migration of Porous Calcium Phosphate Ceramics [thesis]. New Orleans, La: Louisiana State University School of Dentistry; 1987.
25. Spivak JM, Ricci JL, Blumenthal NC, et al. A new canine model to evaluate the biological response of intramedullary bone to implant materials and surfaces. J Biomed Mater Res. 1990;24:1121-1149.
26. Ricci JL, Blumenthal NC, Spivak JM, et al. Evaluation of a low-temperature calcium phosphate particulate implant material: physical-chemical properties and in vivo bone response. J Oral Maxillofac Surg. 1992;50:969-978.
27. Fang Y, Agrawal DK, Roy DM. Thermal stability of synthetic hydroxyapatite. In: Brown PW, Constantz B, eds. Hydroxyapatite and Related Materials. Boca Raton, Fla: CRC Press; 1994:269-282.
28. Urist MR, Dowell TA. The newly deposited mineral in cartilage and bone matrix. Clin Orthop Relat Res. 1967;50:291-308.
29. Roufosse AH, Landis WJ, Sabine WK, et al. Identification of brushite in newly deposited bone mineral from embryonic chicks. J Ultrastruct Res. 1979;68:235-255.
30. Masters DH. Problem solving in implant dentistry. J Am Dent Assoc. 1990;121:355-358.
31. Corsair A. A clinical evaluation of resorbable hydroxylapatite for the repair of human intra-osseous defects. J Oral Implantol. 1990;16:125-128.
32. Hurzeler MB, Quinones CR, Morrison EC, et al. Treatment of peri-implantitis using guided bone regeneration and bone grafts, alone or in combination, in beagle dogs. Part 1: clinical findings and histologic observations. Int J Oral Maxillofac Implants. 1995;10:474-484.
33. Hurzeler MB, Quinones CR, Schupback P, et al. Treatment of peri-implantitis using guided bone regeneration and bone grafts, alone or in combination, in beagle dogs. Part 2: histologic findings. Int J Oral Maxillofac Implants. 1997;12:168-175.
34. Donohue WB, Mascres C. A comparison of the effects of two hydroxyapatites and a methacrylate resin on bone formation in the rat ilium. Int J Oral Maxillofac Implants. 1993;8:75-82.
35. Ruano R, Jaeger RG, Jaeger MM. Effect of a ceramic and a non-ceramic hydroxyapatite on cell growth and procollagen synthesis of cultured human gingival fibroblasts. J Periodontol. 2000;71:540-545.
36. Wagner JR. A 3 1/2-year clinical evaluation of resorbable hydroxylapatite OsteoGen (HA Resorb) used for sinus lift augmentations in conjunction with the insertion of endosseous implants. J Oral Implantol. 1991;17:152-164.
37. Wagner JR. Clinical and histological case study using resorbable hydroxylapatite for the repair of osseous defects prior to endosseous implant surgery. J Oral Implantol. 1989;15:186-192.
38. Parsons JR. Histology Report. The George L. Schultz Laboratories for Orthopaedic Research, University of Medicine & Dentistry of New Jersey; January 29, 1988. (Included in Wagner JR, Reference No. 37.)
39. Linkow LI, Wagner JR. Management of implant-related problems and infections. J Oral Implantol. 1993;19:321-335.
40. Ganz SD. Restoring the anterior maxillary arch with an implant supported fixed bridge. Implant Soc. 1993;4:2-5.
41. Vlassis JM, Hurzeler MB, Quinones CR. Sinus lift augmentation to facilitate placement of nonsubmerged implants: a clinical and histological report. Pract Periodontics Aesthet Dent. 1993;5:15-23.
42. Vassos DM, Petrik PK. The sinus lift procedure: an alternative to the maxillary subperiosteal implant. Pract Periodontics Aesthet Dent. 1992;4:14-19.
43. Smiler DG, Johnson PW, Lozada JL, et al. Sinus lift grafts and endosseous implants: treatment of the atrophic posterior maxilla. Dent Clin North Am. 1992;36:151-186.
44. Whittaker JM, James RA, Lozada J, et al. Histological response and clinical evaluation of heterograft and allograft materials in the elevation of the maxillary sinus for the preparation of endosteal dental implant sites. Simultaneous sinus elevation and root form implantation: an eight-month autopsy report. J Oral Implantol. 1989;15:141-144.