Osseous regeneration is now an essential part of periodontal therapy. The efficacy of various grafting materials in combination with occlusive membranes (guided tissue generation) has been demonstrated.1-6 The use of barrier membranes is aimed at preventing the down growth of epithelial cells from the surrounding tissues.7 Epithelial cells divide rapidly and will repopulate a wound well before new bone can form. The use of a barrier membrane will impede epithelial cell growth into the wound, hence the expression guided tissue regeneration.
A logical extension of these concepts is the use of resorptive and nonresorptive barrier membranes along with bone-grafting materials to preserve ridge integrity after tooth extraction.8-11 The goal is to prevent the loss of 40% to 60% of ridge height and width commonly seen after extractions12 so as to optimize the implant site and the aesthetic result of the prosthetic rehabilitation. In many clinical situations, replacement of missing teeth with implants has become the standard of care. Ridge preservation after tooth extraction is an essential prerequisite in order to avoid future, more invasive augmentation procedures. These procedures should be considered when an extraction is required and the edentulous ridge may be restored with an implant.
Extraction site grafting is a simple procedure that requires a matrix or scaffolding space-maintaining material placed in the socket, which is then covered by a resorbable membrane (or a calcium sulfate barrier) with 1 or 2 sutures to keep the graft material and membrane in place. This contrasts with ridge augmentation, where a large flap is reflected on both sides of the ridge, graft material is placed, and a membrane is either sutured or tacked into place before the flaps are reapposed. These approaches are differentiated by the terms ridge preservation versus ridge augmentation.
This article discusses the materials and clinical protocol for grafting of an extraction site to promote ridge preservation.
OSSEOUS GRAFTING MATERIALS
A number of different types of bone-grafting materials are available for use, and it is important to clarify certain terms that are used to describe these grafts:
Autogenous grafts refer to the patient being the source of bone for the graft. The patient’s bone contains bone morphogenetic proteins (BMP) that have the ability to stimulate bone formation.13 An alloplastic graft is a synthetic material, ie, ceramic material and hydroxyapatite. Allogeneic grafts are derived from other human sources and are obtained from tissue banks. Xenogeneic grafts are tissues from other species, such as bovine bone, bovine collagen, or porcine-derived enamel matrix proteins (although the latter 2 are not bone-grafting materials).These grafting materials exhibit some specific properties in relation to bone regeneration (Table 1).
Table 1. Types of Osseous Grafting Material.
Graft Material Osteogenic Osteoconductive Osteoinductive
Autogenous yes yes yes Alloplastic no yes varying Allogeneic no yes varying Xenogeneic no yes possible
|
Osteogenic potential: supports the formation of new bone by direct interaction with and stimulation of osteoblasts (bone-forming cells). This phenomenon is based on the contribution of viable cells that are contained in the graft. Autogenous bone can promote osteogenesis, with the new bone being generated from endosteal osteoblasts and marrow stem cells that are contained within the graft material. Using bone harvested from the patient is the most predictable grafting technique available.14
Osteoinductive potential: stimulates progenitor mesenchymal cells to transform into osteoblasts under the influence of stimulating or inductive agents from the bone matrix. Bone allografts and autografts have osteoinductive properties because they contain BMP. Human allograft materials are available commercially.15,16
Osteoconductive potential: supports the formation of new bone by acting as a matrix or scaffolding for extension or apposition of new bone from existing bone. This phenomenon depends on the presence of bone or undifferentiated progenitor cells (precursor cells to osteoblasts). Osteoconductive materials are biocompatible and are typified by alloplasts (synthetic materials), including ceramics and polymers. Xenografts formed from the inorganic bone matrix of animals, usually bovine in origin, are osteoconductive as well. The relatively low cost of many of these synthetic materials makes them very suitable for extraction site grafting.17,18
OCCLUSIVE BARRIERS
Gingival and oral epithelium have one of the highest turnover or regenerative rates of any tissue in the body. The epithelial cells will regenerate much faster than bone-forming cells, will invaginate into a wound, and in the case of an extraction site will prevent or interfere with the osseous recovery or fill. A number of barrier materials have been developed for guided tissue generation to exclude the rapidly dividing epithelium and allow for differentiation and migration of the mesenchymal progenitor cells.
Table 2. Nonresorbable Barriers.
Barrier Material Name of Material Distributor Approximate Cost ePTFE Goretex Gore $151 (15 x 20 mm) PTFE(Teflon) Cytoplast Innova $192 (25 x 30 mm, box of 4) (PTFE) BioBarrier Imtec $32 (17 x 25 mm)
|
Table 3. Resorbable Barriers.
Barrier Material Name of Material Distributor Approximate Cost
• Synthetic polyactic acid polymer Resolut Adapt Gore $135.00 (20 x 15 mm) • Bovine collagen Biomend Zimmer $105.00 (15 x 20 mm) • Bovine collagen Neomem Innova $85.00 (15 x 20 mm) • Synthetic lactic acid polymer BioCellect Imtec $50.00 (15 x 20 mm) • Porcine collagen Bioguide Osteohealth $123.00 (13 x 25 mm) • Calcium sulfate (plaster of Paris) Capset LifeCore $50.00 (1 gm) • CaSulfate putty (plaster of Paris
|
There are nonresorbable barriers (Table 2) that have to be removed at a second-stage surgery. These are usually made of expanded polytetrafluorethylene (Teflon) and were the first occlusive barriers developed.19,20 In addition, a host of biocompatible, resorbable materials can be used over a graft placed into an extraction site.1 These are most commonly derived from bovine collagen. A form of medical-grade calcium sulfate (plaster of Paris) is also available (Table 3).21 It is generally easier to use a resorbable material as a barrier over the graft in extraction sites and thereby avoid a re-entry procedure.
CLINICAL GOAL OF EXTRACTION SITE GRAFTING, MATERIAL SELECTION
A number of studies have investigated the efficacy of various graft materials, with or without the use of an occlusive membrane, to reduce alveolar ridge resorption following tooth ex-traction.22-25 It is generally accepted that the goal in extraction site grafting is simply to provide a matrix or scaffolding to establish the appropriate conditions for new bone formation. Bleeding into the graft material with subsequent clot formation allows for the transformation of the progenitor cells into bone-forming cells, surrounding the graft particles. The inner walls of the extraction socket provide the blood supply and the precursor cells for new bone formation. This occurs during the initial angiogenic stage of regeneration. The granulation tissue in the socket consists of immature blood vessels and fibroblasts that become incorporated into the graft material.26 Over a period of time (usually 4 to 6 months) the biodegradeable graft particles are resorbed, leaving new bone in place.
The most ideal material for osseous grafting is autogenous bone. It has osteogenic, osteoinductive, and osteoconductive potential associated with undifferentiated cells or osteoblasts surviving within the graft material. Bone harvested from the patient is rich in Type I collagen and tissue-derived growth factors, including BMP.27
The selection of the graft material depends, to some extent, on the treatment plan. If the extraction site is to be utilized for implant placement, then the nonresorbable synthetic hydroxyapatite (tricalcium phosphate) is not suitable. Dense, nonresorbable calcium phosphate (HA) is extremely hard and difficult to penetrate with a drill, and although it is not resorbed, it is biocompatible. Therefore, it is most suitable for augmentation or ridge retention under a denture or any site that will not be receiving an implant fixture.28 Synthetic resorbable tricalcium phosphate (HA) is an ideal grafting material. It is cost-effective and provides a source of calcium, and the very small particles have an extremely large surface area, effectively preventing bucco-lingual loss of ridge dimension due to its osteoconductive properties. The particles allow for bleeding into the interparticular spaces, providing a source of precursor cells that will eventually surround each particle with developing bone. Therefore, this material provides a matrix or scaffolding in which the cellular proliferation can take place.29,30 Although both materials are composed of calcium triphosphate, the different conditions under which they are manufactured (varying the amount of heat and pressure or sintering) account for their different properties.31
 |
 |
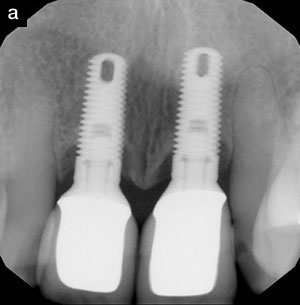
| Figure 1. Failing implant. | Figure 2. Extraction site. |
 |
| Figure 3. Two-year result, using resorbable tricalcium phosphate. Periapical pathology is noted at the apex of the bicuspid tooth. |
 |
 |
| Figure 4. Extraction site showing large radiolucency prior to graft. | Figure 5. Six-month postoperative view at the time of implant placement. |
Figures 1 to 3 illustrate a failed implant that was re-moved; the site was filled with a resorbable tricalcium phosphate graft. This resulted in the dense osseous ridge seen in Figure 3 (2-year result). Note that Figure 3 also demonstrates failing endodontic therapy associated with tooth No. 28. This tooth was eventually removed, the site was grafted, and the edentulous area was treatment-planned for 3 im-plants. Alloplastic (synthetic) materials can also be polymer-based and include layered composites of methacrylates with calcium hydroxide coating (HTR-Polymer)32 as well as bioactive resorbable ceramics. In particular, the ceramics have been used for ridge preservation in extraction sites.33-35 The bioactive ceramic materials have been available for some time and were originally shown to be useful as autograft extenders, that is, having the ability to complement autogenous bone harvested for grafting.36 This may be necessary, since the amount of harvestable autogenous bone is often limited. They have since been shown to have osteoconductive potential and can be used for grafting periodontal defects or extraction sites.37,38
Bioactive glass materials such as Perioglass (Biomaterials) or BioGran (Orthovita) are a form of glass particles upon which a layer of apatite forms, thus promoting bone formation.39 Further, a synthetic graft material that incorporates a 15-amino acid peptide that mimics Type I collagen has been shown to be very effective in enhancing fibroblast and osteoblast binding.40,11 Medical-grade calcium sulfate (plaster of Paris) is another alloplastic material that has been in use for some time as a barrier to achieve guided tissue regeneration. This material has recently been reported as a suitable graft material for extraction sites. It has been shown to be almost completely resorbable, and its use is associated with new trabecular bone formation after 3 months.41
Human allograft (allogeneic) material such as demineralized, freeze-dried bone (DFDBA) has been shown to be an effective material with excellent osteoconductive properties.42 It is relatively inexpensive, is completely replaced by the patient’s bone, and is thus a very good choice for extraction site grafting where an implant will eventually be placed. Freeze-dried bone allograft material (demineralized or nondemineralized) is a useful graft material because of the possible presence of residual BMP.43
Figure 4 shows an extraction site prior to placement of an immediate graft in a case in which a human, freeze-dried, demineralized bone allograft was used. Figure 5 shows the site 6 months later at the time of implant placement. The increased density of the graft site can be seen in an outline corresponding to the original extraction site.
Anorganic bovine-derived material (xenograft) is a good space maintainer for new bone formation because it provides the matrix for osteoconduction. It offers a favorable microscopic architecture, since only the organic portion of the material is removed during preparation. This process leaves the inorganic osseous architecture with channels and spaces for new bone growth, maintaining the physical dimension of the augmentation during remodeling.44,45 The ready availability of xenografts and their safety lend weight to their selection in grafting.
Table 4. Examples of Commonly Used Osseous Grafting Materials.
Class of Material Name Distributor Approximate Cost Per Site
Allograft (human) AlloGro Ceramed $27 to $50 Allograft (human) FDBA DynaGraft putty/gel Salvin $100 Allograft (human) HFDBA RedCross, Pac Coast, MTF $20 to $50 Allograft (human) Grafton DBM Biohorizons $95 Allograft (human) Puros Sulzer $70 to $100 Alloplast (synthetic) Calcitite (HA) Sulzer $75+ hydroxylapatite Alloplast (synthetic) Bioplant HTR Bioplant $40+ Methylmethacrylate polymer Alloplast (synthetic) Bioplant-SSD Bioplant $25+ Methylmethacrylate polymer Alloplast (synthetic) ceramic OsteoGraf Ultimatics $20+ Dentsply/Ceramed, hydroxylapatite Alloplast (synthetic) Capset Lifecore $50 CaS04 Alloplast (synthetic) Perioglass Novabone, Sunstar Butler $49 Bioactive glass Alloplast (synthetic peptide) PepGen P-15 Dentsply/Friadent/Ceramed $130 Synthetic polypeptide Xenograft (bovine) Bio-Ossbovine Osteohealth $45 to $100
|
Table 4 lists many of the osseous grafting materials that are currently available.
CONCLUSION
Immediate extraction site grafting is a simple and straightforward procedure. After the ex-traction, the graft is placed into the debrided socket. There must be some hemorrhage into the site. The blood will clot in and around the graft, and in the presence of progenitor cells bone formation will occur. A resorbable barrier can be placed over the graft, and the area is closed and stabilized with 1 or 2 simple sutures. A number of barriers and/or membranes can be used, including bovine collagen, calcium sulfate, or biodegradable synthetic membranes.
Extraction site grafting often facilitates the best possible functional and aesthetic result. This procedure is frequently indicated where an implant fixture will be placed in the future. Following healing, dense bone often is observed at these grafted extraction sites. These procedures are generally cost-effective, predictable, and not associated with any significant morbidity.
References
1. Paul BF, Mellonig JT, Towle HJ 3rd, et al. Use of a collagen barrier to enhance healing in human periodontal furcation defects. Int J Periodontics Restorative Dent. 1992;12:123-131.
2. Evans GH, Yukna RA, Cambre KM, et al. Clinical regeneration with guided tissue barriers. Curr Opin Periodontol. 1997;4:75-81.
3. Blumenthal N, Steinberg J. The use of collagen membrane barriers in conjunction with combined demineralized bone-collagen gel implants in human infrabony defects. J Periodontol. 1990;61:319-327.
4. Zitzman NU, Naef R, Scharer P. Resorbable versus nonresorbable membranes in combination with Bio-Oss for guided bone regeneration [published correction appears in Int J Oral Maxillofac Implants. 1998;13:576]. Int J Oral Maxillofac Implants. 1997;12:844-852.
5. Wang HL, MacNeil RL. Guided tissue regeneration. Absorbable barriers. Dent Clin North Am. 1998;42:505-522.
6. Reynolds MA, Aichelmann-Reidy ME, Branch-Mays GL, et al. The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontol. 2003;8:227-265.
7. Bunyaratavej P, Wang HL. Collagen membranes: a review. J Periodontol. 2001;72:215-229.
8. Artzi Z, Tal H, Dayan D. Porous bovine bone mineral in healing of human extraction sockets. Part 1: histomorphometric evaluations at 9 months. J Periodontol. 2000;71:1015-1023.
9. Serino G, Biancu S, Iezzi G, et al. Ridge preservation following tooth extraction using a polylactide and polyglycolide sponge as space filler: a clinical and histological study in humans. Clin Oral Implants Res. 2003;14:651-658.
10. Tischler M, Misch CE. Extraction site bone grafting in general dentistry. Review of applications and principles. Dent Today. 2004;23:108-113.
11. MacNeill SR, Cobb CM, Rapley JW, et al. In vivo comparison of synthetic osseous graft materials. A preliminary study. J Clin Periodontol. 1999;26:239-245.
12. Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967;17:21-27.
13. Cochran DL, Wozney JM. Biological mediators for periodontal regeneration. Periodontol 2000. 1999;19:40-58.
14. Narang R, Wells H, Laskin DM. Experimental osteogenesis with demineralized allogeneic bone matrix in extraskeletal sites. J Oral Maxillofac Surg. 1982;40:133-141.
15. Schwartz Z, Mellonig JT, Carnes DL Jr, et al. Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation. J Periodontol. 1996;67:918-926.
16. Becker W, Becker BE, Caffesse R. A comparison of demineralized freeze-dried bone and autologous bone to induce bone formation in human extraction sockets [published correction appears in J Periodontol. 1995;66:309]. J Periodontol. 1994;65:1128-1133.
17. Kent JN, Jarcho M. Ridge augmentation procedures with hydroxylapatite. In: Fonseca RJ, Davis WH, eds. Reconstructive Preprosthetic Oral and Maxillofacial Surgery. 2nd ed. Philadelphia, Pa: WB Saunders; 1995:57-103.
18. Misch CE. Contemporary Implant Dentistry. 2nd ed. St Louis, Mo: Mosby; 1999:451-467.
19. Blumenthal NM. A clinical comparison of collagen membranes with e-PTFE membranes in the treatment of human mandibular class II furcation defects. J Periodontol. 1993;64:925-933.
20. Gottlow J. Guided tissue regeneration using bioresorbable and non-resorbable devices: initial healing and long-term results. J Periodontol. 1993;64(11 suppl):1157-1165.
21. Hoexter DL. Bone regeneration graft materials. J Oral Implantol. 2002;28:290-294.
22. Yukna RA, Castellon P, Saenz-Nasr AM, et al. Evaluation of hard tissue replacement composite graft material as a ridge preservation/augmentation material in conjunction with immediate hydroxyapatite-coated dental implants. J Periodontol. 2003;74:679-686.
23. Guarnieri R, Pecora G, Fini M, et al. Medical grade calcium sulfate hemihydrate in healing of human extraction sockets: clinical and histological observations at 3 months. J Periodontol. 2004;75:902-908.
24. Schopper C, Moser D, Sabbas A, et al. The fluorohydroxyapatite (FHA) FRIOS Algipore is a suitable biomaterial for the reconstruction of severely atrophic human maxillae. Clin Oral Implants Res. 2003;14:743-749.
25. Gross J. Ridge preservation using HTR synthetic bone following tooth extraction. Gen Dent. 1995;43:364-367.
26. Harris RJ. Clinical evaluation of a composite bone graft with a calcium sulfate barrier. J Periodontol. 2004;75:685-692.
27. Schallhorn RG, Hiatt WH, Boyce W. Iliac transplants in periodontal therapy. J Periodontol. 1970;41:566-580.
28. Ohta Y. Comparative changes in microvascular and bone during healing of implant and extraction sites. J Oral Implantol. 1993;19:184-198.
29. Kent JN, Quinn JH, Zide MF. Alveolar ridge augmentation using nonresorbable hydroxylapatite with or without autogenous cancellous bone. J Oral Maxillofac Surg. 1983;41:629-642.
30. Klein CP, Driessen AA, de Groot K. Biodegradation behavior of various calcium phosphate materials in bone tissue. J Biomed Mater Res. 1983;17:769-784.
31. Jarcho M. Biomaterial aspects of calcium phosphates. Properties and applications. Dent Clin North Am. 1986;30:25-47.
32. Froum S, Orlowski W. Ridge preservation utilizing an alloplast prior to implant placement – clinical and histological case reports. Pract Periodontics Aesthet Dent. 2000;12:393-402.
33. Camargo PM, Lekovic V, Weinlaender M, et al. Influence of bioactive glass on changes in alveolar process dimensions after exodontia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:581-586.
34. Lekovic V, Kenney EB, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997;68:563-570.
35. Fetner AE, Hartigan MS, Low SB. Periodontal repair using PerioGlas in nonhuman primates: clinical and histologic observations. Compendium. 1994;15:932-938.
36. Stahl SS, Froum S. Histologic and clinical responses to porous hydroxylapatite implants in human periodontal defects. Three to twelve months postimplantation. J Periodontol. 1987;58:689-695.
37. Norton MR, Wilson J. Dental implants placed in extraction sites implanted with bioactive glass: human histology and clinical outcome. Int J Oral Maxillofac Implants. 2002;17:249-257.
38. Bhatnagar RS, Qian JJ, Gough CA. The role in cell binding of a beta-bend within the triple helical region in collagen alpha 1 (I) chain: structural and biological evidence for conformational tautomerism on fiber surface. J Biomol Struct Dyn. 1997;14:547-560.
39. Wheeler DL, Stokes KE, Hoellrich RG, et al. Effect of bioactive glass particle size on osseous regeneration of cancellous defects. J Biomed Mater Res. 1998;41:527-533.
40. Tonetti MS, Pini-Prato G, Cortellini P. Periodontal regeneration of human intrabony defects. IV. Determinants of healing response. J Periodontol. 1993;64:934-940.
41. Aichelmann-Reidy ME, Heath CD, Reynolds MA. Clinical evaluation of calcium sulfate in combination with demineralized freeze-dried bone allograft for the treatment of human intraosseous defects. J Periodontol. 2004;75:340-347.
42. Rummelhart JM, Mellonig JT, Gray JL, et al. A comparison of freeze-dried bone allograft and demineralized freeze-dried bone allograft in human periodontal osseous defects. J Periodontol. 1989;60:655-663.
43. Mellonig JT, Bowers GM, Cotton WR. Comparison of bone graft materials. Part II. New bone formation with autografts and allografts: a histological evaluation. J Periodontol. 1981;52:297-302.
44. Misch CE, Dietsh F. Bone-grafting materials in implant dentistry. Implant Dent. 1993;2:158-167.
45. Richardson CR, Mellonig JT, Brunsvold MA, et al. Clinical evaluation of Bio-Oss: a bovine-derived xenograft for the treatment of periodontal osseous defects in humans. J Clin Periodontol. 1999;26:421-428.
Dr. Bader practices periodontics and implant dentistry in Concord, Mass. He is a graduate of NYU College of Dentistry, and in 1966 completed a residency in periodontology at the Harvard School of Dental Medicine, where he currently serves as a lecturer in postgraduate periodontology. He is a fellow of the American College of Dentists, International College of Dentists, and American Academy of Osseointegration. He has been published in the Journal of Dental Research, Journal of Periodontology, Journal of Clinical Periodontology, and the American Journal of Dentistry. He can be reached at (978) 369-5066, or visit drbaderimplants.com.
|
Continuing Education Test No. 67.3
|
After reading this article, the individual will learn:
• the rationale and indications for extraction site grafting; and
• the different types of available graft materials and barriers.
1. The technique for guided tissue regeneration was developed because:
a. bone-forming cells need to be “guided”
into place.
b. epithelial cells can invaginate into a
wound.
c. osseous exclusion is necessary for
healing.
d. osteoblasts develop faster than
epithelial cells.
2. The goal of extraction site grafting is to:
a. prevent the loss of ridge height
and width.
b. prevent the adjacent tooth from
migrating.
c. allow the extraction socket to heal more
quickly.
d. prevent alveolar osteoitis (“dry socket”).
3. An alloplastic graft is derived from:
a. the patient’s iliac crest.
b. another individual/human.
c. bovine collagen.
d. synthetic materials.
4. An osteoconductive graft:
a. stimulates new bone-forming cells.
b. contains cells that will differentiate
to produce bone.
c. acts as a matrix for new bone
formation.
d. can be highly antigenic.
5. The first-generation barriers for guided tissue generation were:
a. biodegradable.
b. obtained from porcine sources.
c. pure titanium.
d. expanded polytetrafluorethylene
(Teflon).
6. Biodegradable barriers for guided tissue regeneration may be derived from:
a. rat calvaria.
b. bovine collagen.
c. hydroxyapatite.
d. methyl methacrylate.
7. Extraction site grafting will promote the formation of bone in the socket:
a. in 4 to 6 months.
b. at a much faster rate than nongrafted
sites.
c. within 4 to 6 weeks.
d. at a normal rate, but the new bone will
ha