The literature abounds with studies that address the subject of bone loss following tooth removal. One study reported a 30% to 40% loss of vertical and horizontal dimension within 3 years of tooth loss.1 Other causes of ridge defects include advanced periodontal disease, poor extraction technique, developmental anomalies, accident trauma, or implant failure.2 This sequella presents a challenge to the restorative dentist. How do we aesthetically manage deficient pontic sites with conventional crown and bridge techniques?
This article will revisit a basic augmentation procedure introduced 45 years ago that remains a predictable and efficient option to address this problem.3
|
|
||
|
TYPES OF DEFECTS
The types of defects that can occur after tooth loss were classified by Dr. Seibert back in 1983:
Class I: Buccolingual loss of tissue, with normal ridge height in the apicocoronal dimension.
Class II: Apicocoronal loss of tissue, with normal ridge width in a buccolingual dimension.
Class III: Combination buccolingual and apicocoronal loss of tissue, resulting in loss of normal height and width.4
Over the years several soft tissue augmentation procedures have been developed. The free gingival graft and the subepithelial connective tissue graft have probably received the most attention. This article will illustrate 2 cases that utilized both of these procedures.
Subepithelial Connective Tissue Graft
This procedure was originally conceived by Dr. Langer in the late 1970s. This is the procedure of choice for all of Dr. Seibert’s 3 aforementioned classifications.5 It has several advantages including: versatility, primary closure, dual vascularity, and reduced trauma. One of the advantages of the connective tissue graft is the preservation of color and character of the overlying mucosa.5 Disadvantages include less of an increase of the alveolar ridge height, as compared to the onlay graft. Also, some reduction of keratinized tissue can occur because of a displaced coronally positioned flap to cover the graft.6
Onlay Grafts
These are thick free gingival grafts that can be either partial or total thickness palatal grafts.7 These grafting techniques were developed to address the Seibert Class II defect, the apicocoronal defect. Multiple surgeries are often required when addressing large soft-tissue defects. Onlay grafts can be repeated at 8 to 10 week intervals.2 They have several disadvantages including: they maintain the color of the harvested tissue which is usually pale; they undergo significant post surgical shrinkage; and lastly, they can not be used in areas of previous surgical trauma since they require rapid capillary proliferation.7 It is noteworthy that increasing vertical dimension of a alveolar ridge, as illustrated in the second case study in this article, remains challenging. The patient would be best served with guided bone regeneration techniques (immediate socket grafting) at the time of extraction.2
CASE 1: THE USE OF SUBEPITHELIAL CONNECTIVE TISSUE GRAFT
Diagnosis and Treatment Planning
A 61-year-old female presented at an initial office visit with a history of a 20-year-old partial denture replacing teeth Nos. 7 and 8. She was seeking a “fixed” alternative (Figures 1 and 2).
An exam yielded a negative medical history with no contraindications to dental treatment. Her dentition was intact with the exception of teeth Nos. 7 and 8. She presented with no significant periodontal problems. Gingival color and tone were within normal limits, except for isolated inflammation secondary to the ridgelap pontic design. Her vertical dimension of occlusion (VDO) was significantly collapsed through years of tooth wear and migration.
 |
 |
|
Figure 1. Case 1: Preoperative full-face photo. |
Figure 2. Existing removable partial denture shown in place. |
Several treatment options were reviewed and it was decided that we would treat the patient in 2 stages with the following goals:
- Replacing the lateral and central as a fixed bridge with teeth Nos. 6 and 9 as abutments.
- Improving the aesthetics of both the hard and soft tissue.
- Restoring the lost VDO.
For the purpose of this article we will focus on the treatment of the patient’s deficient edentulous ridge. Since the patient’s defect was primarily of horizontal nature, a connective tissue graft was used (Figure 3).
 |
 |
|
Figure 3. Note the horizontal defect. |
Figure 4. The incision design with connective tissue bed. |
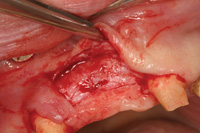
Recipient Site
The recipient site was prepared with a partial thickness dissection. This type of flap is accomplished by using a scalpel to sharply dissect through the gingival lamina propia and the alveolar mucosa. Although technically demanding, the underlying periosteum and connective tissue is critical to preserve and will serve as the bed to which the harvested graft will be sutured initially (Figure 4). A vertical releasing incision was made with a 15c blade (Bard-Parker) 3.0 mm mesial to the cuspid ending with a sulcular incision around No. 9.
Donor Site
 |
 |
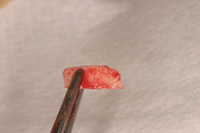
|
Figure 5. The donor site. |
Figure 6. The harvested connective tissue. |
A horizontal incision was made perpendicular to the palate, 3.0 mm below the free gingival margin. A second incision parallel to the long axis of the teeth, approximately 6.0 mm in depth, is made 2.0 mm inferior to the first incision (Figure 5). This incision is 1.5 to 2.0 mm under the outer palatal flap. The underlying connective tissue is then removed down to the palatal osseous and carefully removed (Figure 6). Next, the palatal tissues are sutured back into position. It is recommended that this be done immediately (before suturing the harvested tissue) to reduce the blood clot size and potential tissue necrosis.8 The underlying donor site will fill to its original level at approximately 3 to 4 months.
Graft Stabilization
 |
 |
|
Figure 7. The connective tissue sutured in place. |
Figure 8. Postsurgical site at 3 months. |
 |
 |
|
Figure 9. Close-up of the final prosthesis. |
Figure 10. Case 1: Postoperative smile. |
First, the epithelial “collar” from the first incision is removed. This is done on a sterile tongue blade with a 15C Bard Parker. The harvested tissue is then sutured with resorbable gut utilizing 4.0 chromic gut (Ethicon [Johnson & Johnson]). The split-thickness flap is then sutured over the graft. A periodontal dressing was not utilized in this case (Figure 7).
After 6 weeks, new pontic site concavities can be created with a high-speed diamond (285.5C [PREMIER]) and the provisional can be recontoured. At 12 weeks, final impressions (Impregum Medium Body [3M ESPE]) were taken for the fabrication of the permanent prosthesis in the dental laboratory (Figures 8 to 10).
CASE 2: THE USE OF AN ONLAY GRAFT
Diagnosis and Treatment Planning
A 39-year-old white male presented desiring a more “natural” smile. He noted that the lengths of his anterior teeth were “uneven” (Figure 11). A clinical exam revealed an existing combination case. The patient wore a fixed bridge from the right maxillary cuspid to the left central incisor; replacing the right lateral and central incisors with ridgelap pontics. He also wore a removable partial denture replacing his right and left posterior teeth, with the exception of his left second bicuspid. He had a negative medical history.
 |
 |
|
Figure 11. Case 2: Preoperative full-face photo. |
Figure 12. Existing fixed bridge (teeth Nos. 6 to 10) with ridge-lap pontics. |
 |
 |
|
Figure 13. A vertical defect is observed. |
Figure 14. The recipient site outlined. |
The patient agreed to a treatment plan that would address the deficient edentulous ridge in the area of teeth Nos. 7 and 8 (Figures 12 and 13). This was a Seibert Class II, with 4 to 5 mm compromised vertical component but an adequate horizontal dimension. The patient was informed that this would include multiple surgeries. This treatment would be followed by fixed crown and bridge from teeth Nos. 5 through 11 with a precision partial denture utilizing ERA (Sterngold) attachments.
Recipient Site
The recipient site was outlined 1.0 mm medial to teeth Nos. 6 and 9. It would run apicocoronally, 8.0 mm from the ridge crest (Figure 14). An incision is made 1.0 mm in depth and perpendicular to the tissue in order to create a butt joint for the tissue to be harvested. The butt-joint prevents sloughing of the margins.2 Incisions parallel to the surface epithelium are made. This results in a de-epithialized “bleeding connective tissue bed.” If bleeding is minimal, due to scarring from a prior surgery, additional hemorrhage is encouraged by making a series of cuts into the underlying connection tissue.2
Donor Site
 |
 |
|
Figure 15. The donor area. |
Figure 16. Foil approximating need of the donor tissue. |
 |
 |
|
Figure 17. Foil on donor site. |
Figure 18. Outline of harvested area. |
 |
 |
| Figure 19. Harvested tissue. | Figure 20. Gelfoam placed in donor site. |
 |
 |
| Figure 21. Sutured donor site left to heal by secondary intention. | Figure 22. Retracted view of the final prosthesis. |
 |
| Figure 23. Case 2: Postoperative smile. |
Typically the palatal tissue adjacent to the maxillary molar and premolars is used because substantial tissue can be harvested in this region (Figure 15). Sterile foil is cut to the size and shape of the recipient bed. The foil is then transferred to the palate where a 1.0 mm outline is done. The remaining donor tissue is harvested with 2.0 mm peripheral cuts (the center is significantly deeper [as much as 5.0 mm]) to address the defect (Figures 16 to 19).
Gelfoam (Pharmacia & Upjohn Company) is placed in the concavity and a previously fabricated surgical stent is inserted to protect the wound site (Figure 20). This is made of acrylic with ball clasps from a pre-op surgical model. It is kept in place 48 hours after surgery and for approximately 10 days except for hygiene procedures.
The 4 corners of the graft are sutured with 3.0 Vicryl (Ethicon [Johnson & Johnson]). The remaining graft is sutured every 2.0 mm with 4.0 or 5.0 Vicryl (Figures 21). The goal is to stabilize the graft and provide a “water tight” seal to keep the blood/ serum in the graft. This causes the graft to swell up to 20%.2
The Prosthesis
As previously noted, onlay graft shrinkage is one drawback. It maximizes at 6 weeks following surgery.2 A second procedure utilizing a subepithelial connective tissue graft harvested from the contra lateral side was provided for this patient. (Three months should be allowed for stabilization.) Four months following the graft, final impressions were initiated for the final prosthesis (Figures 22 and 23).
DISCUSSION
A review of recent literature addressing the replacement of missing teeth illustrates an overwhelming dominance of implant related articles. Despite this fact, full-coverage restorations continue to be used as the most common restorative option.9 In fact, it has been the treatment of choice for the past 60 years.2
Treatment of the deficient ridge is more significant in patients with high lip lines. The concept of ridgelap or modified pontics to treat the deficient ridges dates back to the 1930s. This restorative design often led to inflammation of the surrounding tissue. In the author’s experience, motivated patients who desire superior aesthetic outcomes are likely to be dissatisfied with ridgelap pontics as a restorative solution. These patients are often quite willing to have multiple surgical procedures for a final result that yields acceptable aesthetic, phonetic, and self-cleansing advantages.
It is crucial that the restorative dentists treat each deficient ridge with individual consideration. The pretreatment workup should include mounted models, diagnostic wax-ups, and photography to educate the patient regarding the pre-existing condition and to have realistic expectations for any treatment outcome.
CONCLUSION
This article has addressed treatment for the ridge defect, a common restorative dilemma. Clearly the best treatment for our patients is the prevention of bone and soft-tissue deformities by utilizing immediate socket grafting at the time of tooth removal.
Acknowledgement
Dr. Rasner would like to thank the team at Valley DentalArts (Stillwater, Minn), especially Steve Hedquist for the laboratory work of both cases presented.
References
- Single tooth replacement: surgical considerations. In: Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, Mo: Mosby; 2007:742.
- Periodontal plastic surgery. In: Naoshi S. Periodontal Surgery: A Clinical Atlas. Hanover Park, Ill: Quintessence Publishing; 2000.
- Bjorn H. Free Transplantation of Gingival Propria. Odontol Revy. 1963;523:14.
- Cohen ES. Ridge augmentation utilizing the subepithelial connective tissue graft: case reports. Pract Periodontics Aesthet Dent.1994;6:47-53.
- Langer B, Calagna L. The subepithelial connective tissue graft. J Prothet Dent. 1980;44:363-367.
- Breault LG, Shakespeare RC, Fowler EB. Enhanced fixed prosthetics with a connective tissue ridge augmentation. Gen Dent. 1999;47:620.
- Seibert JS. Ridge augmentation to enhance esthetics in fixed prosthetic treatment. Compendium. 1991;12:548-552.
- Langer L. Enhancing cosmetics through regenerative periodontal procedures. Compend Suppl. 1994;18:S699-S705.
- Tarnow DP, Chu SJ, Kim JJ. Aesthetic Restorative Dentistry: Principles and Practice. Mahwah, NJ: Montage Media Corp; 2008:491.
Dr. Rasner received his DMD from the University of Pennsylvania. He earned his MAGD from the Academy of General Dentistry in 1997. Dr. Rasner has owned a private practice in Bridgeton, NJ, since 1980. He has been widely published and has lectured on the topics of implant dentistry and practice management internationally since 1999. He can be reached at (800) 337-8433 or at the Web site realizingthedream.com.
Disclosure: Dr. Rasner reports no conficts of interest.









