Treatment of occlusal enamel loss as it relates to human longevity, attrition, bruxism, and erosion demands closer scrutiny by general dentists. This article reviews factors associated with enamel loss, the effects of enamel loss on occlusion and vertical dimension, and diagnosis and treatment considerations involving enamel loss and the need to re-establish functional occlusion and vertical dimension (FOVD). I define FOVD as the optimal clinical range for which vertical dimension is functionally accepted.
“Normal” occlusion, like all other aspects of human anatomy and physiology, is the continuing result of man’s evolution, and any dental trait (eg, tooth design, jaw shape) that has endured must be considered essentially successful. Paleontologists even use such dental changes to help classify 5- to 6-million-year-old hominids.1 The direct influence of attrition, bruxism, and erosion on occlusion is not a new concept. However, in light of demographic factors and current knowledge, the effects of enamel loss on dental health may need re-evaluation. Water fluoridation, prevention, effective oral hygiene care, and modern periodontal methods are allowing us to maintain our dentitions longer. Although the general consistency of the modern diet has “softened,” and varied environmental factors accelerating enamel loss may not be more notable now than in previous times, enamel wear continues at an accelerated pace.
FACTORS ASSOCIATED WITH ENAMEL LOSS
 |
| Figure 1. |
The average life expectancy in the United States has now risen above the age of 80, with 60 million Americans over the age of 55. Review of US Census data shows that during the 20th century, America’s elderly population has grown at a moderate pace. But not too far into the future, that growth will become rapid. So rapid, in fact, that by the middle of the next century, the Census Bureau projects the US elderly population (over 65) will double, reaching 80 million by the year 20502 (www.census.gov/population.) With so many elderly people keeping their own teeth, this extended normal wear is pushing teeth and supporting structures to their natural limit and beyond.
Many of today’s dental patients present with work-related or home-related stress-generated bruxism. In addition, fingernail biting, pen chewing, or other deleterious habits are common ways of stress mitigation and can cause attrition of enamel. Other patients frequently indulge in caffeine and nicotine, often near bedtime, thus increasing the possibility of nocturnal bruxism. Subconscious dental damage is incurred as a result of clenching and/or bruxing during strenuous fitness activities. Though not always clearly noted as a side effect, dental damage can result from the use of bodybuilding supplements, endurance or mood-elevating drugs, and/or various other pharmaceuticals.3-5
An oral health study of 1,000 females and 1,000 males between the ages of 35 and 44 completed by researchers in the province of Quebec, Canada, concluded that one out of five people are bruxers. Bruxism related tooth wear has been reported even in children.6 Studies have also shown that bruxers and clenchers produce 6 times the bite strength7 of nonbruxers, and are therefore capable of greater damaging occlusal forces than nonbruxers. Clinically, simple tactile manipulation of the masseter and temporalis muscles can easily verify this strength.
The physiologic relationship between enamel loss, occlusion, and systemic sequellae may be complex. Nevertheless, extensive current research supports more direct associations between oral health and general health.8-10 Other studies have correlated a functional relationship between maxillo-mandibular enamel loss and a decreased “isometric strength” throughout the body.11 Enamel erosion also promotes oral inflammation and can increase the mesial-distal and inter-occlusal spaces between teeth. Coffee, certain wines, and most popular soft drinks lower salivary pH levels, further eroding enamel. Furthermore, enamel erosion may be significant as a result of bulimia and other gastric-related illnesses. Even the excess of otherwise healthy dietary habits such as eating citric fruits can be very damaging. Avid swimmers may present with erosion caused by frequent chlorine exposure. Specific patterns of enamel erosion may go undetected for years.
Whatever the causes, when specific patterns of accelerated enamel loss are pronounced, resulting symptoms may not only include chronic tooth sensitivity, but the excessive loss of vertical dimension may also impair mastication. Direct enamel loss and nutritional deficiency correlations are less well defined, but extensive loss of vertical dimension may promote oral inflammation and oral disease.12
It remains the dental professionals’ responsibility to familiarize themselves and their patients with the varied factors associated with enamel loss through recognition and clear, candid communication.
DIAGNOSIS AND EVALUATION OF ENAMEL LOSS
The success of any dental treatment is dependent not only on proper treatment technique but on thorough initial examination with careful evaluation and proper diagnosis. When evaluating enamel loss, it should be noted that some degree of gradual enamel reduction over the course of a lifetime may be of no clinical concern. However, accelerated or excessive reduction of enamel requires treatment intervention. Fortunately, preventive options, improved dental materials for more conservative restorations, and a more realistic outlook on occlusion and vertical dimension have all served to broaden our potential in the treatment of this ever-expanding problem. Nevertheless, not all patients with a degree of vertical dimension loss require its functional treatment. Each individual patient’s lifestyle and habits need to be recognized and reviewed on a timely basis in the light of our current treatment possibilities and the now-available scientific implications.
Patients of all age groups are more aesthetically aware, and society’s continued preoccupation with youth and beauty intensifies this awareness. Changes in adult “face height” have long been associated with tooth wear and tooth loss.13 This subtler “mid-face collapse” is one of the factors now clearly associated with the face appearing older prematurely,14 even outside the realm of full denture preparation. In the past, aesthetic alternatives for older adults have been somewhat restricted, but today there are many aesthetic treatment options available to patients of all ages. From a functional perspective, negative physiologic effects of the reduction of ideal facial contour because of tooth wear and tooth loss are becoming more commonly recognized. Ethical concerns of creating “ideal beauty” not withstanding, the prevalence of greater vertical dimensional loss through attrition, bruxism, and erosion must also be addressed functionally.
MULTIDIMENSIONAL TREATMENT CONSIDERATIONS
 |
| Figure 2. |
Severe bruxism and attrition are easy to detect. Diagnosing their cause and selecting appropriate treatment recommendations are often more exacting. Various relaxation techniques and much more liberal preventive or arrestive use of supervised occlusal guard or bruxism-reducing appliance therapy should be presented as effective, well-supervised, primary treatment modalities. Furthermore, many practitioners consider splint wear mandatory prior to extensive restorative therapy. A number of successful techniques and materials for guard fabrication have been described in the literature.15
Oral-maxillofacial surgeons who perform orthognathic surgery, as well as orthodontists, well recognize general improvements brought about by changes in vertical dimension.16 Both specialties have long been comfortable making significant or instantaneous changes in vertical dimension.17 While the mathematical quantification of ideal beauty in facial proportion has existed since ancient times,18 its biological significance has also often been proposed in the literature.19
Often, the appropriate treatment approach for loss of vertical dimension is not orthognathic nor primarily orthodontic, and a general dental restorative treatment is advisable. However, such correction often does require a more elaborate treatment effort. The importance and acceptance of even slight restorative correction of vertical dimension loss by the generalist have remained somewhat guarded. The ethical-legal implications of any such corrective approach can only be evaluated in relation to the ethical-legal implication of its disregard. In determining proper restorative treatment with the goal of achieving clinically acceptable FOVD, the time may have come for a more progressive view that incorporates scientific guidelines common to all disciplines.17
While the physiologic benefits of a well-functioning dentition are unquestionable, the actual determination of when a restorative intervention for lost occlusal vertical dimension is functionally indicated may remain a matter of some debate. The adaptive capabilities of the human dentition are complex. Parameters for diagnosis and treatment planning of oral disease are usually multifaceted, and this certainly holds true for lost occlusal vertical dimension. Recognizing moderate resulting changes in facial proportions and labial over-closure are challenging. Quantification of cheek convexity, lip compression, and infralabial fold depth may be somewhat subjective. Even anatomic dental changes from occlusal enamel reduction can range from subtle to pronounced. However, some more explicit parameters for determining FOVD intervention are very readily apparent.
Clinically and radiographically, excessive occlusal enamel loss and its associated dentinal exposure are clearly visible. Generalized posterior dimensional loss can aggravate or be the primary cause of a periodontally traumatic deep anterior bite. Proximal or direct lower-anterior impingement on the anterior palate and/or upper-anterior impingement on the lower buccal gingiva must be viewed from a FOVD perspective. The deleterious periodontal results of traumatic excursive motion can likewise be well ascertained. Lost cuspid guidance can be confirmed and documented. Additionally, the loss of proper mesial-distal contacts and/or crown-emergence-profiles, with associated periodontal deterioration, is often associated with vertical dimensional loss from erosion. Musculoskeletal parameters have also been examined.20,21 Further research supporting these clinical findings as well as related nutritional correlations for FOVD identification and treatment planning should continue.
TREATMENT PLANNING
 |
| Figure 3. |
A definite and exact determination of a decisive, optimal vertical dimension may be obscure; absolute scientific support for any single technique in the reestablishment of FOVD may be lacking. Nevertheless, clinicians make valid, quantitative, working evaluations. Techniques that combine centric relation, anterior guidance, and facially-generated analysis have often been presented.16,17 Understanding the effects of vertical dimensional change on facial contour remains a primary requirement for proper treatment planning. Anticipating the various effects of vertical dimension change on condylar rotation or possible consequences on midline alignment, as well as its effect on nasion-to-menton facial contour, is essential.
Along with a mid-face collapse, one of the earliest clinical signs of excessive bruxism and attrition is loss of functional “cuspid guidance.”22 This loss has extensive implications far beyond “smile-line” anterior aesthetics. With historical and evolutionary argument, some clinicians tend towards “flatter plane” restorative occlusal parameters for resolving modern-day dental pathology.23 Many other practitioners advocate re-establishment of cuspid guidance along with group function as beneficial.24 Especially in light of increased human longevity, shallow rather than deep cuspal anatomy certainly has less of an ongoing traumatic potential. Undeniably, the premature or excessive loss of vertical dimension and/or cuspid guidance aggravates generalized periodontal occlusal trauma and facilitates chipping of anterior teeth.
Cuspids, with their higher pressure sensitivity and stereotactility, provide an important protective mechanism against traumatic forces.25,26 Because of cuspid strength and position, some degree of even mild cuspid guidance furnishes protection for the upper and lower central and lateral incisors both coronally and periodontally. Thus, even shallow cuspid protection with a properly restored cross-arch stability functionally benefits the bicuspids and also the molars.
Pretreatment oral and facial photographs are highly recommended. Full-arch pretreatment diagnostic casts are necessary. Often, periodontal, orthodontic, and orthognathic consultations will be advised. Limited orthodontic arch expansions with minor tooth movement, or even complete orthodontics, are adjunct preliminary treatment options that must also be carefully evaluated. In order to properly evaluate proposed treatment, hinge-axis centric location is verified on mounted study models using an adjustable, semi-adjustable, or polycentric model-mounting device.27 A diagnostic wax-up will assist in confirming patient aesthetic acceptance and anticipate proper future functionality. Using aids such as the Lorin Library of tooth design (digident.com) can assist with patient anterior smile-design selection.
Experience and an understanding of the various centric determinants will provide predictable neuromuscular occlusion or repeatable bimanual centric relation. A combination of the recognized functional techniques will result in the establishment of a physiologic, clinically acceptable vertical dimension in most patients.28-30 Regardless of technique used, conservative, pain-free, functional occlusion is the goal.
When dealing with TMD, many studies do suggest that some degree of cuspid guidance along with group function is advantageous in treatment and prevention.24 Conversely, such an etiologic relationship between vertical dimension change and TMD has not been well established.31 Nevertheless, any actual TMJ treatment will certainly require a specialist. Effectively “opening the bite” seldom causes discomfort and may relieve a pre-existing TMJ symptom by bringing the condyle downward, away from retrodiscal tissues.32 Even when a TMD is not present, prudence dictates very thorough pretreatment documentation, with thorough recording of relevant pretreatment parameters, including range of motion and any pre-existing patient discomfort.
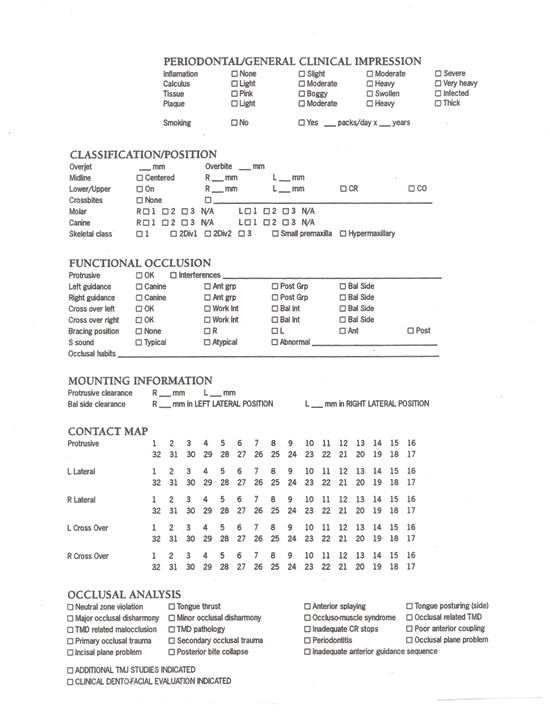
A well-designed, written occlusal evaluation form should be employed (Figures 1 through 3). Similar forms can be used singly or in combination.
Any type of written prior and post-treatment occlusal evaluation provides more due diligence than is now performed by many general dentists or even specialists.
Before initiating therapy, patients should have a basic understanding of the importance of multiquadrant, anterior, and posterior functional interrelation in a complete dentition. At the practitioner’s discretion, well-designed informed consent forms, while unable to afford complete protection, will serve to document risks and benefits of either elected treatment or nontreatment.33
Such a treatment planning process can also allow for the evaluation and final achievement of protective, bilateral, occlusal load function. For best results, along with equal bilateral force loading, proper TMJ support requires maintaining or sometimes re-establishing optimum midline. Functionally as well as periodontally, corrective restoration may further benefit from anterior or full-arch splinting.
CURRENT RESTORATIVE TREATMENT OPTIONS AND PRINCIPLES
In the very near future, a greatly increasing number of healthy and concerned patients will expect and request more enduring dentistry to meet their changing needs. By appropriately challenging absolute third-party exclusions that prevent insurance benefit for any restoration of lost occlusal dimension, the dental profession must now reaffirm its mandate to provide patients with more comprehensive preventive and appropriately durable treatments than ever before.
Present-day treatment plan options often include composite bonding and all-metal, PFM, and all-porcelain restoratives. Ibsen and Xin-Yi described the limited, relatively noninvasive use of bonded porcelain for reestablishing cuspid guidance34 when such treatment is provided at the proper time, before extensive loss of cuspid guidance. If additional anterior occlusal dimensional increase is indicated, palatal coverage, particularly of maxillary cuspids, along with porcelain coverage to include the full labial surface of mandibular cuspids, can also be performed. New pressable ceramic materials and low-abrasion “biocompatible” porcelains such as low-fusing “hydrothermals” built over gold-alloy metals or using various porcelain-core-based techniques can facilitate incorporating a more incremental, single-arch restorative treatment approach.35 Supragingival coverage is often possible and can help limit periodontal tissue involvement. Indirect technique glass fiber-reinforced resin composites can also now offer a durable, biocompatible full-mouth restorative alternative to metal-substrate and all-porcelains.
Conscientious evaluation of fixed or removable prosthetic changes in the posterior segments’ vertical support should be made prior to, and in conjunction with, any proposed treatment of anterior teeth. Patients may have become accustomed to their long-term, reduced vertical dimension. Any determined amount of proposed vertical dimension change should be tempered by the patient’s individual functional and aesthetic needs. Patients’ complete involvement in the selection, progress, and verification of their adaptability to the resulting treatment changes is essential for success.
Substantial increase in vertical dimension is possible and may be well tolerated. However, increased vertical dimension is not always necessary for clinical success, and even with very limited tooth preparation or a very minor change in vertical dimension, improved function and aesthetics can still be achieved.36,37 As a result of the natural anatomic condylar rotation, even very slight restored adjustment of vertical dimension in the mid-posterior segment (<0.5 mm) provides a more significant and often advantageous rotational and dimensional improvement when measured anteriorly. This anatomical, geometrically based rule of a “3-to-1” anterior-to-posterior vertical dimension change-ratio should be very prudently observed.
Established principles for mid-line alignment, mandibular flexure, balanced occlusal table with equal bilateral loading, sensible crown-to-root ratios, and sufficient bone support in periodontal force distribution must be respected during any proposed restorative treatment. Some limited equilibration of any balancing interference may be required.38,39 Standard confirmation of centric and lateral excursive relations and liberal use of a post-preparation desensitizing agent with judicious supervision and confirmation of patient acceptance before the restorative finalization is paramount.
A very carefully monitored, well-managed, limited (4- to 6-weeks), “conservative” bite plate appliance therapy40 such as an anterior guided orthosis is often used. If needed, an extended period (8 to 10 weeks or longer) of fixed acrylic provisionalization of proposed corrective occlusal changes is indicated to further avoid problems such as temporal tendonitis and actual or iatrogenically perceived dental stress, with its various associated documented or undocumented complaints.41,42
At this juncture, some form of final confirmation of patient acceptance of occlusal changes, with a signature in the chart or on a form, is therefore recommended.
Previously, some hesitation has existed among many general dentists to address the troublesome issue of alteration of lost vertical dimension, and certain myths43,44 or misconceptions have persisted. Many dental insurance companies have shrewdly inserted “attrition” exclusions hidden in contract language alongside “cosmetic” and “nontraumatic” exclusions. (The Guardian: 04/7/99 and Blue Cross & Blue Shield 07/22/98) (Figure 3). Though interrelated, ideal beauty and ideal function are not synonymous when dealing with occlusion. Many companies even deny the arrestive use of bruxism guards through similar, overly expansive device exclusions and limitations. Thorough evaluation of current scientific documentation and present and future functional needs of the general patient population demand a more flexible reimbursement environment.
Correction of vertical dimension loss from attrition and bruxism should still be guided by a prognostic desire for natural tooth preservation. Any tendency toward excessive, purely cosmetic overtreatment should be very carefully evaluated or ethically discouraged. Future research may better address additional, more specific, relevant treatment parameters.
Continued post-treatment hygiene care is required, and ease of care is important. Especially in the elderly population, dexterity, mot
ivational, or other patient restrictions should be considered in any case design. Finally, concurrent, post-treatment evaluation of related lifestyle factors should be reviewed in order to identify any continuing, dentally harmful behavioral factors.
SUMMARY
Much of the accelerated or premature loss of vertical dimension experienced by patients is certainly preventable, and prevention should be emphasized. Recommendations on limiting any nicotine and caffeine use, supporting needs for fitness efforts, and assisted or self-management of damaging habits from stress are vital. Restoratively along with aesthetics, substantial, functional vertical dimension changes may now be addressed conservatively, using a range of strategies and current state-of-the-art materials.
Patients should become better informed about the importance of a good dentition for their better general health. Restorative alteration of vertical dimension may not be universally essential. Nevertheless, the profession, patients, and the third-party payment community must unequivocally recognize the physiologic advantage of restoring lost FOVD.
The simple replacement of missing or damaged teeth without also reviewing and often addressing related facial proportions, occlusion, and vertical dimension concerns can be too limited a treatment option. Treatment of this current and ever-increasing condition cannot be sparingly restricted to the realm of specialists. In light of current population demographics, general dentists must inform themselves of extensive, currently available information in order to improve their proficiency and gain more confidence in addressing these multifaceted, ever more common problems.
Examining all treatment variables in conjunction with the proficient determinationfor improved masticatory function and durability will increase our potential for achieving more favorable outcomes. New research in these areas will continue to be applied in order to optimally compose and implement modern comprehensive treatment plans and better evaluate post-treatment success.
Not taking the interrelated issues discussed in this article into consideration, or a failure to assess and better engage these increasingly widespread needs of our population, could severely compromise the dental health of an increasing number of current and future patients.
References
1. Neiburger EJ. The evolution of human occlusion: ancient clinical tips for modern dentists. Gen Dent. 2002;Jan:44-49.
2. US Census Bureau: Economics and Statistics Administration, US Department of Commerce, May 1995.
3. River L , Saugy M, Mangin P. Principal doping substances and their side effects: a compilation prepared for the International Cycling Union. Compilation Report, International Cycling Union. 2001 April:3-4.
4. Wadler G-I, Hainline B. L’athlète et le dopage, drogues, et mèdicaments (The Athlete and Doping, Drugs, and Medication). Collection Sport et enseignement, Editions. Vigot, Paris; 1993.
5. Pallasch TJ, Joseph CE. Oral manifestations of drug abuse. J Psycho Drugs. 1987;19:275-377.
6- Schneider PE, Peterson J. Oral habits: considerations in management. Pediatr Clin North Amer. 1982;29:523-546.
7. Gibbs CH, Mahan PE, Mauderli A, et al. Limits of human bite strength. J Prosthet Dent. 1986;56:226-229.
8. Johnson-Leong C, Patel G, Messieha Z. The relation between coronary artery disease and periodontal disease. Dentistry Today. 2003; Feb:99-105.
9. Wu T, Trevisan M, Genco RJ, et al. Periodontal disease and the risk of cerebrovascular disease. Arch Intern Med. 2000;160:2749-2755.
10. Douglass C, Periodontal disease and stroke. Colgate Oral Care Report. 2001;11:4.
11. Abduljabbar T, Mehta NR. Effect on isometric strength of vertical dimension loss in TMD patients. J Craniomandib Practice. 1997;15:57-66.
12. Enwonwu CO, Phillips RS, Falkler WA Jr. Nutrition and oral infectious diseases: state of science. Compendium. 2002;23:431-446.
13. Tallgren A. Changes in adult face height due to aging, wear and loss of teeth and prosthetic treatment. Acta Odontol Scand Suppl. 1957;24:1-24.
14. Schlott WJ. Midface collapse: an overlooked disease. Dent Today. 1997;16:54-57.
15. Dylina TJ. The basics of occlusal splint therapy. Dent Today. 2002;15: 82-87.
16. Mack MR. Facially generated occlusal vertical dimension. Compend Contin Ed Dent. 1997;18:1183-1194.
17. Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Ed Dent. 1997;18:1169-1177.
18. Richetts RM. The biological significance of the divine proportion and Fabonacci series. Amer J Orthod. 1982;81:357-370.
19. Mack MR. Vertical dimension: a dynamic concept based on facial form and oropharyngeal function. J Prosthet Dent. 1991;66:478-485.
20. Manns A, Mirrales R, Palazzi C. EMG, bite force, and elongation of masseter muscle under isometric voluntary contractions of vertical dimension. J Prosthet Dent. 1979;42:674-679.
21. Prombonas A, Vlissidis D, Molyvdas P. The effect of altering the vertical dimension of occlusion on biting force. J Prosthet Dent. 1994;71:139-143.
22. D’Amico A. The canine teeth. J South Calif Dent Assoc. 1958;26:6-22,49-60,127-142.
23. Turner KA, Missirlian DM. Restoration of the extremely worn dentition. J Prosthet Dent. 1984;52:467-474.
24. Manns A, Chan C, Miralles R. Influence of group function and canine guidance on electromyographic activity of elevator muscles. J Prosthet Dent. 1987;57:494-501.
25. Weinberg L. The prevalence of tooth contact in eccentric movements of the jaw: its clinical implications. J Am Dent Assoc. 1961;44:401-403.
26. Schuyler C. Factors contributing to traumatic occlusion. J Prosthet Dent. 1961;11:707-709.
27. Pitel ML. Clinical management of a worn dentition with a new polycentric occlusal system. Dent Today. 2000;19:42-51.
28. D’Amico A. The canine teeth: normal functional relation of the natural teeth and man. J South CA Dent Assoc. 1958;261:197-199.
29. Rivera-Morales WC, Goldman BM. Are speech-based techniques for determination of occlusal vertical dimension reliable? Compend Contin Ed Dent. 1997;18:1214-1223.
30. Stewart B. Restoration of the severely worn dentition using a systemized approach for a predictable prognosis. Int J Perio Restor Dent. 1998;18:47-57.
31. Manns A, Moralles R, Guerrero F. The changes in electrical activity of postural muscles of the mandible upon varying the vertical dimension. J Prosthet Dent. 1987;11:493-495.
32. Dylina TJ. Choosing a starting point for restorative dentistry. Dent Today. 2000; Sept:100.
33. Ahlin JH. Informed consent. Cranio Clin Int. 1991;1:207-210.
34. Ibsen RL, Yu XY. Establishing cuspid-guided occlusion with bonded porcelain. J Esthet Dent. 1989;1:80-85.
35. Catena F, Goldstein C. Esthetic success with low-wear ceramics. Contemp Esthet Restor Pract. 2000;3:20-25.
36. Jackson RD. Loss of cuspid guidance: a functional and aesthetic dilemma. Dent Today. 2000;19:56-61.
37. Wynne WPD. Terminal wear syndrome. Contemp Esthet Restor Pract. 1999;10:52-60.
38. LeGall MG, Lauret JF. Function of mastication: implications for occlusal therapy. Pract Perio Aesthet Dent. 1997;10:225-229.
39. Schlott WJ. Occlusion and dental disease. Dent Today. 1999;18:72-77.
40. Widmalm SE. Use and abuse of splints. Compend Contin Ed Dent. 1999;20:252,256-258.
41. Bledsoe WS Jr. Selection, application and management of phase I orthotics. Cranio Clin Int. 1991;1:13-58.
42. Brown CR, Shankland W: Pain management temporal tendonitis. J Perio Esthet Dent. 1996;8:418.
43. Thompson JR. The rest position of the mandible and its significance to dental science. J Am Dent Assoc. 1946;33:151-180.
44. Schlott WJ. Dental mythology and trends for the millennium. Dent Today<


