Accidents are daily occurrences; however, problems often occur that are iatrogenic in nature and result because of misinformation or the lack of information. Periodontal disease, which often proceeds in silence, very often in its stealth masks the underlying destruction of the periodontium. When the disease advances beyond the corrective talents of the primary clinician and/or the periodontist, then the only recourse is extraction.
Current concepts in periodontology and restorative and rehabilitative dentistry give today’s dentist a plethora of options for the replacement of one or more teeth. While many treatment alternatives are available, such as implants, removable partial dentures, etched-metal bridges, resin-bonded bridges, and traditional ceramo-metal bridges, time and costs are the usual factors that influence the patient’s choice of treatment.
This article presents a case in which an improved technique for localized ridge augmentation was used to treat a challenging periodontal and aesthetic problem.
CASE STUDY
 |
 |
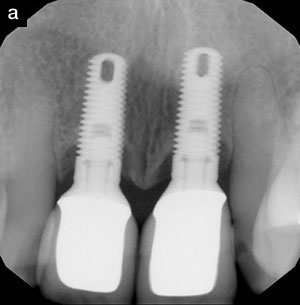
| Figure 1. The patient was a 30-year-old male in excellent health. | Figure 2. Radiographs reveal the extent of bone loss associated with tooth No. 9. |
 |
| Figure 3. Tooth No. 9 is almost completely denuded. |
 |
 |
| Figures 4 and 5. Tooth No. 9 was extracted, resulting in an alveolar ridge defect. |
The patient was a 30-year-old male in excellent health (Figure 1) who was referred by a friend. He recalled being struck accidentally in the mouth during a social function, and regarded this event as the etiology of his “loose” front tooth (Figure 2). Tooth No. 9 was nearly completely denuded (Figure 3) with the exception of a very small lingual soft tissue attachment. Tooth No. 9 was extracted, resulting in an alveolar ridge defect (Figures 4 and 5). The discontinuation of the cortical plate was complete due to a prior chronic infectious process.
TREATMENT PLANNING
 |
| Figure 6. A “flipper” partial is placed immediately following extraction of tooth No. 9. |
The treatment plan consisted of tissue regeneration and augmentation, a fixed partial denture spanning abutments Nos. 8 thru 10, and an indirect restoration for tooth No. 7. A flipper partial approximating the incisal plane and temporarily replicating the previous tissue volume of tooth No. 9 was placed immediately after the disarticulation of tooth No. 9 (Figure 6). The infectious process, attachment loss, and removal of tooth No. 9 had resulted in the formation of a Seibert class III ridge defect. The augmentation technique used in this case is an amalgamation of two different techniques. The incision and flap design were an adaptation of the technique described by Garber and Rosenberg.1 The ridge augmentation technique employed was a modification of a technique using an alloplast graft material described by Allen and co-workers.2
PREPARATION
Soft Tissue
The importance of preserving gingival and osseous tissue in this type of case has been well documented in the literature. The paramount concerns during this stage are dental morphology, embrasure form, gingival and osseous anatomical form, and resulting osseous and gingival health.
 |
 |
| Figure 7. A full-thickness envelope flap is created. | Figure 8. BIOGRAIN synthetic bone graft material is delivered into the distended envelope flap. |
After administering local anesthesia, an arcuate horizontal incision using a 15c scalpel blade in a No. 5 blade handle was made at the crest of the edentulous ridge. A full-thickness envelope flap was created by sharp dissection to the bony crest of the residual ridge and then blunt dissection over the facial aspect of the ridge deformity in a latero-apical direction (Figure 7). A synthetic bone graft material (BIOGRAIN, Corthovita) was utilized. This syringeable bioactive glass product was selected for its affinity for both osseous and gingival tissues, and was delivered into the distended envelope flap (Figure 8).
 |
 |
| Figure 9. Connective tissue is obtained from the left palatal area. | Figure 10. The connective tissue graft is harvested. |
 |
 |
| Figure 11. The flaps are repositioned with suture material, along with hemostatic control. | Figure 12. Occlusal view of the surgical site immediately after surgery. |
 |
 |
| Figure 13. Facial view of surgical site at 14 days. | Figure 14. Occlusal view at 14 days. |
 |
| Figure 15. Donor site at 14 days. |
The soft tissue portion of the surgery involved obtaining connective tissue from the left palatal area (Figure 9). The connective tissue graft was harvested (Figure 10). The donor tissue was prepared in a laminar fashion, then carefully teased into place. The flaps were then repositioned with 5-0 gut suture material along with hemostatic control (Figure 11). Following hemostasis, the interim prosthesis was modified and reinserted. The palatal donor area healed rapidly and uneventfully (Figures 12 through 15). The 1-month surgical follow-up appointment revealed a successful hard and soft tissue augmentation result.
Tooth Structure
Abutments Nos. 8 and 10 were prepared after 60 days of healing. An ovate pontic site partially developed by the flipper partial was modified and refined for the final prosthesis. Diamond burs were used to develop adequate incisal reduction, shoulder widths, and lingual, axial, and labial reduction. Preparations were then smoothed with Arkansas stone burs. Tooth No. 7 was then prepared to receive an indirect veneer. Depth guides were placed and blended. The gingival, proximal, and incisal aspects of No. 7 were then conjoined. The entire preparation was then planed with sandpaper discs and an Arkansas bur.
LABORATORY INSTRUCTIONS
 |
 |
| Figure 16. A depiction of provisional morphology. | Figure 17. Provisional restorations are fabricated for tooth No. 7 and Nos. 8 through 10. |
Thirty-five millimeter preoperative slides and prints, a stick bite registration, a very detailed color map, shade selection using the Vitapan 3-D Master shade guide (Vita), preoperative models, and a meticulous laboratory prescription were forwarded to the laboratory technician. A provisional was fabricated for No. 7 and abutments Nos. 8 thru 10 (Figures 16 and 17) with Pro-Temp (3M ESPE) using the original preoperative impression. The provisionals were luted with Temp-Bond NE (Kerr), and the excess was removed without insult to the soft tissues.
PLACEMENT AND CEMENTATION
The provisionals were removed and the abutments were cleaned with Concepsis scrub (Ultradent). The bridge was then tried in with Fit Checker (GC Corporation), and ultimately tooth No. 8 had to be readjusted with a reduction coping. Once the bridge was seated, the pontic site was evaluated for blanching. No blanching was observed. Both mesial and distal contacts were very tight, suggesting an adjustment. Hi-Site (Ultradent) was applied proximally to indicate tight contacts. The “binding” areas were relieved, then polished with Dialite (Brasseler) porcelain polishers. The bridge was then luted with Rely X (3M ESPE) cement, and the residue was removed with a No. 12 (Bard-Parker) blade.
 |
 |
 |
| Figures 18, 19, and 20. The final restorations are an aesthetic and functional success. |
The veneer was tried on No. 7. The fit was confirmed, and the appropriate cement shade was selected. The veneered surface was cleaned with Concepsis scrub (Ultradent). The veneer was then silanated with Porcelain Primer (Bisco) for 60 seconds. The labial surface was then saturated with Optibond Solo (Kerr), then light cured for 20 seconds. The indirect restoration was then bonded with Insure Lite (Cosmedent), and cured for a total of 2 minutes. Excessive luting cement was removed, contacts were flossed, and the occlusion was evaluated for eccentric contacts in all border movements (Figures 18 through 20).
CONCLUSION
Today’s clinicians have the fortuitous advantage of having at their disposal myriad restorative materials and techniques to restore, enhance, and preserve both soft and hard dental tissues. The clinical dilemma faced with this particular case was to reconstruct a partially edentulous deformed alveolar ridge. The different techniques that comprise this subdiscipline in periodontics play a fundamental role in modern “peri-prosthetic” treatment.
This treatment zone was effectively restored with ridge augmentation and significantly enhanced with an indirect porcelain veneer and a ceramo-metal fixed partial denture. Proper communication regarding adequate home care and timely hygiene visits will help preserve the longevity of this treatment.
Acknowledgment
The author would like to thank periodontist Richard Young, DDS, MS, Des Moines, Iowa, and John Haupt, MDT, Haupt Dental Lab, Brea, California, for their valuable assistance in helping to make this case a success.
References
1. Garber DA, Rosenberg ES. The edentulous ridge in fixed prothodontics. Compend Contin Educ Dent. 1981;2:212-223.
2. Allen PE, Gainza AC, Farthing GG, et al. Improved technique for localized ridge augmentation: a report of 21 cases. J Periodontol. 1985;56:187-199.
Suggested Reading
Abrams L. Augmentation of the deformed residual edentulous ridge for fixed prosthesis. Compend Continu Educ Dent. 1980;1:205-213.
Chiche GJ. Esthetics of Anterior Fixed Prosthodontics. Chicago, Ill: Quintessence Books; 1994:75-96.
Johnson K. A study of the dimensional changes occuring in the maxilla following tooth extraction. Aust Dent J. 1969;14:241-244.
Kaldahl WB, Tussing GJ, Wentz FM, et al. Achieving an esthetic appearance with a fixed prosthesis by submucosal grafts. J Am Dent Assoc. 1982;104:449-452.
Langer B, Calagna L. The subepithelial connective tissue graft. A new approach to the enhancement of anterior cosmetics. Int J Periodontics Restorative Dent. 1982;2:22-33.
Meltzer JA. Edentulous area tissue graft correction of an esthetic defect: a case report. J Perodontol. 1979;50:320-322.
Olsen GM. Replacement of the maxillary left central incisor with an InCeram bridge. AACD J. 1997;Fall:20-28.
Rekovic V, Kenney EB, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction: report of 10 cases. J Periodontol. 1985;56:187-199.
Shillingburg HT. Fundamentals of Fixed Prosthodontics. Chicago, Ill: Quintessence Books; 1978:13-67.
Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts: Part 1, technique and wound healing. Compend Contin Educ Dent. 1983;4:437-453.
Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts: Part 2, prosthetic/periodontal interrelationships. Compend Contin Educ Dent. 1983;1:205-213.
Siebert JS. Reconstruction of the partial edentulous ridge; gateway to improved prosthetics and superior aesthetics. Prac Periodontics Aesthet Dent. 1993;S(5):47-55.
Smidt A, Goldstein M. Augmentation of a deformed residual ridge for the replacement of a missing maxillary central incisor. Pract PeriodontIcs Aesthet Dent. 1999;2:229-232.
Spear F. A Conceptual Approach to Tooth Preparation, Tissue Management and Provisionalization for Anterior Restorations. [videotape] Clinical Topics in Dentistry. University of Nebraska-Lincoln; 1993.
Winter RR. Esthetic pontics. Dent Econ. 1994;5:92-93.
Dr. Thomas is a cosmetic and restorative dentist in private practice in West Des Moines, Iowa. He is a diplomate of the American Board of Aesthetic Dentistry and a general member of the American Academy of Cosmetic Dentistry. He can be reached at (515) 223-8800 or visit www.IowaSmiles.com.