The National Diabetes Education Program is a joint program of the National Institutes of Health and the Centers for Disease Control and Prevention. The program’s participants developed a proposal entitled “Team Care: Comprehensive Management for Diabetes.”1 In many ways, that proposal could be applied to programs for the control of dental and other oral diseases and conditions. This paper adopts components of the diabetes proposal for the control of periodontal diseases. In the process, important aspects of the American Academy of Periodontology (AAP) publication entitled Rights and Responsibilities of Patients2 were incorporated.
The AAP states in its Web site: “Periodontal diseases…are serious infections that, left untreated, can lead to tooth loss. Periodontal bacteria can enter the bloodstream and travel to major organs…Research is suggesting that this may:
•Contribute to the development of heart disease, the nation’s leading cause of death.
•Increase the risk of stroke.
•Increase a woman’s chance of having a preterm, low-birthweight baby.
•Pose a serious threat to people whose health is compromised by diabetes, respiratory diseases, or osteoporosis.”3
This unique interrelationship between periodontal diseases and systemic diseases and conditions compels dentistry to establish and maintain a “team care” program for the patients we treat, which is similar to the one proposed for the management of diabetes. That proposal defines team care as multidisciplinary care for patients. Like the diabetes program, the periodontal model would incorporate a wellness model including health promotion and disease prevention in addition to intensive clinical management of patients with periodontal diseases.
Team care integrates the skills of different healthcare professionals with those of the patient into a comprehensive, lifelong, periodontal disease-management program. Similar to the diabetes model, the patient is central to the team. The team would include the patient’s dentist, general dental hygienist, the periodontist, the periodontal dental hygienist, as well as auxiliary personnel such as dental assistants and possible other healthcare providers. The common goal of this program would be establishing and maintaining periodontal health for all of its patients.
THE NEED FOR A BETTER SYSTEM
Many factors affect today’s dental healthcare environment, including greater numbers of aging and older individuals, a declining dentist/patient ratio, too few dental hygienists, advances in treatment options for periodontal diseases, and the presence of a high percentage of patients in general practice with periodontal diseases, some of whom may not be diagnosed, treated, and/or referred.4
To achieve the best control of periodontal diseases, treatment must be as follows:
•continuous, not irregular;
•proactive, not reactive;
•planned, not sporadic; and
•patient centered rather than provider centered.
A chronic disease model for diabetes and other chronic illnesses affecting people in the United States incorporates all of these characteristics. Numerous publications support the rationale for a chronic disease model.5-7
Data collected from general dental practices have demonstrated that on average 78% of patients evaluated have periodontal diseases.8 If these data are accurate, general dentists and hygienists alone could not possibly treat all of the patients with periodontal diseases in the population. Likewise, periodontists alone could not possibly treat all patients. It is clear that effective treatment of periodontal diseases requires communication, cooperation, and collaboration among all members of the team. Team care integrates the skills of the primary providers—the general dentists and hygienists—with periodontists, their hygienists, possibly a physician or other healthcare professional, and the patient into a comprehensive, lifelong, periodontal disease-management program.
Essential elements for team success include the following:
(1) regular communication among team members and documentation of care provided;
(2) reimbursement for the services of the core team members relative to expertise and nature of treatment provided; and
(3) continuing efforts to educate policy makers (eg, purchasers of dental benefits, providers of dental benefits, benefits managers, and chief executive officers) about the importance of treating and controlling periodontal diseases.
RECOMMENDED ACTION STEPS
Dental healthcare providers would need to consider the following:
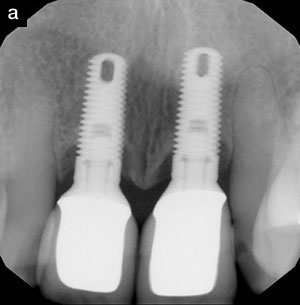
•Ensure that all patients in general practice have a periodontal screening. If there is evidence of periodontal disease, a complete periodontal exam, including appropriate radiographs, should be performed.9
•The general practice component of the team would then provide disease-control therapy or refer the patient to the periodontist on its team.10
•Whether the patient is treated in general or periodontal practice, a re-evaluation would need to be performed within 2 months after disease control to remeasure pockets, or more ideally, clinical attachment levels to evaluate treatment results.
•The patient would then be placed into a periodontal-maintenance program. For the majority of treated patients, the maintenance intervals would be 3 months, including annual periodontal evaluations of attachment loss.11
•Adjunctive therapies would be applied as needed. If sites are unresponsive to this treatment, more advanced treatment would be provided by the periodontist.
ADVANTAGES OF THE TEAM APPROACH
A multidisciplinary team brings together the particular skills, knowledge, and experience of several dental healthcare professionals to establish and maintain the periodontal health of its patients. This coordinated team care provides a high-quality method for achieving and maintaining periodontal health similar to a proposed ideal model for diabetes.12
Strategies to Apply
| Table. Gingival and Periodontal Diseases.13
|
(1) Stratify the patient population. In 1999, the AAP published the results of a conference on the classification of periodontal diseases.13 Using this classification system (Table) of more than 40 different gingival diseases in addition to 7 major categories of destructive periodontal diseases, a diagnosis would be made.
A co-chairman of that conference reported: “The diagnostic label…helps guide the clinician toward answering questions that are important to both the dentist and patients:
•What is the cause of the disease or condition?
•What will happen if the disease or condition is not treated? What are the treatment options?
•What is the best treatment?
•What is the expected outcome of treatment?
•What are the anticipated side effects of treatment?
•Will the treatment be painful?
•Will the treatment result in aesthetic problems?
•How long will treatment take?
•How much will treatment cost?”14
In addition, regarding establishing a diagnosis, he stated: “Before a diagnosis can be made, three questions have to be answered: Which periodontal diseases or condition does the patient have, what is the severity of the disease, and is the disease generalized or localized in nature?”14
(2) Define the team philosophies, goals, and objectives. This would require communication between members of the team. In many instances, it may require a physical meeting of the general dentist, periodontist, hygienists, and possibly even dental assistants.
(3) The team members of the general dental office would then determine the structure and scope of the program, including appropriate data collection, diagnosis and treatment planning, oral hygiene education, disease-control therapy, periodontal-maintenance therapy, adjunctive therapy as needed, appropriate risk counseling and risk factor reduction, and coordination of referrals to the periodontist.
(4) All dental healthcare providers would provide evidence-based care whenever possible in conjunction with the knowledge and experiences of the various team members. This would be done according to the standards of practice and in compliance with the ADA Principles of Ethics and Codes of Profes-sional Conduct.15
(5) The entire core team would develop a system that supports the continuity of care through regular team meetings and ongoing documentation and communication of pertinent information among team members, ideally via computerized information systems coupled with verbal contact, traditional written reports, and letters.
(6) The part of the core team that treats the individual patients would plan for regular assessment of clinical outcomes.
GUIDING PRINCIPLES TO THE CARE OF PERIODONTAL DISEASES
Principle 1: All patients in general dental practice with periodontal diseases have a right and should expect comprehensive data collection, diagnosis, treatment planning, and disease-control therapy followed by periodontal-maintenance therapy.
Principle 2: Patients have a right and should expect high-quality periodontal-maint-enance care on an ongoing basis, with continuity of care and with ongoing changes made to their treatment plan when needed to achieve better control of their periodontal disease.
Principle 3: Patients have a right and should expect informed consent. In other words, all of the periodontal problems have been diagnosed and presented to the patient along with treatment options, allowing the patient then to make an informed decision about choice of treatment.
Principle 4: Patients have a right and should expect referral to a periodontist when the necessary treatment is beyond the scope of the general dental team.
Principle 5: Patients have a right and should expect respectful and nondiscriminating care with access to their records and confidentiality of those records.
Principle 6: That part of the core team overseeing the patient’s periodontal care would serve in an advocacy role for the patient with other members of the team as well as with other healthcare providers, as necessary.
Principles of Patient Responsibility
(1) The patient must own the problem and must participate in the solutions.
(2) The patient must main-tain a high level of personal oral hygiene care.
(3) The patient must follow through with treatment.
(4) The patient must minimize whatever risk factors over which they have control.
(5) The patient must ob-tain periodic evaluations and periodontal-maintenance therapy after disease-control therapy.
SUMMARY
Periodontal diseases are a chronic, widespread disease problem. Treating periodontal diseases requires a team care approach. It also requires thorough examination, diagnosis, and treatment planning followed by disease-control therapy, periodontal-maintenance therapy, adjunctive therapy as needed, and referral to the periodontist if control of the disease is not established in the general dental practice. Only with collaboration and communication can a highly effective level of disease control be achieved. This disease control has a significant impact on the maintenance of the dentition and potentially on systemic health.
This paper reports on a treatment model for diabetes adapted to the treatment of periodontal diseases. This model, which incorporates elements of the AAP’s Rights and Responsibilities of Patients, provides a framework and foundation for improving the well being of patients with periodontal diseases.
References
1. Centers for Disease Control and Prevention. Team Care: Comprehensive Lifetime Management for Diabetes. National Diabetes Education Program Web site. Available at: http://www.ndep.nih.gov/diabetes/pubs/TeamCare.pdf. Accessed September 15, 2004.
2. Greenstein G, Rethman M. Rights and Responsibilities of Patients. American Academy of Periodontology News; November/December 1999.
3. Mouth Body Connection. American Academy of Periodontology Web site. Available at http://www.perio.org/consumer/mbc.top2.htm. Accessed Novem-ber 11, 2004.
4. American Dental Association. ADA Dental Workforce Model 2001-2025. Chicago, Ill: American Dental Association; 2003.
5. Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097-1102.
6. Etzwiler DD. Chronic care: a need in search of a system. Diabetes Educ. 1997;23:569-573.
7. Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12-25.
8. Townsend CL. Obligations that are opportunities. American Academy of Periodontology News Practice Management Column. January-March 2004.
9. Armitage GC; Research, Science and Therapy Committee of the American Academy of Periodontology. Diagnosis of periodontal diseases [published correction appears in J Periodontol. 2004;75:779]. J Periodontol. 2003;74:1237-1247.
10. Cohen RE; Research, Science and Therapy Committee of the American Academy of Periodontology. Position paper: periodontal maintenance. J Periodontol. 2003;74:1395-1401.
11. Research, Science and Therapy Committee of the American Academy of Periodontology. Treatment of plaque-induced gingivitis, chronic periodontitis, and other clinical conditions. J Periodontol. 2001;72:1790-1800.
12. Solberg LI, Reger LA, Pearson TL, et al. Using continuous quality improvement to improve diabetes care in populations: The IDEAL model. Improving care for Diabetics through Empowerment Active collaboration and Leadership. Jt Comm J Qual Improv. 1997;23:581-592.
13. 1999 International Workshop for Classification of Periodontal Diseases and Conditions. Ann Periodontol. 1999;4:1-112.
14. Armitage G. Periodontal diagnoses and classification of periodontal diseases. Periodontol 2000. 2004;34:9-21.
15. American Dental Association Principles of Ethics and Code of Professional Conduct. ADA Website. Available at: http://www.ada.org/prof/prac/law/code/index.asp. Accessed September 15, 2004.
Dr. Townsend is in full-time periodontal practice in Bellevue, Wash. She has lectured nationally for 25 years and has published several articles, one of which was published internationally. She was selected in 1989 and 1996 as one of 100 worldwide participants in the World Workshop in Periodontics. She currently serves as a District VI trustee to the AAP and has served as past president of the Washington State Society of Periodontists as well as the Seattle-King County Dental Society.