Construction of conventional mandibular dentures can be a frustrating restorative procedure for dentists to successfully accomplish, and this type of denture can be the most difficult prosthesis for patients to wear. Occasionally, it is not possible to achieve optimal retention and stability because of factors beyond adequate denture fabrication alone.1 These factors can include (1) poor jaw and ridge relationships, (2) neuromuscular coordination, (3) inadequate quantity and poor location of available bone and alveolar mucosa, and (4) inadequate vestibular width.
The widespread occurrence of edentulism creates both physiologic and psychologic problems because the alveolar ridge of denture wearers is very susceptible to resorption.2 Treatment alternatives to increase retention and stability include surgery to augment the alveolar ridge or increase vestibular depth, dental implants to provide anchorage for an all implant-supported prosthesis, or mucosa and implant-supported overdentures.3 It has been demonstrated that patients whose dentures lack stability, particularly the mandibular denture, benefit significantly from even slight increases in denture retention.4 Grogono et al found the most common reason that patients elect to have implant treatment is to improve eating ability.5
The implant overdenture is an especially attractive treatment because of its relative simplicity, minimal invasiveness, and economy.5 Existing complete dentures can be converted for many patients and maintain facial support with denture flanges when moderate-to-extreme alveolar ridge resorption is present. The implant overdenture is supported by both implant and mucosa; therefore, fewer implants are necessary than for the prosthesis supported only by implants.3 Two or more implants connected by a bar has been the treatment norm for implant-supported overdentures. Engquist et al reported that separate attachments are easily used in a number of different situations and are less expensive relative to the bar attachment.6 Also, patients with limited vertical dimension of occlusion may have inadequate space for a bar overdenture. Burns et al reported that independent implant placement may be beneficial in the control of hyperplastic tissue formation occasionally associated with the use of the bar attachment.3 Intimate contact between the denture base and supporting tissues is maintained over a larger surface area with the use of independent fixtures rather than with a bar overdenture.
The initial research of a porous-surfaced implant was reported in 1986.7 This contemporary implant is a tapered, truncated–cone-shaped, endosseous root-form implant fabricated of titanium alloy. The implant uses a powder-sintered, porous surface geometry over most of its length to promote 3-dimensional bone ingrowth and implant stabilization. In the initial study,7 24 porous-surfaced implants were placed in dogs. Two implants were placed in edentulous areas on each side of the mandible of each dog and covered with a full-thickness mucoperiosteal flap. The implant sites on one side of the mandible were allowed to heal for 4 weeks, while those on the other side were allowed to heal for 8 weeks before the animals were sacrificed. Histological specimens were obtained and assessed both qualitatively and by computer-assisted morphometry. All but one of the 24 implants were well-tolerated and healed with variable ingrowth of bone into the porous-surface geometry. The histomorphometric measurements revealed that bone ingrowth had reached a plateau by 4 weeks of initial healing.
The initial research in humans with a porous-surfaced implant was performed at the University of Toronto.8 In this trial, 3 implants were placed in the anterior mandibles of 52 patients and were used as freestanding units to support an overdenture. Shorter implants were used with reduced initial healing periods and simpler surgical techniques than are customary with other implant designs. The cumulative survival rate after 3 years was 8 failures, for a 94.8% success rate. Six of the 8 failures occurred in 4 patients in the first 12 months. All 4 patients were smokers.
A porous-surfaced implant (Endopore Dental Implant System, Innova Corp) was introduced in North America in 1993. The Midwest Implant Institute agreed to participate in the clinical investigation of the implant conducted for the FDA.9 In this trial, 69 implants were placed in the anterior edentulous mandibles of 23 patients. Three implants were placed in each patient to serve as freestanding overdenture abutments. Over a 3-year period, 2 implants failed to integrate after uncovering, and 3 implants were lost to follow-up. The success rate was 97%.
The first porous-surfaced implant course in the United States was conducted at the Midwest Implant Institute in Columbus, Ohio, in June 1995. The research, clinical success, and simplicity of the implant resulted in its use at the College of Dentistry, University of Tennessee Health Science Center. A general dentist with a good knowledge of sterile surgical technique can manage the surgical and prosthetic techniques required of the implant system.10 The implant was intended for use by residents of the Advanced Education in General Dentistry (AEGD) program and at the university’s dental practice by a general dentist. However, residents of the program in graduate periodontics, senior dental students, and private dentists in an implant externship are also placing and restoring porous-surfaced implants.
Since October 1995, 119 porous-surfaced implants have been placed in patients at the College of Dentistry, University of Tennessee Health Science Center for use as single overdenture abutments in the anterior mandibles of 39 patients. Thirty-seven patients received 3 implants and 2 patients received 4 implants. Prefabricated overdenture abutments were placed on all implants as retainers for mandibular dentures. Thirty-five patients were restored using O-rings and 3 patients were restored with Dalla-Bona attachments (Innova Corp). One patient with 3 implants lost all of them due to a traumatic injury. Two implants were replaced in original sites and the patient was restored with Dalla-Bona attachments. One patient with 3 implants lost 2 implants 6 months after restoration due to peri-implantitis. After bone regeneration, 2 implants were replaced in the original sites and restored with O-rings. These patients are now stable. No implants were lost by any other patients.
CASE 1: RESORBED MANDIBULAR RIDGE
A 62-year-old edentulous white male presented for evaluation for mandibular implants to support an overdenture. The patient’s dentures were 5 years old and serviceable, but he was unable to function with the mandibular denture. The patient’s medical history included Type I diabetes and quadruple bypass heart surgery. His diabetes was well controlled with insulin, and he had no additional heart problems 6 years after his bypass surgery.
 |
 |
| Figure 1. The patient’s mandibular ridge is inadequate for denture stability. | Figure 2. A panographic radiograph shows sufficient width between the mental foramina and adequate vertical height for 3 implants. |
 |
| Figure 3. A full-thickness mucoperiosteal reflection shows the bony ridge with initial osteotomy sites. |
 |
 |
| Figure 4. The right mental foramen is isolated. The osteotomy site will be located 5 mm mesial to the foramen. | Figure 5. Parallel pp/dg gauges are placed in the osteotomies. Note parallelism of the pp/dg’s. |
The patient’s mandibular ridge was evaluated clinically (Figure 1) and radiographically. A panographic radiograph revealed adequate mesial-distal width between the mental foramina and adequate vertical height to place 3 implants (Figure 2). The area for implant placement was anesthetized with local infiltration. Block anesthesia was not used. A midcrestal incision was made and a full-thickness mucoperiosteal flap was made, revealing the bony ridge (Figure 3). The mental foramina were isolated and the sites for the distal implants were located 5 mm anterior to the foramina to reduce the possibility of trauma to the mental nerve11 (Figure 4). The midline osteotomy site was located and the pilot drill was taken to a depth of 9 mm. A parallel pin/depth gauge (pp/dg) was placed in the osteotomy to determine angulation and parallelism. The distal osteotomies were taken to 9 mm with the pilot drill using the midline pp/dg as a guide. Placement of pp/dg’s in the osteotomies provided feedback to ensure that the implants would be parallel (Figure 5).
 |
 |
| Figure 6. Trial fit gauges are tapped to the final depth in all osteotomies. Note gauges in position with the maxillary denture. | Figure 7. The implants are tapped to place. Healing caps are attached to implants during manufacture. |
The osteotomies were completed with the implant bur and trial fit gauges, which are shaped like the implants. The trial fit gauges were tapped to the final implant depth and were so tight that they were difficult to remove with hemostats (Figure 6). Completion of osteotomies with trial fit gauges ensures stability and more predictable integration of porous-surfaced implants. Three 4.1- x 9-mm implants were inserted into each osteotomy and tapped to place (Figure 7). The surgical area was closed with individual sutures and the patient healed uneventfully.
 |
 |
| Figure 8. Rubber dam sections and silicone O-rings are placed on the abutments. | Figure 9. The patient’s mandibular denture is altered so abutments are not in contact with the denture. |
 |
| Figure 10. O-rings are processed in the patient’s denture; the denture is relieved and is not in contact with the abutments. |
At 12 weeks, the implants were uncovered and overdenture abutments were attached to the implants. Individual pieces of rubber dam were placed over each abutment along with silicone O-rings (Figure 8). The rubber dam material restricts the acrylic from touching the tissue and guards against the denture material locking in the denture as the material cures. The patient’s denture was modified to fit passively on the tissue without contact with the implant abutments (Figure 9). Self-curing acrylic was placed in the modified areas of the denture and around the abutments. The denture was seated and the patient was instructed to bite in centric occlusion against the maxillary denture until the material began to set. The denture was removed with the O-rings embedded and the denture was relieved so only the O-rings were in contact with the abutments (Figure 10).
 |
 |
| Figure 11. Slight bleeding exists upon probing but probing depths are minimal. Good hygiene can eliminate bleeding. | Figure 12. A panographic radiograph shows implants with attached abutments and stable crestal bone around the implants. |
After 5.5 years, the implants are stable with minimal probing depths around the abutments (Figure 11). A panographic radiograph of the mandible shows the implants with abutments and stable crestal bone around the implants (Figure 12).
CASE 2: EXCESSIVELY RESORBED MANDIBULAR RIDGE
 |
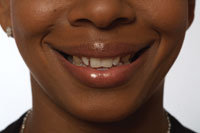
| Figure 13. A virtually nonexistent mandibular ridge is present and is inadequate for denture stability. |
A 47-year-old edentulous white male presented for treatment. The patient’s medical history included multiple sclerosis, arthritis, and a functional heart murmur. His dental history included a full-mouth extraction and construction of maxillary and mandibular dentures at the age of 15 years. The patient was unable to wear the mandibular denture because of pain when he attempted to chew. The patient’s mandibular ridge was essentially nonexistent (Figure 13).
 |
| Figure 14. A panographic radiograph shows an excessively resorbed mandibular ridge, dehisced mental foramina, and mesial-distal width for 4 implants. |
A panographic radiograph revealed an excessively resorbed mandibular ridge with dehisced mandibular nerves in areas of the mental foramina (Figure 14). Adequate mesial-distal width existed between foramina to place 4 implants, and vertical bone height was adequate for 7-mm or 9-mm implants. The prosthetic scheme included an anterior overdenture bar with plastic sleeves constructed in the denture for retention and stability. The patient’s physician stated that the patient was neurologically stable and should be prophylactically covered with antibiotics prior to implant surgery.
 |
 |
| Figure 15. Four pp/dg’s are placed in the osteotomies. Note the lingual undercut of the bony ridge. | Figure 16. Trial fit gauges are tapped to the final depth in all osteotomies. |
 |
 |
| Figure 17. The implants are tapped to place. | Figure 18. The surgical area is closed with continuous suture. |
The area for implant placement was anesthetized with local infiltration. Block anesthesia was not used. A midcrestal incision was made anterior to the mental foramina and a full-thickness mucoperiosteal flap was made. The mental foramina were carefully exposed and distal osteotomy sites were located 5 mm mesial to the foramina. The mesial osteotomy sites were located 6 mm mesial to the distal sites. The pilot drill was taken to 7 mm in all sites and pp/dg’s placed in all sites (Figure 15). A 7-mm implant bur and trial fit gauges were used to complete the osteotomies (Figure 16). Four porous-surfaced implants 4.1 mm wide x 7 mm long were tapped to place (Figure 17). The surgical area was closed with continuous suture and the patient healed uneventfully (Figure 18).
At 14 weeks, the implants were uncovered. The patient requested that his present mandibular denture be modified so he could wear it while his new dentures were being constructed. Prefabricated overdenture abutments were attached to the implants. The patient’s present denture was altered and relined with soft reline material over the abutments, which provided satisfactory retention for the denture. The occlusion of the denture was adjusted and the patient was reevaluated at 1 week. The patient was delighted with the retention of the modified denture and said that he could chew without pain. He requested that an overdenture be made with the present abutments to save time and delete the extra expense of a bar overdenture.
After primary impressions were made, custom impression trays were fabricated. Master impressions were made for a conventional maxillary denture and implant-retained mandibular overdenture. Analogues were placed in the mandibular master impression and a master cast was constructed. Silicone O-rings were placed on the analogues prior to processing the overdenture. After fabrication, the overdenture was adjusted so that only O-rings were in contact with the abutments. The overdenture was very retentive, and the O-rings were relieved so the patient could remove it.
The patient was placed on 6-month recall, which is standard regimen for overdenture implant patients. Six-month recall visits for mandibular overdenture patients include hygiene instructions, probing of abutments, retorquing abutments to 30 Nt-cm, O-ring replacement, and denture adjustment (if necessary). Panographic radiographs are made every 6 years.
 |
 |
| Figure 19. A panographic radiograph shows implants 7 mm long with attached abutments. Crestal bone height is stable around the implants. | Figure 20. The implants are solid and tissue around the abutments is healthy with minimal probing depths. |
After 6 years, a panographic radiograph of the patient’s mandible indicated that crestal bone is stable around all implants (Figure 19). Clinically, the implants are solid, probing depths are minimal, and tissue around the abutments is healthy (Figure 20).
CONCLUSION
Mandibular overdentures retained with single overdenture abutments are stable, retentive, and functional for patients with resorbed ridges who are unable to chew with conventional dentures. Laboratory procedures are simple and overdentures are easily maintained and repaired. Because of the increased surface area of porous-surfaced implants, smaller and shorter implants can be placed for use with single overdenture abutments. This allows patients with excessively resorbed mandibular ridges the opportunity for treatment with mandibular overdentures. As few as 3 anterior mandibular implants can support a complete arch overdenture.12 Porous-surfaced implants are easily placed, although the surgical procedure is technique-sensitive. Patients with serviceable mandibular dentures have the option of modifying their existing dentures to receive overdenture abutments or constructing new overdentures that are equivalent in cost to conventional dentures.
References
1. Tarbet WJ, Boone M, Schmidt NF. Effect of a denture adhesive on complete denture dislodgement during mastication. J Prosthet Dent. 1980;44:374-378.
2. Carlsson GE, Persson G. Morphologic changes of the mandible after extraction and wearing of dentures. A longitudinal, clinical, and x-ray cephalometric study covering 5 years. Odontol Revy. 1967;18:27-54.
3. Burns DR, Unger JW, Elswick RK Jr, et al. Prospective clinical evaluation of mandibular implant overdentures: Part I—Retention, stability, and tissue response. J Prosthet Dent. 1995;73:354-363.
4. Burns DR, Unger JW, Elswick RK Jr, et al. Prospective clinical evaluation of mandibular implant overdentures: Part II—Patient satisfaction and preference. J Prosthet Dent. 1995;73:364-369.
5. Grogono AL, Lancaster DM, Finger IM. Dental implants: a survey of patients’ attitudes. J Prosthet Dent. 1989;62:573-576.
6. Engquist B, Bergendal T, Kallus T, et al. A retrospective multicenter evaluation of osseointegrated implants supporting overdentures. Int J Oral Maxillofac Implants. 1988;3:129-134.
7. Deporter DA, Watson PA, Pilliar RM, et al. A histological assessment of the initial healing response adjacent to porous-surfaced titanium alloy dental implants in dogs. J Dent Res. 1986;65:1064-1070.
8. Deporter DA, Watson PA, Pilliar RM, et al. A prospective clinical study in humans of an endosseous dental implant partially covered with powder-sintered porous coating: 3- to 4-year results. Int J Oral Maxillofac Implants. 1996;11:87-95.
9. Heller AL, Heller RL. Clinical evaluations of a porous-surfaced endosseous implant system. J Oral Implantol. 1996;22:240-246.
10. Fleming AE. The Endopore dental implant system: implant treatment simplified. J Can Dent Assoc. 1994;60:785-789.
11. Tatum OH Jr, Lebowitz MS. Anatomic considerations for dental implants. J Oral Implantol. 1991;17:16-21.
12. Weiss CM, Weiss A. Principles and Practice of Implant Dentistry. 1st ed. St Louis, Mo: Mosby; 2001:192.
Dr. Cloyd is professor in the Department of Restorative Dentistry and in the Program in Dental Science, College of Graduate Health Sciences, University of Tennessee, Memphis. He also serves as director of the Advanced Education in General Dentistry (AEGD) program. He is a graduate of the Midwest Implant Institute and is an honorary fellow and faculty member. Dr. Cloyd has served as aconsultant in implant dentistry for the Dental Department, Veterans Administration Hospital, Memphis, Tenn, the post-doctoral general dentistry programs of the Lutheran Medical Center, Brooklyn, New York, and the AEGD program at Oklahoma University College of Dentistry, Oklahoma City, Okla. He teaches implant dentistry to residents of the AEGD program and graduate program in periodontics and to senior dental students. He places and restores dental implants for private patients as an associate member of the university dental practice, and he directs a comprehensive implant course and externship for dentists in private practice. A component of the externship allows dentists to place implants in their patients at the College of Dentistry, University of Tennessee, Memphis, under the supervision of Dr. Cloyd. He can be reached at (901) 448-7180.