INTRODUCTION
Complete edentulism can be defined as “the physical state of the jaw(s) following removal of all erupted teeth and the condition of the supporting structures available for reconstructive or replacement therapies.”1 It is estimated that the need for complete dentures will have increased from approximately 54 million in 1991 to approximately 61 million by 2020.2 Although the rate of edentulism will have decreased, the aging population will bring with it an increase in the number of teeth lost.3 Due to longer life spans and the aging baby boomers, the number of Americans age 65 years and older will double over the next 25 years. By 2030, there will be 71 million older adult Americans who will account for approximately 20% of the US population.4 The Centers for Disease Control and Prevention’s State-Based Examples of Network Innovation, Opportunity and Replication grant program includes an oral health component which identifies several approaches to improve the oral health of older adults, including the development of innovative and effective strategies to prevent and treat dental disease.
To address the disease of edentulism, dental endosseous implants are being used as a therapeutic adjunct and can reduce the problem of long-term bone resorption to less than 0.1 mm per year.5 Tissue-supported prostheses do not treat alveolar bone loss, disuse atrophy, or pressure mediated resorption, which are all germane to edentulism. Therefore, they are only rehabilitative, not therapeutic.
According to a consensus statement on overdentures from McGill,6 there is “overwhelming evidence that a 2-implant retained overdenture should become the first choice of treatment for the edentulous mandible.” However, the 2-implant retained mandibular overdenture is tissue-supported; thus, stable conventional complete dentures must still be fabricated. The 2 implants stabilize and cannot support the prosthesis.7
It is therefore incumbent upon clinicians to ensure that the best evidence-based treatment plan is developed for the edentulous patient. Furthermore, they should take the leading role in the selection of appropriate materials and prosthesis design for each patient, while still involving the laboratory technologist in the treatment planning process.
CASE REPORT
A 43-year-old white female was referred for fabrication of new maxillary and mandibular complete dentures. Her goals were to improve her appearance, self-confidence, and function with a long range plan for maintenance. The deficiencies in her current prostheses adversely affected her personal life and professional career. She received infrequent dental care as a child. Her maxillary teeth were extracted at age 31 years due to caries, and a maxillary immediate complete denture was delivered.
 |
|
Figure 1. Pretreatment prostheses. |
Soon thereafter, a mandibular removable partial denture was fabricated. The patient presented for examination with an existing maxillary complete denture opposing a removable partial denture, with prosthetic teeth having been added as teeth were extracted (Figure 1). She had been wearing her prostheses most of the day and while sleeping. The existing prostheses were approximately 3 years old, and the maxillary immediate denture had been relined approximately 6 months after delivery.
Summary of Clinical Findings
The patient displayed a prominent chin, nasiolabial folds, thin lips, and elongated commissures. There was insufficient upper lip support and an apparent deficiency in the prosthetic occlusal vertical dimension (OVD) (Figures 2 and 3). There was approximately 5 mm interocclusal rest space, and the maximum opening was 40 mm, with deviation to the right side upon maximum opening. There were no audible joint sounds, pain, or tenderness on palpation over the temporomandibular joints, the preauricular areas, or muscles of mastication. The oral mucosa, lips, tongue, floor of the mouth, and oropharynx were without pathoses. The maxilla presented with ulcerated areas and generalized erythema (Figure 4). The saliva was serous and of normal quantity. Amalgam tattoos were present in positions Nos. 3, 5, and 7.
 |
 |
|
Figure 2. Pretreatment occlusal vertical dimension (OVD), frontal view. |
Figure 3. Pretreatment OVD, lateral view. |
 |
 |
|
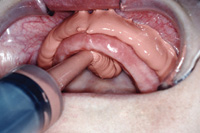
Figure 4. Pretreatment view of the maxillary arch. |
Figure 5. Pretreatment view of the mandibular arch. |
 |
|
Figure 6. The orthopantomograph. |
The maxillary arch showed decreased posterior vestibular depth, vertical and horizontal bone loss, indistinct hamular notches, slightly mobile tuberosities, and a palatal vault that would minimally resist horizontal denture movement. The anterior edentulous ridge was firm. The soft palate form was a House Class I, and she displayed a hypertrophied tongue with normal position (Wright’s Class I).
The mandible displayed an adequate attached mucosal base in all regions except the anterior facial and lingual vestibules in the canine to canine region, high genioglossus, and mentalis muscle attachments. The mandibular bone height, as measured on the panoramic radiograph (Figures 5 and 6), was 15 mm at its narrowest dimension.
Retromolar pads and buccal shelves were well defined. The retromylohyoid areas showed significant undercut, a Neil’s Class II Lateral Throat Form, and insignificant mylohyoid ridges. In centric relation (CR), the patient occluded only on her anterior teeth and appeared as a Class I maxillomandibular relationship.
Diagnosis and Treatment Planning
According to the American College of Prosthodontists’ Prosthodontic Diagnostic Index for Complete Edentulism (ACP PDI CE),1 the maxilla was moderately compromised (Class II), and the mandible was substantially compromised (Class III ). The ACP PDI CE maxillomandibular relation was Class I.
The maxillary residual alveolar ridge demonstrated soft-tissue trauma and candidiasis, possibly secondary to unstable, nonretentive existing removable prostheses. Radiographic interpretation revealed probable idiopathic condylar resorption (ICR) of the right condyle. Amalgam tattoos were present, in addition to an apparent loss of prosthetic OVD. The patient was a house personality classification of “Philosophic.” Overall, the diagnosis was an ACP PDI CE Class III (Substantially Compromised).
Due to financial considerations, the primary treatment option was a conventional maxillary complete denture opposing a 2-implant retained mandibular overdenture. The treatment plan included soft-tissue oral hygiene and denture maintenance instructions, tissue conditioning, and re-establishing posterior occlusal support in her existing prostheses. It was important to develop healthy tissue before making the definitive impressions. The clinical/radiographic findings were reviewed and the treatment plan presented and discussed to ensure the patient’s expectations were realistic and consistent with the proposed treatment.
The patient was informed of the indications for care, fees, goals, benefits, and risks of alternative treatment options. She also was informed of the factors affecting care, the need for her continued active maintenance, future care, and the long-term outcome expected. There was mutual agreement about her responsibilities, commitment, and expectations for treatment outcome.
Informed consent was obtained prior to initiating treatment.
Treatment
The patient immediately began using 2% Ketoconazole cream (Teva) and a Bezalkonium Chloride 1:750 denture soak (Zephiran [Sanofi-Synthelabo]). The existing prostheses were lined with a soft-tissue conditioning material (Lynal [DENTSPLY Caulk]), then mounted on a semi-adjustable articulator (Hanau Wide View [Whip Mix]) using a Hanau Earpiece face-bow and a CR record with Alu Wax at the proposed OVD. Auto-polymerizing acrylic resin was added to the occlusal surfaces to stabilize the dentures and improve posterior support. The length of the lip at rest (Figure 7) was measured with a papillameter (Ivoclar Vivadent).
 |
 |
|
Figure 7. The papillameter. |
Figure 8. Maxillary final impression. |
 |
 |
|
Figure 9. Mandibular diagnostic impression. |
Figure 10. Centric tray. |
After establishing tissue health, impressions were made with a dual phase irreversible hydrocolloid (Accu-Dent System 1 [Ivoclar Vivadent]), a master maxillary impression (Figure 8), and a preliminary mandibular impression (Figure 9). A preliminary CR and OVD record was made with a Centric Tray device (Ivoclar Vivadent) (Figure 10). This was only an approximation of CR and the planned OVD. This recording, along with the Papillameter measurement, enabled the laboratory to fabricate wax rims (Figure 11) that required less intraoral adjustment.
 |
 |
|
Figure 11. Wax rims. |
Figure 12. Central bearing striking plate. |
 |
 |
|
Figure 13. Central bearing screw assembly. |
Figure 14. Mounted central bearing assembly. |
 |
 |
|
Figure 15. Fox plane. |
Figure 16. The Fox plane, once leveled. |
 |
 |
|
Figure 17. Maxillary rim with silicone. |
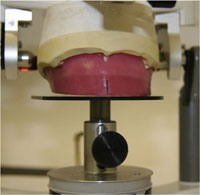
Figure 18. Maxillary rim with silicone on a flat mounting table. |
A second maxillary acrylic base was made to retain the striking plate of an intraoral central bearing assembly (Figure 12), to be used for definitively recording CR and the OVD. The mandibular wax rim contained the central bearing point assembly (Figures 13 and 14). Adjustments were made to the maxillary wax rim for proper aesthetics, phonetics, horizontal aesthetics and Camper’s planes.
In lieu of adding or subtracting wax to refine this parallelism, a Fox plane and silicone were used to level the Fox plane parallel to the floor in a medial-lateral dimension and parallel to Camper’s plane in the anterior-posterior dimension (Figures 15 to 17). The maxillary rim and silicone shim were used with a Stratos Mandibular Flat Plane Table (Ivoclar Vivadent) (Figure 18) to mount the maxillary cast, similar to the use of the Kois Dento-Facial Analyzer (Panadent). This replaced the face-bow and ensured that the anterior smile line and posterior plane of orientation were aesthetically pleasing and not sloping inferiorly, unilaterally, or bilaterally (Figure 19).
The vertical dimension was determined by the patient using the central bearing assembly and neuromuscular perception of comfort.8 The central bearing assembly helped relax the patient, and a repeatable CR position was recorded at the vertical dimension determined by the patient. Virtual Quickset Bite Registration (Ivoclar Vivadent) was injected between the upper and lower record bases, thus locking the assembly together (Figure 20). This was used to mount the diagnostic mandibular cast on an average-value articulator (Stratos 100 [Ivoclar Vivadent]).
Given the patient’s wide smile and demand for superior aesthetics, a nanohybrid composite tooth (SR Phonares NHC [Ivoclar Vivadent]) was selected. The Phonares Typ (Ivoclar Vivadent) posterior tooth mould was selected to achieve bilateral balanced occlusion. This tooth is designed to be set in a “one tooth-to-2 teeth” occlusal relationship (Figure 21) and maximizes aesthetics through the premolar region. The laboratory will set teeth on the maxillary rim and diagnostic mandibular record base, which once housed the central bearing assembly.
 |
 |
|
Figure 19. View revealing the maxillary rim deficiency. |
Figure 20. Centric relation/vertical dimension recording. |
 |
 |
|
Figure 21. One tooth-to-2 teeth set-up. |
Figure 22. Mandibular final impression. |
 |
|
Figure 23. View of the injection molded acrylic with custom tinting (Robert Kreyer, CDT). |
The patient returned for wax try-in and evaluation of aesthetics, phonetics, OVD, and CR. Upon verification of the above and approval of aesthetics by patient and friend, the mandibular wax-up was duplicated in clear auto-polymerizing acrylic resin. Five-millimeter stainless steel balls were placed in the proposed implant positions to act as radiographic and subsequent surgical guides. Ideally, implant positions should be planned such that additional implants (eg, 2 to 3) can be placed in the future.3,5
Two SLA endosteal implants (Straumann) were placed near the Nos. 22 and 27 positions. Following 12 weeks of healing, a new mandibular Accu-Dent impression was made for construction of a light-polymerizing acrylic resin Light Tray (Ivoclar Vivadent) custom impression tray with wax relief. Intraorally, the healing abutments were removed and the appropriate cuff height LOCATOR Abutments (Straumann) were torqued to 35 Ncm. The mandibular arch was border molded with modeling plastic impression compound, and abutment level impression copings were picked up with a light viscosity polyvinylsiloxane (PVS) impression material (Extrude [Kerr]) (Figure 22).
Abutment analogs were attached and the master cast poured in Type III gypsum. A new record base/wax rim was fabricated on the mandibular master cast to again retain the central bearing assembly. This also was used with the previously constructed maxillary record base/striking plate to record the vertical dimension and CR, as previously described. The mandibular master cast was mounted so that it could be related to the previously verified maxillary setup.
Mandibular Phonares Typ NHC teeth were set to match the maxillary setup. A subsequent wax try-in confirmed aesthetics, phonetics, OVD, and CR. The dentures were processed with an injection molding acrylic (SR Ivocap Injection System [Ivoclar Vivadent]), but without the Locator metal housings. The Locator housings would be picked up clinically 2 weeks after denture delivery (Figure 23).
Delivery, Post-Treatment Therapy, and Prognosis
The dentures were independently inserted and evaluated with Pressure Indicator Paste (Mizzy). The centric occlusal contact was determined, and the prostheses were clinically remounted with an Aluwax CR record. The centric occlusal contact was confirmed on the mounted casts, and the occlusion was refined. A PVS reline material (GC Reline Extra Soft [GC America]) was placed in the mandibular denture overlying the Locator abutments.
 |
 |
|
Figure 24. Post-treatment OVD. |
Figure 25. Post-treatment full smile lateral view. |
 |
| Figure 26. Post-treatment view of the patient in natural pose. |
Professional and home maintenance protocols were reviewed with the patient. Regular prosthodontic recall was emphasized to monitor fit, function, and condylar changes. The patient was very pleased with the comfort, function, and aesthetics of the prostheses. There was an improvement in the patient’s lip support and OVD (Figures 24 and 25). The patient confirmed her desire to work towards upgrading to a mandibular implant-borne prosthesis in the future.
The patient returned after 24 hours for a postdelivery evaluation. There were no reported problems at the one- and 2-week post-treatment visits. At 2 weeks, the Locator metal housings were independently picked up chairside with a bead-brush autopolymerizing polymethylmethacrylate (ProBase Implant [Ivoclar Vivadent]).
Due to ICR and increased biting force, the patient’s OVD and posterior soft tissue support demanded close monitoring. If she was not compliant with the post-treatment recommendations regarding prosthesis wear and recall, she could possibly experience Combination Syndrome-like intraoral changes.9 However, with patient commitment, positive attitude, and proper post-treatment care, her prognosis was good.
MATERIAL SELECTION
Manufacturers continually develop new products to enable clinicians to meet the demands of today’s patients. The manufacturers and the dental technologists are good sources for information on new products; however, it is the responsibility of the practitioner to remain educated on the appropriateness of materials for their patients’ specific needs.
Denture Tooth, Acrylic, and Occlusal Scheme Selection
Phonares Nanohybrid Composite (NHC) teeth were selected due to the patient’s demand for superior aesthetics. The SR Phonares FormSelector (Ivoclar Vivadent) utilizes the patient’s personality and age to simplify the selection process while involving the patient.
Phonares denture teeth are fabricated with NHC. The NHC consists of nanoparticles less than 50 µm in size, and hybrid particles of different types and sizes of fillers. Some are organic fillers for strength and color stability, others are urethanedimethacrylate for the matrix, inorganic fillers for wear resistance, and silanated silica based fillers for translucency.
A tissue-supported mandibular denture can move 10 mm or more during function, whereas a mandibular implant-retained denture allows a patient to more consistently return to CR and focus less attention on retaining the denture with the tongue, buccinators, and orbicularis oris muscles.10 Perhaps this contributes to the increased efficiency and biting force seen with implant-retained prostheses compared to tissue-supported dentures. This increased prosthesis stability and biting force dictates the need for a more wear-resistant prosthetic tooth. For this reason, Phonares Typ NHC with inorganic fillers were utilized.11 This increased wear resistance, however, necessitates more precise control over the occlusal contacts, since the patient will not self-equilibrate by normal wear as easily as if she had teeth without inorganic fillers. Close attention is therefore given to clinical remount and equilibration.
With implants comes a greater need for dimensional stability and masking the implant substructures. The dimensionally accurate precision injection molding system (SR Ivocap [Ivoclar Vivadent]) was used to compensate for acrylic shrinkage and reduce tooth movement during acrylic processing. The SR Ivocap system results in significantly less shrinkage in comparison to compression packing.12 Strohaver13 showed the mean increase in vertical dimension for compression packed processing to be 0.66 mm compared to 0.02 mm for the SR-Ivocap samples. In addition, the SR Ivocap Implant shade was developed to block out underlying attachments, thereby reducing dark spots associated with traditional acrylic.
FUTURE TREATMENT
Given the patient’s young age and the substantially compromised maxillary and mandibular anatomy, the goal was to eventually upgrade the patient to totally implant-supported prostheses. Ideally, the 2 implants should have been placed in the lateral incisor position to allow a future midline implant and 2 additional implants anterior to the mental foramen.3 Because the mandibular implants were not placed in the ideal position and the maxilla had poor morphology and severely pneumatized sinuses, the definitive dentures were duplicated into radiographic guides with Barium Sulfate for cone beam computed tomography (CBCT). Preoperatively, implant sites could then be planned in 3 dimensions to potentiate implant position and number.
DISCUSSION
During the initial appointment, clinical data, psychosocial and dental/ medical history, and the patient’s expectations should be recorded. A thorough examination and consultation ensures that the patient understands his or her problem and responsibility for a successful outcome. The patient’s commitment and ability to adapt also should be assessed. Anatomy should be evaluated in terms of potential to provide prosthesis retention, support, and stability. Both positive and negative patient factors should be discussed, as well as how each will affect the outcome.
Patients define success by subjective quality of life criteria. Therefore, treatment does not commence without patients’ acceptance of their responsibility for adaptation to the new prostheses. A thorough intraoral examination and patient education on the relationship among their anatomy, habits, and success builds respect and trust and is a great practice builder.
As there was no improvement in the prominence of the chin or nasiolabial folds, the aesthetic outcome might have been unacceptable to the patient had the limitations not been discussed and agreed upon before treatment. Successfully meeting the patient’s desire for excellent aesthetics, function, and bone preservation resulted in a return of her personality and the confidence to advance herself professionally (Figure 26).
CONCLUSION
The edentulous patient presents both anatomical and psychosocial factors which affect the treatment and outcome. By identifying these factors, patient expectations can be modified, thus avoiding disappointment. Rehabilitative and therapeutic treatment and a long-range plan for maintenance should be identified before initiating care. Through the use of CBCT, the number of implants and their position can be idealized to preserve bone and increase prosthesis stability. The edentulous population will increase for at least the next 20 years, along with demand for removable prosthodontic care. To meet this demand, more dentists must provide this service. Dental professionals can improve the quality of life for this growing population through removable prosthodontics, continuing education, excellent laboratory support, and advancing technology.
Acknowledgment
The author wishes to acknowledge Robert Kreyer, CDT, from Kreyer Dental Prosthetics in Larkspur, Calif, for fabricating the removable prostheses illustrated in this case presentation.
References
- McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont. 1999;8:27-39.
- Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002;87:5-8.
- Feine JS, Carlsson GE, eds. Implant Overdentures: The Standard of Care for Edentulous Patients. Chicago, IL: Quintessence Publishing; 2003.
- The State of Aging and Health in America. Atlanta, GA: Centers for Disease Control and Prevention; 2007.
- Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387-416.
- Feine JS, Carlsson GE, Awad MA, et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002;17:601-602.
- Preiskel HW. Overdentures Made Easy: A Guide to Implant and Root Supported Prostheses. Chicago, IL: Quintessence Publishing; 1996.
- Lytle RB. Vertical relation of occlusion by the patient’s neuromuscular perception. J Prosthet Dent. 1964;14:12-21.
- Palmqvist S, Carlsson GE, Owall B. The combination syndrome: a literature review. J Prosthet Dent. 2003;90:270-275.
- Sheppard IM. Denture base dislodgment during mastication. J Prosthet Dent. 1963 May; 13(3):462-468.
- SR Phonares [scientific documentation]. Principality of Liechtenstein: Ivoclar Vivadent AG; 2010.
- Gary C. Anderson, John K. Schulte, Thomas G. Arnold. Dimensional stability of injection and conventional processing of denture base acrylic resin. J Prosthetic Dent. 1988 Sept.; 60(3):397.
- Strohaver RA. Comparison of changes in vertical dimension between compression and injection molded complete dentures. J Prosthet Dent. 1989;62:716-718.
Dr. Williamson is a graduate of Texas A&M University, receiving his DDS degree from the University of Texas Health Science Center, Houston. He maintained a solo general practice in College Station for 17 years before returning to graduate school at the University of Nebraska Medical Center, Lincoln. Dr. Williamson holds a certificate in Prosthodontics and an MS in Oral Biology. He is a Diplomate of the American Board of Prosthodontics and a Fellow of the American College of Prosthodontists and International College of Dentists. Currently, Dr. Williamson is a clinical associate professor in the Department of Family Dentistry at the University of Iowa. Dr. Williamson provides fixed, removable, and implant prosthodontic care in a University of Iowa-based dental practice. Dr. Williamson lectures internationally on complete denture, removable partial denture, implant prosthodontic care, and other restorative options. He is also an American Dental Association CELL Seminar Series Speaker. He can be reached at richard-williamson@uiowa.edu.
Disclosure: Dr. Williamson lectures on techniques and principles of removable prosthodontics for Ivoclar Vivadent, but does not receive funding to promote their materials or products.