For far too long, the well understood anatomy and physiology of the head and neck has been only loosely associated with the dental treatment of patients. For many reasons, dentists have isolated the teeth and the pathology of dentition from the functional, dysfunctional, and parafunctional physiology that can cause wear, damage, fracture, abfractions, failure of restorations, and pain for their patients. These traumas and degenerations are but the signs and symptoms of an underlying problem. In the attempt to offer patients the opportunity for the best possible outcome, clinicians will be required to get to the foundational cause of these manifestations of disease, dysfunction, and, too often, despair.
It is the premise of this article that we can simply redirect the focus of the examination processes and the initial care sequences to address the underlying functional physiology. Patients then can be offered the opportunity to deal with their symptoms and problems in a way that will assure them of a pathway to long-term predictable health and dental stability. In addition, by addressing the problems at the level of the causation, we will be able to expand our care to include excellent results for many of our patients with intractable, late or end stage disorders that include severe dental disease as well as head and neck pain, range of motion disabilities, and accelerated aging related to dysfunction and poorly healed injuries.
CATEGORIZING DENTAL DISEASE
The nexus of tooth related problems with musculoskeletal and neurological physiology is at the point where the effects of muscle-related forces are applied to the teeth or to a bolus of food in a way that develops and determines the patterns of muscle activity through the sensorimotor neurology via the brainstem. When the neurology is abnormal (as in chronic pain) or when the muscle patterns are driven by central nervous system requirements (as in parafunction during sleep disturbances) or when the proprioception of the teeth is altered (as in sensitization or dental changes), then the forces are altered between the teeth via the musculature. How these forces are managed, sensed, and adapted to is the essence of force-related dental disease and dentomandibular sensorimotor dysfunction.
The vast majority of dental-related disease can be categorized into 3 primary issues:
- Bacterial/host response disease (especially periodontitis)
- Acid breakdown of tooth enamel
a. Caries
b. Acidic biofilm
c. Gastric acid (reflux)
d. Dietary acid - Force overload
a. Frictional
b. Compressive
c. Shear
d. Bending (abfraction).
Most restorative treatment currently done in dentistry on adults is a direct result of force-related problems. And, of course, aside from external trauma, these abnormal forces are applied to the teeth by the patient’s muscles. The forces that cause the breakdown of the teeth also cause the acceleration of periodontal breakdown and the early breakdown of previous restorative attempts.
Whether we observe open margins, fractures, wedge defects (abfractions), wear, sensitivity, mobility, or failed restorations, there is reliably an underlying force problem at play. We call this “stress in the system.”
Truly, we can redefine the term “malocclusion” to mean “abnormal forces between some or all of the teeth that results in damage to the integrity of the tooth anatomy or the periodontal interface, or resulting in pain to the patient.”
Malocclusion related pain can manifest as hypersensitivity, deep tooth pain, jaw pain, or pain in the head and neck region served via the trigeminal cervical nucleus. This definition of malocclusion does not necessarily exclude other definitions that refer to the interdigitation of the teeth, or the location of centric stops on the teeth. Rather, this definition allows a perspective on occlusion that addresses the direct relationship of functional physiology to the disease and degeneration that we observe and treat.
Force-Balanced Occlusion
There must then be a force-related definition of a normal or healthy occlusion. I would suggest the following definition: “A system of interdental forces that are well distributed around the arch with an unhindered path to closure and to mastication via effective proprioceptive and somatosensory guidance. The interdental forces should be distributed down the long axis of the posterior teeth with the total forces balanced 50/50 right to left during a full closure to interdigitation.”
Additionally, the ability to masticate without working or nonworking interferences within a normal envelope of function distributes muscle activity with both symmetry and synergy. There should be musculoskeletal stability and symmetry of the temporomandibular joints (TMJ) with the discs normally interposed at full closure. The patient is comfortable in rest and in full closure, and the mandibular range of motion is within normal limits.
Many other conditions may also be present to demonstrate normal health, including but not limited to:
• Patient comfort at rest, and in function
• No acute or chronic pain
• Normal cervical range of motion
• Normal posture
• Normal work abilities
• Normal tooth anatomy and mobility
• No exposed dentin
• No dietary restrictions due to dental function.
| T-Scan Technology Explained |
|
Lou Shuman, DMD CLINICAL APPLICATIONS |
As we explore further into the realm of “force-balanced occlusion,” we will encounter many other issues that can disrupt the normal function of the musculature. We will see that as patients develop pathology or have dentistry done, there will be changes to the balance and function of the mandible. Whether this is as simple as a sore or sensitive tooth after restoration, or as complex as the creation of an adapted interdigitation to avoid extreme forces, the patient’s proprioceptive system will constantly adapt to changes. This can result in malpositioned or dislocated condyles during mastication or swallowing, clenching, early disc movement that can precede disc displacement, or patterns of self-equilibration to “grind in” the original force balance through self-mutilation.
Occasionally, these adaptive changes will result in the conversion of acute pain to chronic pain. This then will cause the patient to undergo many neurochemical adaptations as well as compensatory muscle activity that can limit range of motion (mandibular or cervical) and/or result in trigger point muscle spasms.
The signs and symptoms of a “malocclusion” can be manifest in the teeth, muscles, or joints. This triad of anatomy we will refer to as the “dental foundation.”
The dental foundation is considered to be out of balance when any of the following conditions exist:
• Accelerated aging or degeneration of the TMJ condyles
• TMJ vibrations indicative of disc movement, disc derangement, or inflammation
• Tooth damage or degeneration related to abnormal forces
• Limited range of motion of the mandible or the cervical spine
• Presence of sore or painful muscles of the head and neck, especially the presence of “trigger points”
• Symptoms of pain that emanate from the structures connected via and controlled by the trigeminal cervical nucleus, especially headache
• Any lifestyle disability related to the teeth, muscles, or joints of the head and neck
• Abnormal forces are detected in the dentition by examination
• Injuries have occurred that affect any of the above structures or activities.
Generally speaking, any time we need to address a patient’s symptoms that are connected to the dental foundation, it would always be in the patient’s best interest to have the foundation stabilized and balanced prior to or as a part of any treatment for the problem. In other words, if any treatment is needed for the patient, the best possible outcome will reside in the approach that builds a balanced foundation as the first step to care.
The objective examination of the patient for the location, timing, and extent of force imbalance must be accomplished whenever the patient exhibits positive findings for force-related problems on the history or physical examination. In the past, this required multiple visits and expense to develop a set of deprogrammed mounted study casts. This mounted study-cast procedure was cumbersome in that it required additional appointments with the patient to pinpoint the force-related problems.
USING T-SCAN TECHNOLOGY IN THE EXAMINATION PROCESS
The T-Scan system (Tekscan) can provide the dentist a timely (nearly instant) examination of the interdental forces in the patient that manifest force-related problems. The T-Scan also reflects the abnormal dysfunction of the musculature directly with electromyography synchronization or indirectly via the center of force patterns and the disclusion timing. The T-Scan then becomes the definitive diagnostic imaging of the force balance and function of the masticatory muscles. The information provided on a 2-minute T-Scan movie includes much useful diagnostic information (Table).
`Certainly many dentists use the T-Scan for efficient and effective occlusal adjustment procedures. However, the optimal and best use of the T-Scan system is in the diagnostic documentation of force-related problems at the time of examination. Patients can best understand their force-related dental disease and any sensorimotor-related pain and headaches when they can view the computerized force analysis of their own mouth. Every T-Scan movie tells a story about the dental foundation, and each story reveals the underlying cause for whatever may be the pathology that is present.
CLINICAL CASE EXAMPLE
The patient, whose photos are represented in Figures 1 to 3, presented for examination as a new patient. Her chief complaints were as follows: the bridge on the right side had never felt correct to her, her front teeth were chipping and looked unattractive, and she had a history of chronic daily headaches.
Examination revealed worn and fractured enamel on the incisal edges of the incisors, a bridge that needed replacement (a pontic for tooth No. 30), and multiple areas of attachment loss and abfractions lesions.
 |
 |
| Figure 1. Preoperative retracted smile: This reveals evidence of force-related dental disease: anterior wear, chipping, and misalignment of the teeth. Additionally, there are abfractions lesions and attachment loss on teeth Nos. 6, 11, and 24. | Figure 2. Preoperative maxillary occlusal view: This shows additional evidence of force related problems: multiple teeth with crowns, broken incisal edges on the anterior teeth, and narrow misalignment of the upper arch. |
 |
| Figure 3. Preoperative mandibular occlusal view: This shows force related problems in fractures around the margins of restorations on teeth Nos. 18 and 19, misalignment and wear on the lower incisors, missing tooth area No. 30, and poor anatomical contours of the restorations on the lower arch. |
Since all of these problems were likely to be “force” related, we wanted explore the possibilities and to maximize our ability to communicate with her by utilizing the T-Scan dental force analysis.
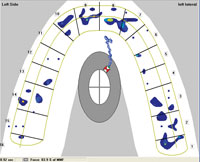
In Figure 4, we can demonstrate to the patient easily that there is a front-to-back force pattern. That was indicative of a tight envelope of function. It was explained to the patient that her muscles were working extremely hard to squeeze her lower teeth together with her upper teeth. Additionally, she was carrying 58% of the force on the right side of her mouth. This tight pattern and imbalance in the bite were perpetuating her headaches and causing her to feel like her teeth did not fit together correctly.
In looking at Figure 5, we showed the patient that 25% of all the force in her mouth was being borne by teeth Nos. 1 and 2 against Nos. 31 and 32. In Figure 6, we easily showed the patient that there were towers of excessive force on her right side in the anterior and back on her bridge.
Armed with this diagnostic information, the patient then easily accepted that a plan could be designed to balance her foundation, starting with the excess muscle activity. Her treatment program included several weeks of muscle rehabilitation, followed by a balancing of the dental forces. After her symptoms were resolved, then her restorative dentistry was accomplished in a predictable and comfortable program.
| Practice Management Ramifications of T-Scan Technology |
|
Amy Morgan |
DISCUSSION
Creating a balanced foundation involves more than just balancing forces. It means that we need to proceed down a path that will allow for the most symmetry of the muscles and joints as the initial focal point for care. This is what we call the “pathway to care.” This pathway to care refers to the development of an appropriate sequence to rehabilitate the musculature and the joints as we treat the patient’s symptoms. Much like an orthopedist must balance the rehabilitation of a patient’s muscles, ligaments, and joints with the development of a planned prosthesis, we must approach the most adaptable tissues first which are the muscles, then the joint rehabilitation, and finally we can complete any needed treatment of the teeth.
| Table. Diagnostic Information | ||||||||
|
This rehabilitative approach gives the appropriate time process to each patient depending on the extent of the injury and degree to which the condition has become chronic. Certainly, the patient who has an acute problem can go through a quick rehab assessment and move quickly to the dental restorative process. However, the patient who has a limited range of motion in the mandible or cervical spine will need more time to rehabilitate the musculature, thus minimizing pain and disability prior to dental restoration. In either case, rehabilitation is the mindset of dealing with dental foundation problems through the development of an appropriate pathway to care.
 |
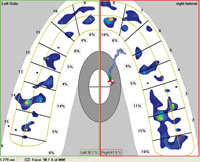 |
| Figure 4. Ts1 Scan: This shows the long center of force tail demonstrating the severe anterior to posterior dimension of closure forces and a very limited envelope of function. | Figure 5. Ts2 Scan: This demonstrates the severe right-sided force imbalance during closure with 25% of the force being borne by teeth Nos. 1 and 2 versus Nos. 31 and 32 during the closure cycle. |
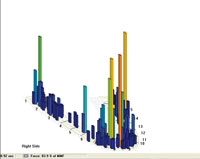 |
| Figure 6. Ts3 Scan: This reveals the “towers of force” that are evident in the unbalanced bite with excessive forces being recorded on the anteriors Nos. 8 and 9, and teeth Nos. 1 and 2. |
As a patient approaches the rehabilitation, we will often discuss the balancing of the foundation and the balancing of the bite. The balancing of the bite is the one piece of the rehabilitation process that can only be done by a dentist. This means that any patient who has a problem that resides in the teeth, muscles, joints, or in the trigeminal cervical nucleus must be cared for by a knowledgeable dentist to have the best opportunity for success.
Other medical professionals who treat some of these “foundation” problems can only achieve short-term success; this is because they cannot control the afferent signals from the teeth to the trigeminal cervical nucleus. This brainstem pathway (or column) carries all the information regarding headache, head and face pain, and neck pain to the patient’s thalamus and on to the cortex. Approximately 40% of the afferent control into this column comes from the area around the teeth and jaws. In other words, this is the domain of the dentist, and it is the dentist who has the systems to ultimately stabilize the rehabilitations that are necessary for this part of the body.
The essence of all force-related and pain-related pathology in the dental foundation is a dentomandibular sensorimotor dysfunction. All conditions that are mediated by, or dependent on, this major neurological system of the brainstem are interconnected via dendritic synapses that have developed within this trigeminal system of nuclei. As a result, all dysfunction of the mandible, upper 3 cervical vertebrae, and associated musculature, are associated with the somatosensory and sensorimotor neurology of the oral and dentomandibular regions. This, then, is the domain of the dentist.
Although many dentomandibular conditions have a “chicken or the egg” etiology, all therapy for dental foundation imbalance or bite imbalance must be approached comprehensively, dealing with all foundational elements to achieve success. The precise etiology of headache, migraine, head/face pain, or tooth wear is not as important to determine as is the understanding that the “stress in the system” must be managed through comprehensive rehabilitation of the muscles, joints, and teeth.
As dentists begin to “balance the bite,” they will proceed with balancing the forces around the arch through both additive and subtractive procedures. The process of balancing the bite is not a therapeutic end unto itself, but must be developed along with the symmetry and normalization of the condyles and the muscles. This will create and develop a balanced foundation through the rehabilitation process.
CONCLUSION
When all the elements of teeth, muscles, joints, neurology, pain, and force balance are addressed, the patient will have the best chance for an excellent outcome. This rehabilitative approach is the crux of a medical/dental synergy that is grounded in the neurology and neuroplasticity of the human brain, brainstem, and cranial nerves. The elements of the applied neurology of the afferent and efferent pathways that are involved with sensation, proprioception, pain, reflex motor control, and compensatory adaptations can be addressed with a pathway to care that includes a “force balanced occlusion.”
Dentomandibular sensorimotor dysfunction can be effectively managed with this straightforward, systematic approach.
Dr. Montgomery graduated from Oregon Health Sciences University in 1980. He is a member of the ADA, Oregon Dental Association, AGD, International Association of Orthodontics, and Academy of Comprehensive Esthetics. He was a founding faculty and director of education with PAC~live and the Hornbrook Group. He currently partners with Aesthetic Masters and University of Nevada Las Vegas School of Dental Medicine in live-patient hands-on curricula for postgraduate clinical studies. He also is a consultant with Pride Institute. He is on the faculty of Aligntech Institute, training dentists in the Invisalign system. He also is the founder of Cascade Aesthetic Masters Study Club in Oregon. He presents continuing education courses affiliated with the Aesthetic Masters Group in the areas of occlusion and full-mouth reconstruction. He can be reached at mark.montgomery@dentalresourcesystems.com.
Disclosure: Dr. Montgomery reports no disclosures.
Dr. Shuman is president of Pride Institute and is well known in the dental community for his leadership and expertise in the areas of strategic relations, emerging technologies, Internet strategy, practice management, and marketing. The Pride Institute’s goal is to utilize its reputation of integrity and fairness as a foundation in educating the community within the field of emerging technologies. He previously served as vice president of clinical education and then vice president of strategic relations for Align Technology for 7 years. He is a member of Dentistry Today‘s Dental Advisory Board and has been listed in Dentistry Today‘s Leaders in Continuing Education from 2004 to 2008, and he is currently listed as a Leader in dental consulting. He can be reached via e-mail at lshumani@msn.com. Follow Dr. Lou Shuman on Google+, on Twitter (@LouShuman) or subscribe to Lou Shuman’s posts on Facebook.
Disclosure: Dr. Shuman reports no disclosures.
Ms. Morgan serves as the CEO of Pride Institute. She is a dental consultant and international lecturer. Over the years, Ms. Morgan has facilitated the successful revitalization of thousands of dental practices using Pride Management Systems. She can be reached at amym@prideinstitute.com.
Disclosure: Ms. Morgan reports no disclosures.
{rscomments on}











