INTRODUCTION
There’s no question that Mother Nature makes the best teeth. Despite advances in dental implant surgery and in the implants and abutments themselves, they cannot replicate the sensory perception that the periodontal ligament of a natural tooth provides. What’s more, a natural tooth can better cope with lateral biomechanical forces. That’s one of the reasons why, as a periodontist, I strive to save a patient’s natural dentition whenever appropriate and when I am confident that my surgical and nonsurgical periodontal disease treatment will be successful.
The question, “Should I treat and preserve or should I extract and place an implant?” is best answered via evidence-based assessment and treatment planning, which begins with gauging the expectations and commitment level of your patient.
For example, if a patient comes in and says, “I want to do anything possible to save my natural teeth,” chances are you will get a high level of compliance for long-term periodontal treatment, at-home oral care, and continued periodontal maintenance.
Equally important is a patient’s willingness to undergo, and ability to afford maintenance therapy every 90 days. This is critical to achieving positive patient outcomes, because the maturation of bacterial plaque occurs within 90 days and the patient becomes disease-active again.1
But when your patient makes statements such as “I hate going to the dentist,” or “I’ll never do that again,” it’s a definite red flag. If they say, “My insurance only pays for 2 cleanings a year,” that’s another warning sign. The bottom line is this: you can be a superstar in intricate periodontal procedures and grow bone in places where no other dentist can, but if you keep getting long-term treatment and insurance coverage objections, your success is unlikely.
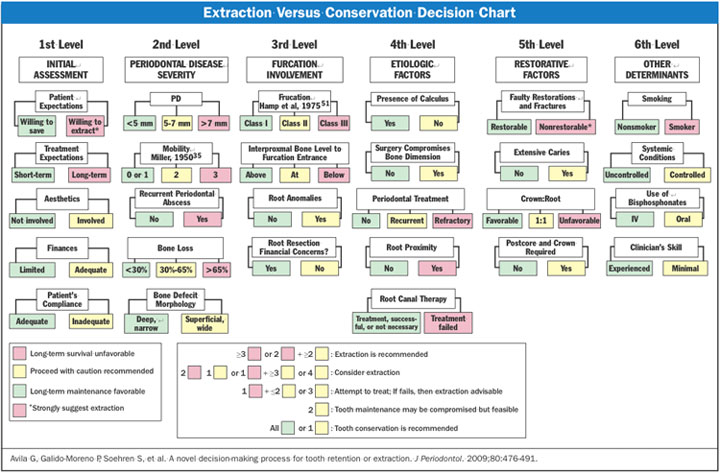 |
| Figure 1. Extraction versus conservation.3 |
Unfortunately, many specialists and general practice dentists alike are becoming “quick to extract.” Part of this is due to a 2-pronged campaign by the implant manufacturers. On one front, they wine and dine dentists and provide free training and continuing education credits. On the second front, they blitz the consumer media with the promise of “teeth in a day.”
The consumer marketing is prompting more and more patients to request implants rather than long-term therapy. What they don’t realize is that dental implants are not a “set it and forget it” solution; peri-implantitis has a prevalence rate ranging from 11.3% to 47.1% of implant patients.2
 |
 |
| Figure 2a. Preoperative radiograph of tooth No. 19. | Figure 2b. A residual pocket depth of 7 mm existed on the distal of tooth No. 19. |
 |
 |
| Figure 3a. Implant tooth No. 30. | Figure 3b. Implant crown. |
These are the major factors influencing clinicians and patients alike in opting for extraction and implants rather than preserving natural dentition. But even if a patient is ready, willing, and able to do whatever it takes and whatever it costs to save his or her teeth, further evidence-based analysis must be conducted to determine which course of treatment is truly best for the patient.
It takes a lot of patient education to offset the “teeth in a day” hype, and this is best achieved by forging strong relationships between general dentists and periodontists, who, in turn, need to maintain a united front in explaining treatment options to their comanaged patient in an objective manner, and work together toward the common end result of a positive patient outcome.
In my practice, I refer to the “Extraction Versus Conservation Decision Chart” developed by Avila et al3 to assess the patient’s condition and predict whether or not long-term periodontal therapy will be successful, or, in the patient’s eyes, an uncomfortable waste of time and money (Figure 1).
The decision chart contains 6 levels of detailed analysis for the following principal areas of assessment:
- Initial assessment
- Periodontal disease severity
- Furcation involvement
- Etiologic factors
- Restorative factors
- Other determinants.
As you can see, each of these principal areas contains several subcategories of analysis that are weighted and averaged to help the clinician determine 3 main evidence-based conclusions:
- Long-term survival: unfavorable
- Proceed with caution: recommended
- Long-term maintenance: favorable.
Decision chart analysis leading to conclusion No. 1 would strongly suggest extraction. No. 2 indicates that treatment is feasible; but if it fails, extraction is advised. Conclusion No. 3, although alluding to a positive outcome, may default to No. 1 if the patient rejects the treatment plan for financial or other reasons.
This decision tree chart was used to evaluate the patient and ultimately plan and perform the following case scenario.
| The Single Implant Crown | ||||||||||||||||||||||||||||||||||||||||||||
|
Tom M. Limoli Jr The most common of all dental implant procedures is by far the endosteal. According to CDT, procedure code D6010 includes the surgical placement of the implant body, the second stage surgery, and the placement of the healing cap. The global aspects of this procedure code encompass all 3 completed subcomponents. In other words—D6010 is not completed until the implant is stable and ready to be loaded. Of question with procedure code D6010 is the concept of the second stage (or pre-abutment placement) surgery. It is at this point where the doctor surgically exposes the implant head so as to test and confirm the integration of the bone to the implant. At this visit, the original surgeon who placed the implant body may (or may not) place either a healing collar or tissue contouring provisional abutment. This is the area of confusion because procedure code D6010 is not yet complete until the tissue surrounding the implant is structurally as well as aesthetically ready for the actual abutment that will retain the prosthesis. Depending upon your desired endosteal implant system of choice, the second surgery may or may not be necessary. Confused yet? With confirmation that the implant body has sufficiently bonded with the bone, the abutment (if necessary) is now ready to be placed in anticipation of the final prosthesis. The analog transfer process of selecting and/or modifying the abutments intended path of prosthetic insertion is all part of either procedure code D6056 (prefabricated) or D6057 (custom). Also, the direct cost of any post surgical custom impression trays as well as soft-tissue models; along with any other miscellaneous assortment of screws, nuts, bolts, washers, gaskets or socket wrenches; are all encompassed within your singular fee that you charge for either the prefabricated or customized abutment. Remember, it’s one code or the other and never both. This leaves us now with coding, billing, and reimbursement for the final prosthesis. If the abutment, retainer and/or implant are supporting a single-unit crown, that crown will have the same fee as any other more traditionally placed crown. The same can be said for multiple units of a fixed partial denture or bridge. The fee is the same provided you have charged appropriately for either D6056 or D6057.
|
EVIDENCE-BASED CASE REPORT
Diagnosis and Treatment Planning
The patient, a 53-year-old white female, presented to my office requesting a comprehensive care program so that she could get re-established in a periodontal cleaning regimen. Her medical history was noncontributory. She takes no medications, some vitamins, and has no drug allergies. Her social history is negative for smoking, and she consumes 3 to 4 alcoholic beverages per week.
Her previous dental history includeed periodontal surgery in the lower quadrants, and nonsurgical therapy in the upper quadrants. Bone grafts were placed in a few areas in the lower molar areas. She has had no maintenance therapy in more than one year. Her initial periodontal exam revealed heavy subgingival calculus ,especially in the posterior areas.
Radiographs indicated that there was generalized horizontal bone loss in the maxillary arch ranging from 10% to 30%, and an isolated vertical defect on the distal of tooth No. 19. Tooth No. 19 had been grafted about 3 years prior to my examination. A residual pocket depth of 7 mm existed on the distal of No. 19 (Figures 2a and 2b).
Tooth No. 30 had been extracted almost 2 years ago, after being deemed hopeless by her previous periodontist. The patient reported that the tooth was not doing well periodontally, and her dentist thought it was also cracked, which was confirmed after extraction. The patient knew that she needed additional periodontal therapy, and also agreed to have tooth No. 30 replaced with a dental implant and PFM crown.
Treatment Protocol
Conventional periodontal osseous surgery was performed in the upper arch, scaling and root planing was administered with hand and ultrasonic instruments with the addition of local delivery antibiotics in No. 19 (Arestin) and a dental implant (Straumann Tissue Level SLActive) was placed in the position of tooth No. 30 (Figures 3a and 3b).
The patient and I discussed the importance of a 3-month maintenance interval to control her inflammatory response. Tooth No. 19 will continue in maintenance therapy that will include scaling and root planing and may require additional surgical therapy depending on whether probing depths increase, there is persistent bleeding upon probing, or radiographic evidence of decreased bone mass levels.
Closing Comments
The patient is enthusiastic about keeping her remaining teeth, even with the potential for additional surgical therapy.
This brief case report article provides an example of how treatment decisions are made in a periodontally compromised dentition. We should always refer back to the evidence in the existing literature, and perform regular thorough examination of our periodontitis patients.4
References
- Cohen RE; Research, Science and Therapy Committee, American Academy of Periodontology. Position paper: periodontal maintenance. J Periodontol. 2003;74:1395-1401.
- Koldsland OC, Scheie AA, Aass AM. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J Periodontol. 2010;81:231-238.
- Avila G, Galindo-Moreno P, Soehren S, et al. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80:476-491.
- American Academy of Periodontology. Comprehensive periodontal therapy: a statement by the American Academy of Periodontology. J Periodontol. 2011;82:943-949.
Dr. Masters earned her dental degree from The University of Texas Health Science Center at San Antonio (UTHSCSA) and continued her education at the dental school with a 3-year specialty program in periodontics. She is a board-certified periodontist whose expertise is in the diagnosis and treatment of all types of gum diseases and performing both aspects of surgical and nonsurgical therapy. She is certified to use several types of sedation to alleviate anxiety in patients concerned about their surgical therapy. Dr. Masters is a member of the American Academy of Periodontology, the International Congress of Oral Implantologists, the American Dental Association, Southwest Society of Periodontists, and the Texas Society of Periodontists. She is also a clinical associate professor at the UTHSCSA Dental School. She can be reached at mastersdds@mdgteam.com.
Disclosure: Dr. Masters reports no disclosures.



