INTRODUCTION
For a long period of time, direct posterior composite restorations have enabled clinicians to provide patients with minimally invasive and aesthetic restorations as an alternative to amalgam fillings. However, since the introduction of direct composites, clinicians have faced a variety of challenges associated with the placement of these materials in handling, wear, longevity, and aesthetics.1 Direct posterior composite placement has typically required strict attention to one’s individual operative techniques to ensure complete polymerization, great marginal seal, and no postoperative sensitivity. Due to their polymerization properties and limited depth of cure, light-cured composites are generally used in a layering technique with individual increments that are up to 2.0 mm in thickness.2,3 Each increment is polymerized separately, with light exposure times ranging from 10 to 40 seconds per surface, depending on the power of the curing light and the color/translucency of the composite material. With the materials available up until recently, thicker composite layers resulted in insufficient polymerization of the composite resin, which resulted in inferior mechanical and biological properties.4
Today’s practitioners must be able to effectively carry out all the required operative steps to successfully complete direct composite resin restorations. If these steps (eg, isolation, adhesion, composite placement, and light curing) are done correctly, the risk of premature composite resin failure is a moot point.1 In addition, these steps must be completed as efficiently as possible to contend with issues such as practice overhead or low insurance reimbursement. Efficiency in an everyday dental practice should be considered as not only the ability of the operator to work quickly but also competently. Overhead costs in most practices require that material and technology advancements are introduced so that posterior composites can be placed faster, easier, and more profitably without any compromise in the clinical procedures.
 |
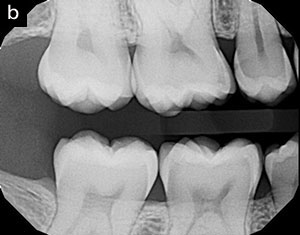 |
| Figure 1. A preoperative image (a) and radiograph (b) depicting interproximal decay on the molar and premolar. |
The Bulk-Fill Option
Understanding the needs of clinicians, a number of composite manufacturers have focused on material development to simplify composite-based restoration techniques in the posterior region. In these new fast-track systems, low-shrinkage, mechanically stable composite materials that can be applied directly into the cavities in larger increments have been developed. One product in this arena that I am now using on a daily basis is Bulk EZ (Zest Dental Solutions). Bulk EZ is a dual-cure, bulk-fill restorative composite designed for direct restorations. It is versatile and can be used as a direct restorative and also as a flowable base/liner. When allowed to self-cure (with no light curing), this bulk-fill composite has excellent physical properties for posterior restorations with an unlimited depth of cure. Light curing is only needed to harden the air-inhibited layer after self-curing. With no layering required, the time saved over other light-cured bulk-composite systems can be as much as 60% per procedure. Unlike other dual-cure composites, Bulk EZ is compatible with all other bonding agents on the market.5 The directed shrinkage in this self-curing composite offers the solution to the common concern of complete polymerization in the deepest portions of box preparations.6,7 When properly placed, voids or gap formation at the bottom of the restoration are virtually eliminated due to the low viscosity and exceptional marginal adaptation of the material, resulting in a decreased risk of post-op sensitivity or recurrent decay. Unlike many other bulk-fill composites, Bulk EZ is available in 3 VITA shades: A1, A2, and A3.
CASE REPORT
Diagnosis and Treatment Planning
A 28-year-old female, in good overall health, presented for a routine periodical oral examination and radiographs. It was determined visually and radiographically (Figure 1) that interproximal decay was present on her upper first molar and second premolar. Having been informed of the possible treatment alternatives and their costs, the patient elected to have direct restorative composite restorations placed.
 |
 |
| Figure 2. A selective etching technique using 35% phosphoric acid gel (Ultra-Etch [Ultradent Products]) was utilized to enhance enamel bonding. |
Figure 3. Application of the universal adhesive (Prelude One [Zest Dental Solutions]) requires agitation or a scrubbing motion for 20 seconds. |
 |
 |
| Figure 4. Keeping the metal cannula submerged in Bulk EZ (Zest Dental Solutions) during placement helps to decrease the chance for voids within the material. | Figure 5. With Bulk EZ in place, full polymerization will occur in 90 seconds. |
 |
 |
| Figure 6. The occlusion was checked to verify proper occlusal contacts. | Figure 7. The final restorations in place, showing proper finish and ideal contacts. |
Clinical Protocol
The patient was anesthetized with one carpule of 4% Articaine (Septodont) with 1:100,000 epinephrine. Isolation under a r
ubber dam setting would have been preferable; however, due to the patient’s intolerance, we utilized a Mr. Thirsty (Zirc Dental) to achieve our optimal working environment. The preparation was completed using high-speed (#330 bur) and low-speed (#4 round bur) handpieces, making sure that any residual amalgam stains were removed.
The prepared cavities were then demarcated using a sectional matrix system (Mega V Ring System [Zest Dental Solutions]). Once the matrix system was in place, a ball burnisher was used in a buccal-lingual motion to ensure adequate contact would be obtained. A universal adhesive (Prelude One [Zest Dental Solutions]) was used for the bonding procedure. In conjunction with the bonding agent, it was decided to incorporate a selective etching technique (Figure 2). Due to the inherent lower pH of the universal adhesives in comparison to phosphoric acid, it is always advisable, in my opinion, to apply phosphoric acid to the enamel cavosurface margin to maximize micromechanical interlocking of the composite material at the enamel surface. A 35% phosphoric acid gel (Ultra-Etch [Ultradent Products]) was placed on the enamel margins of both teeth for 15 seconds. The acid was then thoroughly rinsed off with the air/water syringe for approximately 10 seconds. Excess water was carefully removed from the cavity preparations using air without desiccating the dentinal surfaces. A generous amount of the Prelude One universal adhesive was applied to each preparation using an agitated/scrubbing motion for 20 seconds (Figure 3). The solvent was then gently air dried with oil-free air for 10 seconds or until the film of solvent could no longer be seen moving along the preparation surface. The adhesive was then light-cured for 10 seconds with a light source greater than 800 mW/cm2. The result should be a shiny cavity surface, evenly covered with adhesive. This should be carefully checked, as any areas of the cavity that appear matte in appearance are an indication that insufficient adhesive was applied to those sites. In the worst case, this could result in reduced bonding of the restoration in these areas and, at the same time, in reduced dentin sealing, which may lead to post-op sensitivity. If such areas are found upon visual inspection, additional bonding agent is again selectively applied and light cured as described previously.
The Bulk EZ composite was introduced into each preparation, starting from the deepest portion of the preparation and working my way out toward the occlusal (Figure 4). An important technique point here is the need to keep the applicator tip embedded into the material at all times to help eliminate voids. Once the cavosurface was reached with the proper amount of material, the timer was set for 90 seconds (Figure 5). It is important to not utilize a curing light at all during this 90-second time frame. Simply sit and wait at this point, allowing the material to self-cure; as it sets, the polymerization shrinkage will be directed toward the previously bonded walls of the restoration. Prematurely utilizing a curing light will defeat the purpose of Bulk EZ and its patented IntelliTek Technology. Rather, this is the time to begin to form your general tooth anatomy, if so desired. Personally, I like to slightly overfill and then perform a subtractive technique using carbide and/or diamond finishing burs. After 90 seconds, the sectional matrix band was removed, and light curing of the restorations from buccal, lingual, and occlusal directions for 10 seconds each was performed; this is to help accelerate polymerization.
After removal of the isolation device, the restoration was carefully adjusted with rotary instruments and abrasive discs to ensure proper occlusion form and function (Figure 6). Diamond-impregnated silicone polishers (Enhance Pogo Polishers [Dentsply Sirona]) were then used to make the surface of the restoration smooth and shiny. The restorations reproduced the original tooth shape with an anatomically shaped marginal ridge, proper interproximal contacts, and an aesthetically acceptable appearance (Figure 7).
CLOSING COMMENTS
Although there are numerous composite materials available on the market, each of which can be reliable for specific indications, the material characteristics of Bulk EZ have provided a breakthrough in the placement of direct posterior composite restorations. While possessing the requirements of a posterior composite to withstand daily masticatory forces, this dual-cure bulk-fill composite also provides dentists with a straightforward and reliable procedure while eliminating the challenges associated with conventional composites.8 Its material properties and simplified placement allow clinicians to provide long-lasting, predictable, and aesthetically pleasing restorations quickly and easily.
References
- Christensen GJ. Advantages and challenges of bulk-fill resins. Clinicians Report. 2012;5:1-6.
- Feilzer AJ, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res. 1987;66:1636-1639.
- Giachetti L, Scaminaci Russo D, Bambi C, et al. A review of polymerization shrinkage stress: current techniques for posterior direct resin restorations. J Contemp Dent Pract. 2006;7:79-88.
- El-Damanhoury H, Platt J. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Oper Dent. 2014;39:374-382.
- Vandewalker JP, Casey JA, Lincoln TA, et al. Properties of dual-cure, bulk-fill composite resin restorative materials. Gen Dent. 2016;64:68-73.
- Moorthy A, Hogg CH, Dowling AH, et al. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012;40:500-505.
- Kim RJ, Kim YJ, Choi NS, et al. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent. 2015;43:430-439.
- Zimmerli B, Strub M, Jeger F, et al. Composite materials: composition, properties and clinical applications. A literature review. Schweiz Monatsschr Zahnmed. 2010;120:972-986.
Dr. Schmedding has been a practicing cosmetic and restorative dentist for the last 25 years. He is a 1993 honors graduate from the University of the Pacific, Arthur A. Dugoni School of Dentistry. He currently maintains a private practice in Walnut Creek, Calif. He is an Accredited Member in the American Academy of Cosmetic Dentistry and Diplomate of the American Board of Cosmetic and Esthetic Dentistry. Dr. Schmedding works with numerous manufacturers on the implementation and testing of various restorative products being brought to market. He speaks and teaches nationally and internationally on both aesthetic and restorative dentistry. He can be reached at troy.schmedding.dds@gmail.com.
Disclosure: Dr. Schmedding has received an honorarium for this article from Zest Dental Solutions.
Related Articles
Q&A: Today’s Restorative Dentistry With Dr. Troy Schemdding
Intraoral Repair of Multiple Substrates Using Silication
Technique and Materials for Predictable and Accurate Crown and Bridge Impressions


