INTRODUCTION
Around 1896, Dr. G.V. Black published a standardized set of cavity preparations for amalgam. Gold preparations of the day were a slight deviation from those amalgam preparations: They featured lightly beveled margins and divergent walls for paths of insertion for indirect and solid restorations that needed to be inserted and cemented. Starting in about 1950, Dr. Richard Tucker was mentored by Dr. George Ellesperman and, later, Dr. Gerald Stibbs. During this period, Dr. Tucker continued to perfect his preparations and his gold casting technique. Recognizing that the finest margin was that of a gold foil, he strived to achieve that in his casting and finishing techniques,1 transforming the gold restoration outcomes beyond those of his mentors. In Figures 1 to 3, we see the work of Dr. Tim Hess, a Tucker Gold Study Club member and director of the Tucker Institute Seattle.2,3 His prep has a Calla Lily-style flare on the occlusal and a radius wall on the interproximal. The postoperative size of the external surface area of the gold restoration is easily double that of the amalgam restoration that was replaced. In the interproximal, the walls are flared beyond the confines of the contact area. Dr. Tucker changed the preparations in a dramatic way to maximize the benefits of gold.
When I recently interviewed Dr. Richard Tucker’s son, Dr. Dick Tucker, he explained the reasons behind his father’s fairly dramatic flaring of the walls in the Tucker Class II restoration. The first reason was to move the tooth-restoration interface (TRI) toward the line angles so the gold could be swaged to “close” the margins to make it act more like gold foil. The second was to move the TRI into a place where it was more self-cleansing. Very few clinicians, in the past and likely in the future, have questioned his wisdom or the sacrifice of the minimal healthy tooth structure required to accomplish these goals.
 |
 |
| Figure 1. Preoperative view of a broken amalgam restoration and a fractured marginal ridge. (Image courtesy of Dr. Tim Hess, Seattle.) | Figure 2. A Tucker-style gold inlay cavity preparation with an aggressively flared Tucker-style cavity prep design. (Image courtesy of Dr. Hess.) |
 |
 |
| Figure 3. Polished and seated casting. The Clark Class II composite cavity preparation and restoration shown later in this article have significant similarities to this Tucker Gold masterpiece. (Image courtesy of Dr. Hess.) |
Figure 4. Randomly selected extracted teeth show typical decalcification and cavitation patterns. Two things are apparent to even a casual observer: First, that putting a margin (tooth-restoration interface) within this disease zone does not make much sense, and, secondly, that the decalcification area that extends far beyond the cavitation zone begs for a flared “Tucker-esque” wall, not a 90° cavity wall. |
 |
 |
| Figure 5. Pre-op view with subtle dark caries visible through the translucent enamel. Lumpy natural contact is apparent. It has been the author’s experience that natural contacts that are point contacts or, in this case, irregular with concavities are the most prone to decay. A Class II restoration is a treatment of disease specific to the contact area. The creation of broad and full contacts with rounded occlusal embrasures should be of the highest priority. | Figure 6. An integral step of modern composite dentistry is to place disclosing solution (Bioclear Dual Color Disclosing Solution) on the dried teeth after placing the rubber dam but before placing the pre-wedge(s). At the Roseman University of Health Sciences College of Dental Medicine, where the Clark Class II restoration is taught in full, disclosing solution is actually placed by the students in the simulation lab on plastic teeth to reinforce the importance of this step. You cannot treat what you can’t see. |
 |
 |
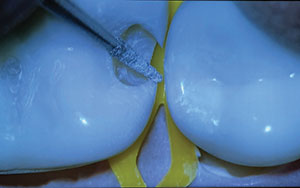
| Figure 7. The widespread biofilm, now easily visible with the bright stain, must be carefully removed before injection molding because modern extension for prevention means the composite will be purposefully extended for several millimeters, when appropriate, beyond the “margin” of the cavity preparation. | Figure 8. The next step is pre-wedging with the largest Diamond Wedge (Bioclear). All the Diamond Wedges are the same height. This blue, extra-large Diamond Wedge is short and squat, allowing for maintenance of the trademark aggressive curvature of the Biofit Matrix (Bioclear). |
 |
 |
| Figure 9. Once initial penetration is made to discover caries with a tapered diamond bur (#6856 FG 018 [Komet]), not shown here), the preparation is moved toward wherever the DEJ caries extends. This terminates the prescriptive portion of the Clark Class II, and the organic caries removal portion then begins. The contact is never broken with the large bur as this can lead to the very common problem of iatrogenic gouging of the neighboring tooth. | Figure 10. A safe-sided metal strip (such as the Miltex Lightning Metal Strip) can be used to safely begin to open the contact areas. |
Benefits of the Cavity Design Attributed to Dr. Tucker
A review of the outcome studies on teeth restored with gold finds that survival rates are wildly inconsistent. Of 2 contrasting studies, one showed a 50% failure rate at 7 years,
In this article, the author proposes that the cavity shapes of the Tucker gold restoration are of profound importance. Whether by design or accident, Dr. Tucker created 3 important benefits that went far beyond his intentions to compensate for the limitations of path of insertion of a gold casting.
1. The aggressive cavosurface occlusal flared walls “turn” the preparation so that the primary strike point of the opposing tooth is close to 90° angle to the TRI instead of parallel to the TRI. This protects the margins from opening up during finishing and after decades of occlusion.
2. The shape and exaggerated volume of the cavosurface area generated a partial compression joint (a Calla Lily-style occlusal shape) and, in larger occlusal gold restorations, a full compression joint with an invisible gold onlay, both of which have shown remarkable resistance to tooth fracturing in the same way that a crown splints a cracked tooth. Tucker put the entire tooth-restoration complex into partial compression.
3. Tucker’s radius walls (flaring) in the interproximal increased the enamel-gold interface, protecting the more vulnerable dentin-gold interface inside and distancing the outside robust seal of enamel from the less robust dentin seal. This is especially critical when selective caries removal (Modified Hall Technique) is practiced. One of today’s sad realities is that many endodontists scoff at restorative dentistry’s movement toward selective caries removal because they do not believe that today’s general practitioners can achieve a long-term restorative seal with composite, especially in the interproximal. The skeptical endodontist says, and I quote, “These composite restorations are all going to leak, so let’s just do the endodontics now.”
Similarities of the Tucker Gold Prep and Clark Class II Cavity Prep Designs
In Figure 4, we see a lineup of extracted teeth with interproximal caries progression that is different than caries progression in the G.V. Black era. This is attributed to the widespread use of fluoride-containing dentifrices and readily available fermentable carbohydrates in today’s diets. There is no good place to put a traditional margin within the traditional confines of the contact area. The same gentle extensions that benefit the Tucker gold prep benefit the Clark Class II for composite resin as well.
 |
 |
| Figure 11. The contacts on the buccal and lingual are broken with the blunt needle diamond bur (#FSD3F FG 008 [Komet]). Enamel cuffs are modified to a convex radius wall where the most external portion of the wall becomes tangential to the untouched tooth surface. | Figure 12. The same bur (#FSD3F FG 008) can be brought from the facial and lingual to remove the “smiley face” decalcification that was demonstrated in Figure 4. In this case, the author also did an “opportunistic” access cavity prep on the neighboring tooth as decalcification and a small cavitation were present there. This allows the luxury of not cutting through the marginal ridge of one of the teeth. |
 |
 |
| Figure 13. Once the cavity preparations are finished, a Bioclear Blaster is used to remove biofilm for the infinity edge areas beyond the cut parts of the preparation, where stubborn biofilm can ruin adhesion. (Note: The phosphoric acid used to etch the enamel does not remove biofilm.) | Figure 14. Occlusal view of a Clark Class II on the first bicuspid and an opportunistic access on the second bicuspid. The jagged shape of the neighboring tooth was flattened with a Sof-Lex XT (3M) coarse disc or discs before restoring both teeth. This led to a larger space between the teeth at buccal and lingual line angle areas. |
 |
 |
| Figure 15. An opportunistic access on the neighboring tooth was injection molded with Filtek Bulk Fill Flowable Restorative (3M). No paste composite was necessary in this area because there were lower stresses on this novel restoration as it was below the contact and completely out of occlusion. | Figure 16. Once the opportunistic access was restored and polished, the Biofit Bicuspid Matrix (Bioclear) was seated and evaluated. Note the aggressive emergence profile. The clear matrix is crucial for both bulk filling for a full 5.0-mm depth of cure via 3-point curing and the ability to inject and light cure the composite all the way to the edge of the matrix for a perfect, long infinity edge. |
 |
 |
| Figure 17. The initial look showed a bit of a point contact because of the unique challenges resultant from flattening the jagged shape of the neighboring tooth. Premolar TwinRing (Bioclear) provides powerful separation, which is crucial when using a strong, stiff matrix such as the Biofit HD matrices (Bioclear). | Figure 18. Two dots of Filtek flowable composite were placed after etching and adhesion but before injection molding. These uncured “spot weld” spots would be light cured momentarily. |
 |
 |
| Figure 19. The Push/Pull instrument (Bioclear, patent pending) applies lateral pressure to create a tight contact; plus it expands the matrix buccal-lingually for a broad contact. This is a more modern version of burnishing. Burnishing was a common compromise necessary with metal matrices that lacked appropriate shapes. |
Figure 20. A less magnified view of the Push/Pull instrument. Once the matrix is expanded and pressure is applied laterally to oppose the matrix against the neighbor, the dental assistant cures the dots of flowable, which locks in a tight and wide contact of the matrix against the neighboring tooth. |
 |
 |
| Figure 21. Magic Mix (Bioclear) was utilized in a disposable prophy cup. Because the Bioclear restorations wrapped around much larger areas of the tooth, more robust and better-shaped polishers and system were needed. | Figure 22. The RSP (Rock Star Polisher [Bioclear], which is a diamond-impregnated, reusable cup) creates a brilliant finish. The mirror finish of Bioclear restorations can be compared to the beautiful luster imparted to Tucker Gold restorations. |
 |
| Figure 23. A postoperative view of the restored opportunistic access prep on the second bicuspid and Clark Class II on the first bicuspid. Broad contacts in buccal-lingual and occluso-gingival dimensions, rounded floss-friendly occlusal embrasures, fracture-resistant engineering, and glassy smooth surfaces lead to a great patient-centered outcome. |
In Figures 5 to 23, we see the Clark Class II cavity preparation has a very similar look to the flaring of the Tucker gold Class II restoration. Because of the author’s exposure to Dr. Tucker as a University of Washington alumnus, it is likely that, when he redesigned the Class II for composite, the design that he came up with did not seem as foreign to him as it can appear to many G.V. Black or strict slot prep aficionados. After introspection, the author feels credit should be given to the late Dr. Tucker for his inspiration in designing the optimization of shaping present in the Clark Class II posterior composite cavity preparation design.
Findings of a Retrospective Outcome Study and Finite Element Analysis
Can we ever hope to achieve the outcomes of a Tucker or Hess gold inlay with composite? The more important question is, are we willing to at least try? In the author’s practice, a retrospective outcome study of Clark Class II composite restorations restored with the Bioclear method between 2007 and 2013 is being done. Thus far, of the 300-plus teeth recalled, an 87% survival rate of these non-retentive, infinity edge, compression-based restorations that are between 5 to 12 years of service is being observed. Just as important, the Finite Element Analysis studies done at the Minnesota Dental Research Center for Biomaterials and Biomechanics is confirming what we are clinically seeing: that teeth can actually be splinted (to avoid fracturing or to splint a cracked tooth) with compression-based composite resin restorations.
IN CONCLUSION
Survival of the tooth and its restoration should be the ultimate goals. When a tooth with a standard composite prep breaks in half some years later, that is a failure of the procedure.
The author offers gold restorations to patients, and, occasionally, they say yes. That’s a win. A close second should hopefully be an injection-molded Clark Class I or Clark Class II composite that can last for decades and protect the tooth from fracturing.
References
- McKay T. In memoriam. Oper Dent. 2016;41:229-232.
- Hess TA, Wadhwani CPK. The Tucker technique: conservative molar inlays preserving the transverse ridge. Oper Dent. 2012;37:93-97.
- Hess TA. The Tucker technique: the proximal hollow grind to address a root concavity. Oper Dent. 2014;39:454-459.
- Tucker RV. Why gold castings are excellent restorations. Oper Dent. 2008;33:113-115.
- Crabb HS. The survival of dental restorations in a teaching hospital. Br Dent J. 1981;150:315-318.
- Donovan T, Simonsen RJ, Guertin G, et al. Retrospective clinical evaluation of 1,314 cast gold restorations in service from 1 to 52 years. J Esthet Restor Dent. 2004;16:194-204.
Dr. Clark maintains a private practice in Tacoma, Wash, and is the founder of the Academy of Microscope Enhanced Dentistry. He is also a course director at the Newport Coast Oral Facial Institute in Newport Beach, Calif, and director of the Bioclear Learning Center in Tacoma. Dr. Clark’s main areas of interest include the redesigning of restorative preparations and endodontic access preparations. He can be reached at the website bioclearmatrix.com.
Disclosure: Dr. Clark is the owner of Bioclear Matrix Systems.
Related Articles
The Seven Deadly Sins of Traditional Class II Restorations
The Injection Molded Class II Restoration
Focus On: Patient-Centered Outcomes


