INTRODUCTION
Dental implants are generally considered a safe and highly predictable surgical procedure performed by many clinicians with the aim of replacing missing teeth. Yet, to this day, a number of implants placed in adequate bone volume are lost each year within a 2- to 8-week period following implant placement for unexplained reasons. As society continues to consume lower-quality foods and rely more heavily on fast foods, a large percentage of today’s population is increasingly demonstrating generic vitamin deficiency upon testing, owing to this lack of nutritional intake. These deficiencies are even more pronounced in the aging population, where a greater percentage of dental implants are placed. Unfortunately, one of the most prominent deficiencies known to mankind is that of vitamin D, a water-soluble vitamin critical for proper immune function as well as bone homeostasis.
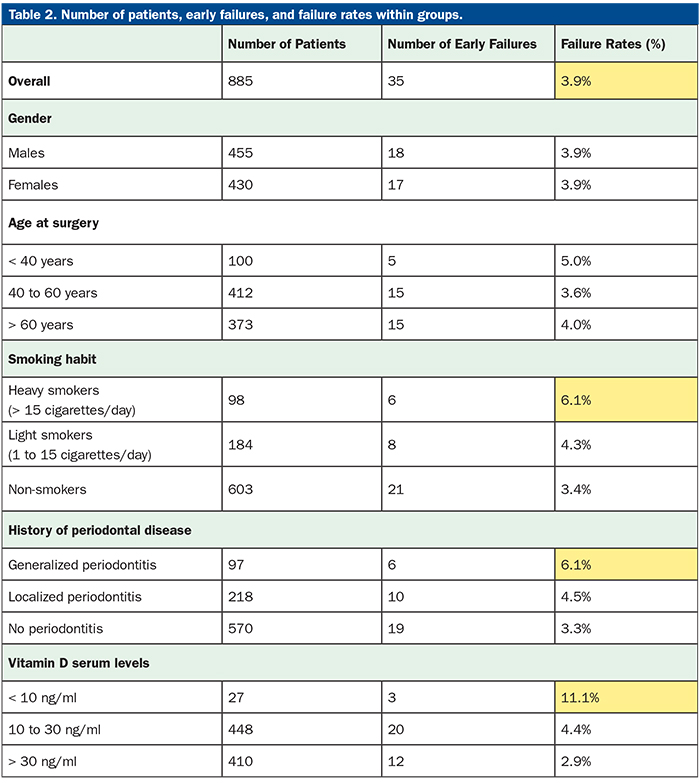
Over the past decade, vitamin D deficiency has been observed in ~70% of the population and particularly in postmenopausal osteoporotic women, for whom vitamin D is commonly prescribed (with various co-factors, such as vitamin K) with the aim of further optimizing bone density and halting disease progression. Interestingly, recent dental implant studies have found that while smoking and generalized periodontitis are generally associated with an approximate 50% to 200% increase in dental implant failure, vitamin D deficiency is associated with up to a 300% increase in early implant failure. These shocking findings further highlight the fact that systemic health, including adequate intake of vitamins and minerals, play a critical role in biomaterial/dental implant integration.
The aim of this article is to briefly present recent research on the prominent links between vitamin deficiencies (particularly vitamin D) and early implant failure. Thereafter, a very quick and easy in-office testing kit for vitamin D is presented that utilizes a simple finger-prick test similar to glucose testing (10 minutes total for testing). Lastly, supplementation guidelines and recommendations from the American Association of Clinical Endocrinologists (AACE) and the American College of Endocrinology (ACE) are presented for deficient patients with the aim of minimizing early implant failure potentially caused by vitamin deficiencies.
Vitamin D Deficiency
Vitamin D deficiency is a worldwide public health problem that spans across all age groups from children to adults. Naturally, as we age, our ability to absorb vitamin D is also decreased. The major source of vitamin D is directly from sunlight exposure along with the very few foods that naturally contain sufficient doses. Unfortunately, direct sunlight has tremendously decreased in modern society with the increased number of desk-related jobs. Epidemiological studies have now shown that roughly 70% of society is deficient.1
 |
Vitamin D deficiency is most known for its association in osteoporotic and menopausal women. Few realize, however, its drastic and substantial role in various other diseases. These include depression, dementia, Alzheimer’s disease, asthma, cancer, cardiovascular disease, and diabetes, among others. Vitamin D is essential for gastrointestinal calcium absorption, mineralization of osteoid tissue, and maintenance of serum-ionized calcium levels. It is also important for other physiological functions, such as muscle strength, neuromuscular coordination, hormone release, and immune cell function.2 More recently, vitamin D deficiency has also been linked with up to a 300% increase in dental implant failure, and associations with other dental-related complications are increasing.3-12 Optimizing vitamin D levels prior to surgery, therefore, becomes fundamental for maximizing wound healing, and this article aims to discuss the relevant research on the topic and its association with dental implant-related failures and bone grafting complications.
Optimizing Vitamin D Levels
Serum 25-hydroxy vitamin D (25-OH) is the reliable marker of vitamin D status, and a level below 20 ng/ml defines deficiency. Optimal levels above 30 ng/ml are required to maximize the bone health and non-skeletal benefits of vitamin D (Table 1). For individuals undergoing any type of dental-related procedures, levels between 40 and 60 ng/ml are generally recommended since it is known that levels may decrease substantially following a period of stress (simply, a dental surgical intervention). Unfortunately, foods do not contain sufficient levels. Examples are cod liver oil (400 to 1,000 IU/teaspoon); fresh-caught salmon (600 to 1,000 IU/3.5 oz vitamin D3); tuna (236 IU/3.5 oz vitamin D3); egg yolk (20 IU/yolk vitamin D3 or D2); and fortified milk, cheese, or yogurt (100 IU/3 oz, usually vitamin D3). These are low levels considering deficiency should be treated with 4,000 to 6,000 IU/day for a 6- to 8-week period to restore levels to sufficient values. According to AACE and ACE guidelines, it is recommended that supplementation maintain levels above 30 ng/ml.13 The Endocrine Society in the United States recommends achieving a concentration of more than 30 ng/ml (> 75 nmol/L) of serum 25-OH,considering the optimal range is 40 to 60 ng/ml (100 to 150 nmol/L). The Endocrine Society also advocates an intake of 1,500 to 2,000 IU/day (37.5 to 50 μg) in adults, and that obese patients (BMI > 30 kg/m2) should take 3 times more than the normal adult daily vitamin dose.13 Unfortunately, epidemiological studies across the United States have routinely shown that deficiencies of vitamin D are typically found in approximately 70% of the population, and this deficiency is only expected to increase as the population works more indoors. The following research articles focus on the link between these deficiencies and the associated risk for early dental implant failure.
 |
| Figure 2. DentaMedica’s 6-week recovery program aimed at optimizing vitamin D and antioxidant levels prior to implant placement. |
Related Dental Complications Associated With Vitamin D Deficiency
Vitamin D plays an important role in supporting the immune system and the integration of various biomaterials. It is also relevant for decreasing general oxidative stress and minimizing additional inflammation caused by surgery. As expressed previously, vitamin D is also involved in biomaterial integration and other metabolic processes, such as bone remodeling. Therefore, some complications have been related to vitamin D deficiency in the dental field.
In 2009, a first animal study investigated the role of vitamin D in dental implant osseointegration.9 Utilizing a rat model, implants were placed in both normal control and vitamin D-deficient animals and subjected to implant push-out tests, as well as histological analysis. The push-out tests revealed an approximate 66% decrease in value in the vitamin D-deficient group and also revealed significantly lower bone-to-implant contact as early as 14 days post-implant placement. It was concluded from this study that the effect of vitamin D deficiency was unexpectedly profound. It was further addressed that future clinical research would benefit patient care, owing to these observations.
 |
Following years of initial preclinical studies demonstrating the marked impact of vitamin D deficiency on osseointegration, clinical studies were then reported. These began initially as case reports. In 2014, Bryce and MacBeth4 reported that vitamin D deficiency was suspected as a causative factor in the failure of immediate implants. In summary, it was reported that vitamin D deficiency was directly associated with early implant failure. It was also advised that the assessment of vitamin D prior to implant surgery be analyzed, especially in patients having undergone either long-term hospital care or a recent traumatic injury/event.4 Additionally, in the same year, it was also noted that low vitamin D deficiency may be a risk factor for implant osseointegration and also bone graft infection.5
In 2016, Fretwurst et al6 reported that unexpected implant removal in a dental university clinic was subject to much controversy around potential causes. These random implants were often removed after only 15 days following placement and, therefore, patients were then sent for various blood analyses. It was found in each case that extremely low serum vitamin D levels (serum vitamin D levels < 20 μg/L) were reported. This study group described that after a 6-month period of healing and vitamin D supplementation, levels were raised (> 46 μg/L), and implants were successfully osseointegrated in all cases following adequate supplementation.6
In 2017, Insua et al8 wrote an extensive review article on the concept of peri-implant disease being driven by osteoimmunology, osteal macrophages, and their related breakdowns and maintenance. An entire section was dedicated to vitamin D and its correlation with lower bone-to-implant contact and potential complications and peri-implant bone loss over time. Furthermore, the immune system was also discussed during the homeostasis of peri-implant tissue/osseointegration.8
In 2019, Mangano et al7 published a retrospective study whereby nearly 2,000 implants were investigated in nearly 1,000 patients (Table 2). To date, this represents the largest study on the topic where implant failure rates were gathered along with data on other known complications, such as smoking and generalized periodontitis. In this study, it was reported that heavy smoking (defined as 15 cigarettes per day) was found to be associated with an approximately 50% increase in early implant failures. Similarly, generalized periodontitis was also associated with an approximate 50% increase in dental implant failures. Interestingly, severe vitamin D deficiency (defined as serum levels < 10 ng/mL) was reported with a nearly 300% increase in overall implant failure rates when compared to controls.7 The conclusions from this study highlight the need for adequate testing, prevention, and supplementation prior to dental implant placement and maintenance.7
 |
Testing Vitamin D Levels
Standard vitamin D tests are routinely performed by measuring serum vitamin D levels in whole blood serum. Naturally, this provides an adequate analysis of blood vitamin D levels; however, the issue is the inconvenience to the patient seeking routine dental work. NanoSpeed Technologies has since developed a novel vitamin D test kit that is based on a simple finger-prick test (Figure 1). Within 10 minutes, vitamin D levels can be reported in-office. This easy-to-use test is cost effective and virtually painless when compared to competing technologies that require venous blood. The technology is based on the principle of a competitive immunoassay. Depending upon the concentration of vitamin D in blood/serum, there will be a varying number of free antibody-gold conjugate molecules that will bind to vitamin D on the test strip and will show a colored line in the test line zone.
During the specimen preparation, the blood sample (10 ul) are placed on the assay (red mark), according to Figure 1. Then 3 full drops of the kit’s “Chase” buffer is added into the square buffer well of the cassette. Within 10 minutes, the vitamin D measurement may be obtained.
Owing to this technological advancement, it becomes possible to utilize the equipment prior to dental implant placement or bone grafting surgery to determine levels/potential deficiencies prior to implant/graft surgery. When deficient, it is clear patients need a solution, and, typically, supplementation is recommended.
Supplemental Recovery Program: The Science Behind Dental Healing
Owing to the impact of vitamin D deficiency-related complications and failures in dentistry, clinicians are advised to use vitamin D supplements when deficiency is observed. Typically, 5,000 IU/day is recommended by the AACE; however, an 8- to 12-week supplementation period is needed to reach adequate levels. This timeframe makes implant dentistry quite inconvenient, owing to the often-encountered need to restore teeth at earlier timepoints, along with the necessity to satisfy patient expectations within reasonable timeframes. Over the years, it has become increasingly clear that vitamin D absorption is further optimized with several co-factors. These include vitamin K, magnesium, calcium, manganese, and boron, among others. These co-factors, when present, help absorb vitamin D toward optimal levels in shorter healing periods. Several supplementation recovery programs have been designed specifically for dentistry and implant/bone grafting procedures (DentaMedica) (Figure 2) with the aim of elevating levels prior to implant surgery within a 4-week period. Noteworthy research, however, has demonstrated that patients older than 65 years of age, diabetics, smokers, obese patients, and patients with reported compromised immune systems typically require double this timeframe of supplementation requirements.
The Role of Antioxidants in Wound Healing
In addition to bone-related deficiencies, several additional factors can impair wound healing, such as infection found in periodontal disease, poor diet, aging, diabetes, alcohol overuse, smoking, stress, and impaired nutritional status.14-16 In recent years, reactive oxygen species (ROS) have gained attention because of their central role to the progression of many inflammatory diseases.17 Excessive production of ROS or impaired ROS detoxification causes oxidative damage, which has been shown to be a main cause of non-healing chronic wounds and tissue degeneration.18,19
To combat oxidative stress, all cells in the body require an intrinsic store of molecules known as “antioxidants,” which prevent tissue damage.20 When this balance is shifted, however, high levels and activity of ROS cause DNA damage, protein damage, and lipid peroxidation. This leads to impairments in wound healing and many long-term chronic degenerative diseases and whole-body tissue inflammation, which are linked to common diseases such as dementia and various cancers.
 |
Unfortunately, a large percentage of the population today suffers from vitamin and mineral deficiencies directly linked to antioxidant levels (Table 3). As a result, it is clear that prior to any major surgery, vitamin recovery programs are indispensable to help restore the patient’s levels prior to surgery to prevent failure and/or delayed wound healing. Furthermore, restoring patient antioxidant levels remains a relatively easy and inexpensive task.
Vitamin C is, perhaps, one of the most well-known antioxidants and has a primary function as a radical scavenger and in the synthesis of collagen hydroxylation in humans.21 It also contributes to immune defense by supporting various cellular functions of both the innate and adaptive immune systems. Vitamin C deficiency results in impaired immunity and higher susceptibility to infections.22 Vitamin C is found in many natural fruits and vegetables, yet the population remains relatively deficient, owing to the poor nutritional status encountered in many patients.
Other important vitamins include flavonoids: polyphenolic compounds found in plants known to contain potent antioxidants, as well as anti-inflammatory, anti-allergic, and antitumor properties.23 Additionally, the vitamin B complex,24 carotenoids (vitamin A), magnesium,25,26 zinc,27 manganese, and selenium are but a few important minerals and vitamins that aid in wound healing. Needless to say, with the population being increasingly more deficient in key vitamins/minerals, their particular relationship with potential implant complications/failure remains to be investigated. To date, only a strong link between vitamin D deficiency and early implant failure has been reported, but it remains to be seen if other relationships exist.
CASE REPORT
Example of Early Implant Failure as a Suspected Result of Vitamin D Deficiency
Routinely, dental implants are placed with long-term success rates of 90% to 95%.28-31 However, for relatively unknown reasons, a small percentage of implants are lost each year with unexplained findings. Figure 3 demonstrates an initial ridge in a 73-year-old male patient with sufficient bone ridge width for implant placement. The patient was not on any medication and was considered healthy. Following midcrestal full-thickness flap elevation, a bone reduction alveoplasty procedure was done to allow adequate width for implant placement with 1.0 to 2.0 mm of remaining width on the buccal and lingual aspects (Figure 4). Note the excellent ridge width. Figure 5 demonstrates the implant osteotomies with adequate bone width on either side. Following implant placement at torque values of 40 Ncm (Figure 6), soft-tissue closure was obtained, and the patient was advised to maintain good-hygiene home care that included saltwater rinses following meals (Figure 7). A periapical radiograph was taken following implant placement, demonstrating adequate bone levels (Figure 8).
At the 2-week recall, suture removal was performed, and the patient was advised to be seen 1 month later. At 1-month postoperative, a subsequent periapical radiograph was taken in which severe bone loss was noted around the implant and clinical mobility was observed (Figure 9). The implants were therefore removed, and the patient was sent for medical analysis. This highlights a typical case whereby simple osseointegration was expected in a relatively straightforward case, and yet unexplained early implant failure occurred.
Upon testing of a full blood workup, the main finding was the patient’s low vitamin D levels. The patient reported levels of vitamin D deficiency. The patient was then supplemented with a 12-week recovery program of supplements (DentaMedica), and implant placement was successful thereafter. This case represents a standard recovery program and timeline following early implant failure for unknown reasons to promote local healing and recovery of vitamin and mineral levels. Vitamin D testing post-early implant failure almost always results in cases reported to be vitamin D-deficient.
Patient Testing and Supplementation
Owing to recent evidence suggesting a strong correlation between vitamin D deficiency and early implant failure, vitamin D testing before bone grafting and implant placement has therefore been recommended. While blood work is not always common and/or available within a dental office, the ability to adequately test vitamin D levels within 10 minutes with a simple finger-prick test becomes a highly valuable tool within dental offices (Figure 1). Upon discovery of low patient vitamin D levels, it becomes essential to supplement patients adequately prior to implant placement or bone grafting procedures. Another alternative is the use of supplementation prior to implant surgery and bone graft surgery. A minimum 4-week supplementation program is recommended to elevate all vitamin and mineral levels prior to surgery, followed by an additional 2 weeks post-op.
CLOSING COMMENTS
This article highlights the effects of vitamin D deficiency on early implant failure and bone graft complications. Vitamin D remains one of the most highly prevalent vitamin deficiencies known to man, and a direct link with bone tissue homeostasis and remodeling has been reported in the literature. It’s noteworthy that vitamin D is also linked with the immune system, whereby introduced biomaterials in the body (especially in bone) such as dental implants may be compromised when vitamin D deficiency is observed. Recent studies have demonstrated a marked and significant additional increase in early dental implant failure of roughly 300% higher in implants placed in vitamin D-deficient patients than in healthy patients. Furthermore, supplementation and a recovery program are discussed as a means to assist patients both pre-surgically as well as in the recovery phase.
References
1. Woo YS, Kim S, Jeong JH, et al. Vitamin D deficiency/insufficiency among inpatients with depressive symptoms. Clin Psychopharmacol Neurosci. 2019;17:121-124.
2. Wimalawansa SJ, Razzaque MS, Al-Daghri NM. Calcium and vitamin D in human health: Hype or real? J Steroid Biochem Mol Biol. 2018;180:4-14.
3. Akhavan A, Noroozi Z, Shafiei AA, et al. The effect of vitamin D supplementation on bone formation around titanium implants in diabetic rats. Dent Res J (Isfahan). 2012;9:582-587.
4. Bryce G, MacBeth N. Vitamin D deficiency as a suspected causative factor in the failure of an immediately placed dental implant: a case report. J R Nav Med Serv. 2014;100:328-332.
5. Choukroun J, Khoury G, Khoury F, et al. Two neglected biologic risk factors in bone grafting and implantology: high low-density lipoprotein cholesterol and low serum vitamin D. J Oral Implantol. 2014;40:110-114.
6. Fretwurst T, Grunert S, Woelber JP, et al. Vitamin D deficiency in early implant failure: two case reports. Int J Implant Dent. 2016;2:24.
7. Mangano FG, Ghertasi Oskouei S, Paz A, et al. Low serum vitamin D and early dental implant failure: Is there a connection? A retrospective clinical study on 1,740 implants placed in 885 patients. J Dent Res Dent Clin Dent Prospects. 2018;12:174-182.
8. Insua A, Monje A, Wang HL, et al. Basis of bone metabolism around dental implants during osseointegration and peri-implant bone loss. J Biomed Mater Res A. 2017;105:2075-2089.
9. Kelly J, Lin A, Wang CJ, et al. Vitamin D and bone physiology: demonstration of vitamin D deficiency in an implant osseointegration rat model. J Prosthodont. 2009;18:473-478.
10. Liu W, Zhang S, Zhao D, et al. Vitamin D supplementation enhances the fixation of titanium implants in chronic kidney disease mice. PLoS One. 2014;9:e95689.
11. Mangano F, Mortellaro C, Mangano N, et al. Is low serum vitamin D associated with early dental implant failure? A retrospective evaluation on 1,625 implants placed in 822 patients. Mediators Inflamm. 2016;2016:5319718.
12. Xiong Y, Zhang Y, Guo Y, et al. 1α,25-dihydroxyvitamin D3 increases implant osseointegration in diabetic mice partly through FoxO1 inactivation in osteoblasts. Biochem Biophys Res Commun. 2017;494:626-633.
13. Pludowski P, Holick MF, Grant WB, et al. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125-135.
14. Park JB, Han K, Park YG, et al. Association between alcohol consumption and periodontal disease: the 2008 to 2010 Korea National Health and Nutrition Examination Survey. J Periodontol. 2014;85:1521-1528.
15. Jang AY, Lee JK, Shin JY, et al. Association between smoking and periodontal disease in Korean adults: the fifth Korea National Health and Nutrition Examination Survey (2010 and 2012). Korean J Fam Med. 2016;37:117-122.
16. Ahn YB, Shin MS, Byun JS, et al. The association of hypertension with periodontitis is highlighted in female adults: results from the Fourth Korea National Health and Nutrition Examination Survey. J Clin Periodontol. 2015;42:998-1005.
17. Mittal M, Siddiqui MR, Tran K, et al. Reactive oxygen species in inflammation and tissue injury. Antioxid Redox Signal. 2014;20:1126-1167.
18. Cano Sanchez M, Lancel S, Boulanger E, et al. Targeting oxidative stress and mitochondrial dysfunction in the treatment of impaired wound healing: a systematic review. Antioxidants (Basel). 2018;7(8). pii: E98.
19. Wei W, Liu Q, Tan Y, et al. Oxidative stress, diabetes, and diabetic complications. Hemoglobin. 2009;33:370-377.
20. Sies H. Oxidative stress: oxidants and antioxidants. Exp Physiol. 1997;82:291-295.
21. Wilson JX. Regulation of vitamin C transport. Annu Rev Nutr. 2005;25:105-125.
22. Carr AC, Maggini S. Vitamin C and immune function. Nutrients. 2017;9(11). pii: E1211.
23. Vinson JA, Jang J. In vitro and in vivo lipoprotein antioxidant effect of a citrus extract and ascorbic acid on normal and hypercholesterolemic human subjects. J Med Food. 2001;4:187-192.
24. Polegato BF, Pereira AG, Azevedo PS, et al. Role of thiamin in health and disease. Nutr Clin Pract. 2019;34:558-564.
25. Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academies Press; 1997.
26. Coates PM, Betz JM, Blackman MR, et al, eds. Encyclopedia of Dietary Supplements. 2nd ed. Boca Raton, FL: CRC Press; 2010.
27. Lin PH, Sermersheim M, Li H, et al. Zinc in wound healing modulation. Nutrients. 2017;10(1). pii: E16.
28. Moraschini V, Poubel LA, Ferreira VF, et al. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44:377-388.
29. Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: a systematic review and meta-analysis. J Dent. 2015;43:487-498.
30. Del Fabbro M, Wallace SS, Testori T. Long-term implant survival in the grafted maxillary sinus: a systematic review. Int J Periodontics Restorative Dent. 2013;33:773-783.
31. Slagter KW, den Hartog L, Bakker NA, et al. Immediate placement of dental implants in the esthetic zone: a systematic review and pooled analysis. J Periodontol. 2014;85:e241-e250.
Dr. Miron is a visiting adjunct faculty member in the Department of Periodontology, University of Bern, Switzerland. He currently is the lead investigator in the Miron Lab (themironlab.com), located in Florida, which has received more than $1,000,000 in national and international funding to perform various research projects. His main research interests involve enamel matrix proteins for bone and periodontal regeneration, bioactive growth factors, platelet-rich fibrin, osteoinductive bone grafting materials, and guided bone regeneration in implant dentistry. He has written 2 best-selling textbooks widely distributed in regenerative dentistry, including his most recent in 2019, titled Next Generation Biomaterials for Bone and Periodontal Regeneration, and his 2017 textbook, titled Platelet Rich Fibrin in Regenerative Dentistry: From Biological Background to Clinical Indications. He can be reached at rick@themironlab.com.
Disclosure: Dr. Miron is a member of the DentaMedica advisory board and is involved in continuous research projects on the topics discussed herein.
Dr. Pikos graduated with honors from The Ohio State University (OSU) College of Dentistry and completed an internship at Miami Valley Hospital and residency training in oral and maxillofacial surgery at the University of Pittsburgh, Montefiore Hospital. He is a Diplomate of the American Board of Oral and Maxillofacial Surgery, the American Board of Oral Implantology/Implant Dentistry, and the International Congress of Oral Implantologists and a Fellow of the American College of Dentists. He is also an adjunct assistant professor in the Department of Oral and Maxillofacial Surgery at The OSU College of Dentistry and Nova Southeastern University College of Dental Medicine. He is also a courtesy clinical associate professor in the Department of Periodontology and Department of Prosthodontics at the University of Florida College of Dentistry. He is the founder and CEO of the Pikos Institute. Since 1990, he has been teaching advanced bone and soft-tissue grafting courses with alumni that now number more than 4,100 from all 50 states and 43 countries. Dr. Pikos maintains a private practice, which is limited exclusively to implant surgery, in Trinity, Fla (pikosinstitute.com). He can be reached at learn@pikosinstitute.com.
Disclosure: Dr. Pikos reports no disclosures.
Dr. Bishara completed his undergraduate studies in medical biophysics at the University of Western Ontario. He went on to complete his DDS degree at the Schulich School of Medicine and Dentistry. Since graduating, he practices in the Durham region with a focus on digital workflow, dental implants, bone grafting material regeneration, and tissue regeneration. He currently collaborates with members of the Miron Lab on tissue regeneration utilizing platelet-rich fibrin (PRF). He is a published author on PRF, immediate dental implants, and clinical applications. He is the president and founder of the Canadian Implant Dentistry Network (CIDN), Canada’s largest online implant community with over 11,000 members focused on advancing implant dentistry He can be reached at info@cdnimplants.com.
Disclosure: Dr. Bishara reports no disclosures.
Related Articles
Bone Grafting Materials in North America: Clinical Report of Biomaterial Usage
Basics of Platelet-Rich Fibrin Therapy
Patients Enrolled in Clinical Study of Bone Adhesive Material











