Increasing standards of aesthetics and higher incidences of allergies caused by titanium, coupled with greater demands for metal-free dental reconstructions, have resulted in the use of ceramics as a surrogate material in dental implants. Though titanium is still the material of choice in implant manufacturing, zirconia has become an attractive alternative material due to its enhanced aesthetic potential and higher mechanical strength compared to traditional metals.
Zirconia’s superior properties include its high compressive strength, higher tensile strength, and modulus of elasticity compared to any titanium alloy or commercial-grade pure titanium. Tetragonal zirconia polycrystal, specifically around 3-mol% yttrium oxide (yttria)-stabilized zirconia, is mainly the selected ceramic for dental implants. Zirconia’s white, opaque color with low affinity for bacterial plaque and ultra-biocompatibility make it a material of interest in the biomedical industry.1
Biomechanically Stable Processing
In its pure state, zirconium dioxide possesses low shear strength and is very brittle, which makes it unsuitable for dental applications. But adding small amounts of aluminum oxide and yttrium oxide increases zirconium’s modulus of elasticity and stabilizes it.
Today, hot isostatic pressing (HIP) subjects monocline zirconia to high pressure, which causes the condensation of particles and results in a tetragonal crystalline lattice structure, where the particles seem to overlap. This significant innovation prevents the propagation of cracks.
With HIP-processed zirconia, any microcrack that develops is quickly stabilized since the tetragonal particles expand into the monocline structure to fill the gap formed. This self-repairing characteristic is also known as the airbag effect.1,2
The modifications of polycrystal “HIP zirconia” material even prevent the material from aging. These key features eliminate breakage.3 Several experiments have evaluated the biomechanical properties of zirconium implants with significant success.4
The 2-Piece Prepable Design
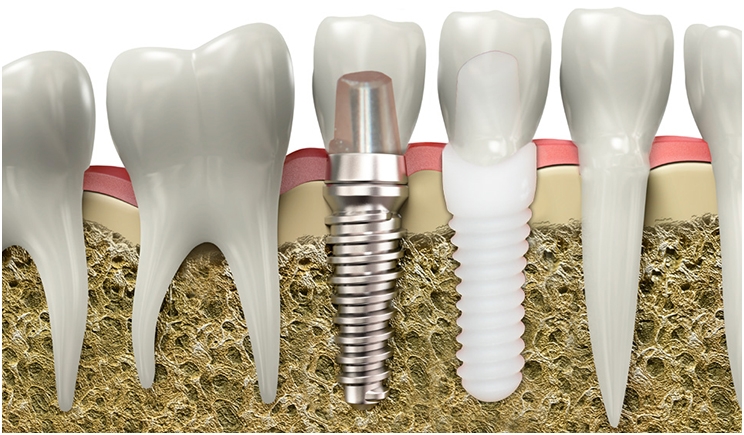
Previously, most zirconia implants were produced as one-piece implants. But these systems had some limitations. It was not always possible to satisfy prosthodontics requirements during the surgical placement, and the angled abutments for correcting misalignment were not available.
Secondary shape corrections with grinding always should be avoided since they could severely degrade zirconia’s fracture strength. Also, one-piece implants are exposed to forces from the tongue and mastication. Ensuring suitable torque, choosing a proper thread design, and using a guarded temporary appliance such as Essix can prevent these problems.
Many ceramic systems are offered as 2-piece implants that can be placed just like titanium implants with good primary stability and left to heal under the gums for 3 to 6 months. These implant systems also exhibit sufficient fracture resistance that can withstand strong bite forces.5
Also, to obtain high connection strength between the implant and abutment, a non-metal carbon reinforced screw made of high tech plastic (Iso-elastic properties) is needed to withstand tensile forces.
Two-piece implants with screw-retained abutments are preferable for many reasons. Further research will surely lead to improved biomechanical properties that will make it possible to try novel solutions. Enhanced strength also will enable the innovative design of implants, reconstructions, and the components for connecting them.5,6
Soft-Tissue Integration and Reduced Peri-Implantitis
From a biological perspective, zirconia provides very valuable characteristics. It has a very low affinity for bacterial plaque, a negligible inflammatory infiltrate, and remarkable soft-tissue integration. All of these characteristics can diminish the risk of peri-implant diseases.
It is suggested that the bacterial biofilm accumulates less on zirconia compared to titanium. Hence, it may be assumed that peri-implant soft tissues around zirconia implants will be at lower risk of infection and inflammation. Every implant material has a definite surface free energy. It is observed that zirconia abutments have low surface free energy and low surface wettability, reducing adhesion of bacteria.
Presently, with fair clinical experience, peri-implantitis appears to be less of a problem with zirconia implants than with titanium implnts. Actually, peri-implantitis has not been observed or reported so far, though this needs to be confirmed with longitudinal monitoring.4,7
References
- Özkurt Z, Kazazoğlu E. Zirconia dental implants: a literature review. J Oral Implantol. 2011;37:367-376.
- Shafie HR, ed. Clinical and Laboratory Manual of Dental Implant Abutments. Ames, IA: John Wiley & Sons; 2014.
- Monzavi M, Noumbissi S, Nowzari H. The impact of in vitro accelerated aging, approximating 30 and 60 years in vivo, on commercially available zirconia dental implants. Clin Implant Dent Relat Res. 2017;19:245-252.
- Cionca N, Hashim D, Mombelli A. Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000. 2017;73:241-258.
- Cionca N, Müller N, Mombelli A. Two‐piece zirconia implants supporting all‐ceramic crowns: a prospective clinical study. Clin Oral Implants Res. 2015;26:413-418.
- Aydın C, Yılmaz H, Bankoğlu M. A single-tooth, two-piece zirconia implant located in the anterior maxilla: a clinical report. J Prosthet Dent. 2013;109:70-74.
- Borgonovo AE, Censi R, Vavassori V, et al. Zirconia implants in esthetic areas: 4-year follow-up evaluation study. Int J Dent. 2015;2015:415029.
Dr. Gupta holds a master’s degree in oral and maxillofacial surgery and is trained in multiple allied surgical disciplines including implantology and laser dentistry. An academic writer, he has published papers in various national and international journals and magazines. He also has presented many national and international lectures on implantology and contributed a chapter on smile design with dental implants for JB Publishers in Poland. He additionally has been a freelance medical academic writer and research scientist since 2010. And, he has a wide clinical practice and is a global education and training manager at the International Academy of Ceramic Implantology (IAOCI). He can be reached at saurabh@iaoci.com.
Dr. Noumbissi obtained his DDS from Howard University and then attended the Loma Linda University Graduate Program in Implant Dentistry, receiving his Certificate in Implant Dentistry and a master of science degree in implant surgery. He has published abstracts, scientific research, and clinical reports in peer reviewed dental journals. His areas or research focus on bioceramics and their uses as regenerative, implant, and restorative material in dental implantology. He is the founder of the International Academy of Ceramic Implantology and practices metal-free implantology in Silver Spring, Md.
Related Articles
Laser Dentistry Requires Bright Practice Management
Online Video Illustrates Prettau Zirconia Bridge Treatment
Use a Laser to Replace a Fractured Solid Zirconia Crown











