
It’s clear that dentistry is not immune from challenges to traditional healthcare delivery and payment models that arise from outside influences. Changes in market demand and technological and environmental disruptors such as COVID-19 are forcing the industry to reimagine itself.
What’s less clear, to many, is the important role dentistry can play in the value equation both during and after the pandemic.
Even before the coronavirus began to spread in early 2020, oral health value-based care (VBC) was gaining significant traction in the United States. In fact, Medicaid dental claims related to VBC represented a third of all government reimbursements in 2017 after a steady increase over five years.
Government agencies, dental benefits companies, and commercial and private dentists are moving toward VBC. We’re seeing significant shifts in the industry, including the rise in automated subscription platforms, because of consumer habit changes, actual and perceived affordability of dental care, and the convergence of medical and dental benefit structures. The economic stress the COVID-19 pandemic has placed on the health system is, of course, a factor too.
Given those influences, respected organizations are moving to endorse VBC for oral health, the most recent being the National Association of Community Health Centers (NACHC). Shifting away from fragmented dental care into a coordinated, integrated care model, NACHC is well positioned to lead transformation into a value-based system.
But community health systems aren’t the only oral healthcare providers moving toward value. Ultimately, VBC constructs will become a mainstay for those working and operating in dentistry, so today’s practitioners should be considering how to find their place in the drive to value.
How are you handling these changes? Where’s your place in the shift toward VBC today? Where do you want to be in the future?
Prioritizing Holistic Health
The VBC model prioritizes preventive care and taking care of the whole patient. In dentistry, it’s been defined as the improvement of oral health outcomes divided by the cost to achieve those improvements. To us, this underscores the importance of integration and supporting oral healthcare quality as a key part of overall health care.
Taking a holistic view of patient health through interprofessional collaboration can pay off for the patient, the provider, and the payer. A recent study of integrated health system data found that for every 1% increase in access to dental services by diagnosed diabetics, there was a 0.2% decrease in the cost associated with uncontrolled diabetes, which carries a cost double to triple that of controlled diabetes.
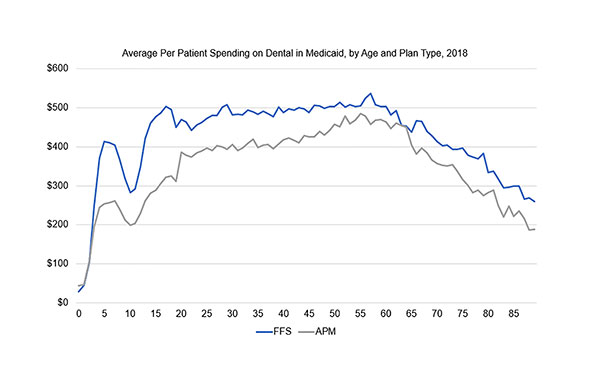 |
| Figure 2. Average per patient spending and utilization on dental care in Medicaid, by age and plan type, 2018. |
VBC opportunities focused on medical-dental integration present significant opportunities for dentists to contribute to overall health improvement and impact care costs for their patient populations, potentially sharing in the success of cost savings from medical care delivery.
A core characteristic of successful VBC is the utilization of minimally invasive care (MIC) that reverses or slows early disease stages. Using MIC to create remineralization or periodontal attachment gain is particularly valuable, notably at the population level, in improving systemic health and impacting cost.
Care teams and organizations driving value and cost savings have found great benefit with initiating and implementing MIC processes, and not just for safety measures detailed as part of the nation’s COVID-19 response.
These proactive processes promote patient wellness through management of chronic disease. In turn, this process drives enhanced outcomes beyond today’s approach of largely reactive interventions, reducing the need for more invasive and thus expensive procedures.
The Evolution of Value-Based Care
There are barriers and professional philosophies entangled with the evolution of VBC. Publications and editorials call attention to a lack of consensus on measurement, limited knowledge of VBC, concern with financial risk, and provider apprehension about patients’ willingness to improve their health.
Regardless of the challenges, many care teams and oral health organizations have found success with VBC models. Most likely, this is because VBC can enable resilience and adaptability for any dentist. For instance, the slower chair turnover and lower daily encounters from COVID-19 care interruptions have less of a financial impact when provider success relies on achieving goals, preventive care, and education delivered outside the dental chair.
One main characteristic shared by these successful programs is the understanding that today’s VBC designs are not the same as the capitated processes of health maintenance organization (HMO) programs, which did not result in widespread outcomes improvement or budget predictability for patient costs.
Today, VBC designs aim to help prepare for a future where patients are using services more but require less costly treatments to stay healthy. Figures 1 and 2 illustrate this using 2018 national Medicaid dental claims to compare alternative payment models (APMs) to fee-for-service (FFS) reimbursement. The analysis shows APMs cost less overall and have higher utilization than FFS.
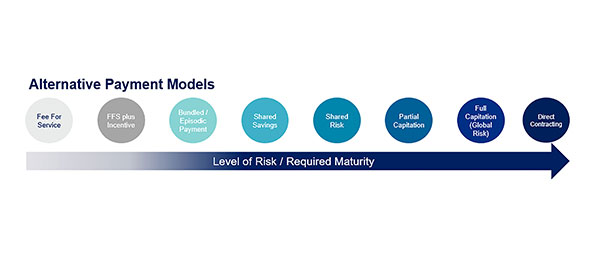 |
| Figure 3. Types of alternative payment models. |
Separating Value-Based Care and Value-Based Payment
A value-based approach to care can be enabled by reimbursement, but the concepts of VBC and value-based payment should not be considered synonymous.
Value-based payment in practice is typically classified as an APM, meaning that the structure is a variation of or completely different than traditional FFS reimbursement. How do these differ?
VBC reimbursement focuses on outcomes and the health of a population, and FFS relies on billing by procedure for financial sustainability. Said another way, traditional FFS structures generate service-based revenue, while VBC profitability comes from overall cost savings and more effective budgeting.
Value-based APMs generate that savings and predictability by tying reimbursement to a base payment for managing the health of a patient panel, plus variable payments based on provider quality performance and measurable improvement for oral health outcomes. This covers a continuum of payment models (Figure 3) scaled for the level of financial risk born by the provider.
More basic APMs (Figure 3, left side) such as FFS plus incentive or bundled payments still utilize the FFS structure but include reimbursement for achieving measures of quality through performance goals or meeting reporting expectations.
As the models mature, we get to shared risk and capitation or global risk payments, where the provider is accountable for quality of care as well as the cost of care for their patient population.
Direct contracting, at the far right of the continuum, offers the most potential for upside and downside risk given the provider can set the relationship with the purchaser (say, an employer) and bypass the payer or dental plan.
VBC structures that work align incentive payments with the care and outcomes desired. Incentives aimed at making an assigned population healthier incorporate compensation for reporting data, improving risk stratification, greater medical-dental integration, increasing prevention opportunities, and decreasing oral disease.
Incentive payments are most often based on specific population health benchmarks and encourage achievable maintenance and/or improvements year over year. Given the increased share of financial risk by providers and dental care organizations, VBC structures rely on transparency among all parties, usually in the form of data dashboards and/or provider scorecards, so care teams and payers can see performance in real time.
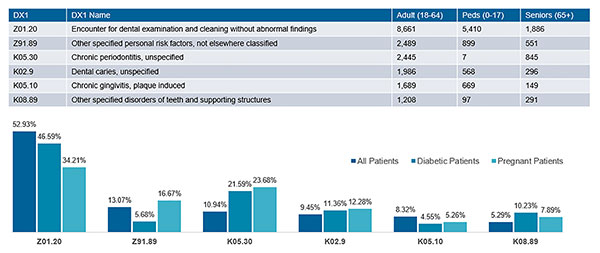 |
| Figure 4. Twelve-month utilization of ICD-10 diagnosis codes of an oral health value-based program. |
Where Any Dentist Can Focus Now
Care teams and dental businesses usually start tackling APM health maintenance or improvement incentives by risk stratifying their assigned patient population, which can be done in today’s environment since many plans already reimburse for caries risk assessment.
Considered most fitting for VBC, the American Academy of Family Physicians defines risk stratified management as the process of using the patient’s risk status to direct and improve care that prevents acceleration to higher risk categories and higher associated costs.
Within dentistry, there is no consensus on the best risk assessment tools or processes. Many care teams and organizations have developed their own methodology to best risk stratify their patient populations, and some organizations use analytics for a more user-friendly care flow process. To find your place, you can use free online training and other tools that outline specific steps and best practices to approach this type of care management.
Understanding an assigned patient population using risk stratified care management gives oral health providers better predictability in the cost of care for individual patients. Add in effective diagnosis coding, and providers can gain even greater insight to best invest in and implement care management and outreach.
These strategies together can be very important in more mature oral health VBC structures that may have financial incentives linked to shared savings from medical costs. Figure 4, for example, shows oral health-related diagnostic coding captured within electronic health records for an interprofessional quality improvement initiative.
Being able to identify a diabetic or pregnant adult with evidence of periodontitis, caries, or gingivitis enables participating dental and medical professionals to intercept and collaborate on disease management and, thus, lower the overall health cost.
As healthcare overall recovers and adjusts through the COVID-19 pandemic, the oral health industry should seize this opportunity. Now is the time to find your place in VBC and demonstrate the power of dentistry to improve population health and reduce overall health costs.
Dr. Boynes is a dentist anesthesiologist who received his DMD from the University of Pittsburgh and completed a three-year residency in anesthesiology from the University of Pittsburgh Medical Center. He currently serves as vice president, health improvement at the DentaQuest Partnership for Oral Health Advancement overseeing national programs and initiatives focused on the integration and coordination of person centered care, developing and implementing value-based oral health strategies and operations, and evaluating and testing change through meaningful oral health measurement and analytics. A prolific author and speaker, he has been recognized by many organizations for his work in health policy and clinical care.
Ms. Mathews is the director of value-based care for the DentaQuest Partnership for Oral Health Advancement, where she has a national leadership role in the implementation, development, and promotion of oral health VBC initiatives. Her responsibilities include developing and implementing care improvement collaboratives with state-level partners to produce effective care model change that aligns with the mission and vision of the DentaQuest Partnership, as well as supporting an innovative team aimed at readying a care model for VBC by transforming care with external stakeholders and provider teams in the Partnership’s learning collaboratives, identifying evidence-based best practices, and convening stakeholders for open discussion on VBC implementation. She is a graduate of the University of South Carolina with a bachelor’s degree in art history and a master’s in public administration.
Related Articles
Harvard Reaches $1 Million Scholarship Goal
Teledentistry for a Prosperous Future
Dental Providers Embrace Electronic Payment Capabilities











