INTRODUCTION
As digital impression scanning, computer-assisted design (CAD), and computer-assisted milling (CAM) are becoming more commonplace in dentistry, the use of high-strength ceramics, such as lithium disilicate and zirconia, are quickly becoming the main laboratory-fabricated restorative choices for many dentists. Lithium disilicate can be a very aesthetic material for both anterior and posterior full- and partial-coverage restorations, as it also exhibits higher strength and fracture toughness over conventional feldspathic and leucite-reinforced ceramics.
High-translucency (HT) ingots have improved the aesthetic quality but cannot always mask the color of a dark preparation. Zirconium oxide restorative materials got their start as tooth-colored replacements for traditional full-gold crowns on posterior teeth. Conservative posterior tooth preparations, similar to prep designs for gold, could be done because of the high strength of the material. However, early zirconia materials were very opaque and only indicated for first or second molars. Because zirconia is a metallic oxide (zirconium oxide), it can be used like a PFM crown to cover dark tooth preparations, and it can also be cemented with a conventional (nonadhesive) cement. Lithium disilicate and zirconia blocks can be designed and milled by the lab team to full contour, making them less labor intensive and less costly to the doctor. Since there are certain clinical indications where zirconia might be a desirable choice for use in the aesthetic zone, the challenge has been to provide the necessary aesthetic characteristics that are required for anterior restorations.
The following case report looks at an anterior case replacing previously placed feldspathic full-coverage restorations, while comparing lithium disilicate to a new aesthetic zirconia material (ArgenZ Anterior [Argen]).
CASE REPORT
A patient presented with a cohesive porcelain fracture on the facial surface of her right central incisor (tooth No. 8) that had been temporarily repaired with composite resin (Figure 1). Since it would be very difficult to match the old feldspathic material, it was decided to replace both the right (No. 8) and left (No. 9) central incisors with new all-ceramic restorations. The fracture in No. 8 was a longitudinal cohesive fracture in the facial ceramic (from the incisal edge to mid-tooth), so a high-strength material was considered for the replacement. In many dental practices, milled ceramic restorations, whether made by the lab team or at the chair, are becoming more commonplace because of reduced costs. In order to compare the aesthetic qualities of lithium disilicate (IPS e.max [Ivoclar Vivadent]) versus the anterior zirconia (ArgenZ Anterior), 2 separate cases would be fabricated by the lab team.
 |
 |
| Figure 1. A preoperative view of feldspathic restorations on the right and left central incisors (teeth Nos. 8 and 9), prior to replacement for a facial fracture on No. 8. | Figure 2. The lithium disilicate restorations tried in on Nos. 8 and 9. |
 |
 |
| Figure 3. The anterior zirconia restorations, in place on Nos. 8 and 9. | Figure 4. An ArgenZ Anterior (Argen Corporation) restoration on tooth No. 8 and an IPS e.max (Ivoclar Vivadent) restoration on tooth No. 9. |
 |
 |
| Figure 5. An IPS e.max restoration on tooth No. 8 and an ArgenZ Anterior restoration on tooth No. 9. | Figure 6. Both ArgenZ Anterior restorations were tried in on teeth Nos. 8 and 9. |
 |
 |
| Figure 7. A digital photo in isolate shade mode (EyeSpecial II [Shofu Dental]) was used to communicate the shade and characterization to the dental technician. | Figure 8. A milled polymethyl methacrylate (PMMA) prototype restoration was made and tried in to evaluate tooth contours, reflective line angles, incisal length, and emergence profiles. |
 |
 |
| Figure 9. The facial contours and disto-facial line angle of the PMMA prototype were adjusted using an 8-fluted carbide composite finishing bur (Komet), making minor corrections as desired by the patient and doctor. | Figure 10. The patient approved the PMMA prototypes after adjustments, then it was sent to the lab team to be scanned for the milling of the definitive restorations. The patient wore the original provisional restoration in the interim. |
Material Comparison and Selection
Figure 2 shows the lithium disilicate replacement restorations for teeth Nos. 8 and 9 tried in. The aesthetic match of the IPS e.max crowns was very good, with no problem observed in the value of the restorations.
Figure 3 shows the anterior zirconia replacement restorations for teeth Nos. 8 and 9 tried in. The aesthetics of the ArgenZ monolithic restorations was excellent when compared to the lithium disilicate restorations, with no decrease in the aesthetic quality observed.
To further compare the 2 materials, they were then placed side by side on adjacent preparations. Figure 4 shows an ArgenZ Anterior restoration on tooth No. 8 and a lithium disilicate restoration (IPS e.max) on tooth No. 9. Figure 5 is showing the opposite with a lithium disilicate restoration (IPS e.max) on tooth No. 8 and an ArgenZ Anterior restoration on tooth No. 9. Looking at both possibilities clinically in the patient’s mouth, it was impossible to discern any visible differences. The 2 anterior zirconia crowns, tried in on both teeth Nos. 8 and 9, can be seen in Figure 6.
Although any of these completed pair of restorations would have been a satisfactory end result for many patients, this case provided some challenges that typically can occur in the aesthetic zone. One problem with monolithic restorative materials is that if any characterization (such as stain and glaze) is done to the milled restoration, any adjustment to make even the most minor changes in the facial contour will adversely affect the aesthetic outcome. While in posterior restorations this may not be an issue, it can be a major problem for anterior restorations, requiring extra laboratory steps.
After comparison of these 2 materials, and since the aesthetic quality and value of the zirconia restorations was excellent, it was decided that the final case would be made using the ArgenZ Anterior material.
Aesthetic Zirconia for Anterior Teeth
ArgenZ Anterior was designed to give the clinician an aesthetic alternative for anterior full-coverage restorations when aesthetics and flexural strength are primary concerns. According to the manufacturer, there are several advantages with this new material: ArgenZ Anterior achieves 25% more translucency over HT zirconia, including ArgenZ Esthetic. This increased translucency comes from its unique composition that contains cubic zirconia. The crystalline structure of the cubic zirconia refracts light differently, increasing translucency and closely mimicking the appearance of a tooth’s natural dentin. In addition, ArgenZ Anterior has a flexural strength of 765 MPa, whereas the industry average for super translucent zirconia is around 650 MPa.
Milled PMMA Prototype to Customize the Definitive Restoration
In this case, the patient failed to approve the contours of either pair of completed restorations, so an attempt was made to make minor alterations in facial contour and embrasure shape to please the patient. Since this alteration of the crowns ruined the surface aesthetics, it was sent back to the laboratory to have a polymethyl methacrylate (PMMA) provisional made to verify that the corrections made to the original restorations would be acceptable before milling a second set of restorations. In hindsight, had this step been done first, it may have prevented the need to remake the ceramic restorations.
Prior to sending back the restorations for the remake, the shade was verified using a digital camera (EyeSpecial II [Shofu Dental]) in isolate shade mode so that the true colors of the teeth could be better visualized by the dental technician (Figure 7).
The recontoured ceramic restorations were then sent back to the laboratory where they were digitally scanned and a PMMA provisional restoration milled. The importance of this step should now be very clear. The facial position of the crowns relative to the lateral incisors, surface texture (or lack thereof), incisal length, prominence of the facial proximal (reflective) line angles, angle and depth of the facial embrasures, and sharpness or roundness of the mesial and distal incisal angles, are but a few nuances that need to be verified visually by the patient with a very exact prototype restoration (Figure 8). Any further modifications of the PMMA, if needed, can be easily accomplished at the try-in appointment (Figure 9). In this case, the patient originally had a diastema between teeth Nos. 8 and 9, so any black triangles in the gingival embrasure area needed to be compensated for in the mesial contours of the restorations to avoid negative space.
Final acceptance of the restoration contours by the patient, as done in the PMMA provisional restoration, were then scanned by the lab team into a digital file. Once that step was accomplished, an exact replica was then milled using the selected zirconia block and delivered to the patient (Figure 10).
Delivery of the Completed Case
The milled restorations are shown in Figure 11 on the master model. A cutaway view of an ArgenZ Anterior crown shows how precise the fit was to the master model (Figure 12). Final contouring, polishing, and glazing were then accomplished by the dental technician to complete the restorations (Figure 13).
The completed ArgenZ Anterior case was tried in and approved by the patient. Having satisfied the aesthetic desires of the patient, the case was ready to be cemented in. One clinical advantage of zirconia is that it can be conventionally cemented using a chemically bonded bioceramic luting cement (such as Ceramir Crown and Bridge [Doxa]), or adhesively cemented using a resin cement. For this case, a resin cement was chosen because of the aesthetics at the facial margin, should the patient experience gingival recession in the future as happened with her older restorations.
When using resin cement (such as Maxcem Elite Chroma [Kerr]) (Figure 14), a zirconia primer (such as Z-PRIME Plus [BISCO Dental Products]) or a universal primer (such as Monobond Plus [Ivoclar Vivadent]) is recommended to enhance the bond of the resin cement to the surface of the zirconia.
A universal bonding agent primer and adhesive (OptiBond XTR [Kerr]) was applied to the preparations in consecutive steps, air-thinned to evaporate the solvent, then light-cured according to manufacturer’s specifications. The internal surfaces of the zirconia crowns were treated with 2 coats of Z-PRIME Plus, then air-dried (Figure 15). The resin cement (Maxcem Elite Chroma) was placed into the restorations, and they were seated to place (Figure 16). A unique feature about this cement is that there is a color change from pink to tooth color to indicate when the gel set phase is complete. This gives the clinician a precise indication when to begin the clean-up process, preventing cleanup that can often be initiated too early in the setting process, possibly compromising the bond strength of the cement to the tooth. When the color change was complete (approximately 2 minutes), the marginal excess was cleaned up (Figure 17), then the restorations were light-cured (Demi Ultra [Kerr]). Figures 18 to 20 show the completed ArgenZ Anterior restorations. (Note: Zirconia restorative materials often display a slightly higher value than natural teeth when photographed due to less light absorption from the flash.)
 |
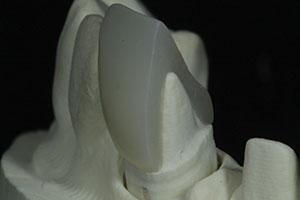 |
| Figure 11. A facial view of the milled ArgenZ Anterior restorations immediately after milling prior to the finishing and glazing by the dental technician. | Figure 12. This sectional view shows the intimate fit of the definitive restoration on the master die. |
 |
 |
| Figure 13. After some minor characterization and glazing, the completed restorations are shown on the master dies. | Figure 14. A zirconia primer (Z-PRIME Plus [BISCO Dental Products]) and resin cement (Maxcem Elite Chroma [Kerr]) were used in this case. |
 |
 |
| Figure 15. The zirconia primer (Z-PRIME Plus) was applied to the internal surface of the restorations prior to cementation. | Figure 16. The restorations, shown after filling with the self-etching resin cement and placement on the teeth. Note the pink color of the cement indicating that the gel set has yet to be reached; cleanup should not be initiated at this time. |
 |
 |
| Figure 17. Once the resin cement reached a gel set and turned to a tooth color, it was safe to remove marginal excess and floss the contacts without compromising the bond strength of the cement to the tooth or restoration. | Figure 18. Close-up retracted view immediately after cementation of the completed the ArgenZ Anterior restorations on teeth Nos. 8 and 9. |
 |
 |
| Figure 19. A smile view of the definitive restorations after cementation. (Note: The patient plans on replacing the maxillary lateral incisors and possibly the canines and premolars at a later time.) | Figure 20. A postoperative view (at one month) of the patient’s smile. |
DISCUSSION
This case was particularly challenging, since previously placed monochromatic feldspathic veneers with gingival recession and root exposure were present on the rest of the teeth. This is an example of real world dentistry! The patient could not afford to replace all the restorations at once; however, she did not want to necessarily match the color and root characterization of the remaining teeth. The challenge for both the dentist and the ceramist was to meet the expectations of the patient, whose desire was to eventually replace the old restorations with slightly higher value restorations to cover the exposed root surfaces and to fill the negative spaces of the gingival embrasures. The high lip-line also contributed to a compromised aesthetic result during this transition time for the patient. Future treatment will include the replacement of the remaining restorations in the aesthetic zone to better match these new central incisors when the patient is ready.
Technical Perspectives
Here are some recommendations to help the clinician maximize the aesthetic result when using anterior zirconia restorations. Although this material is used in the posterior areas much like metal, as far as tooth reduction is concerned for aesthetic areas, it is best to reduce the tooth as one would for a pressed ceramic restoration. This added reduction will give better depth and translucency to the material, also enabling an increase in value when a restoration is being placed over darker tooth structure, to create a more pleasing aesthetic result.
Take digital photos prior to preparation to avoid an increase in value due to tooth desiccation and to capture subtle tooth characterizations, incisal translucency, and surface texture of the tooth to be matched. After shade selection that is first based upon value, then hue and chroma, photograph several shade guides close to the target shade next to adjacent teeth. This will allow the ceramist to more accurately determine the desired shade of the restoration.
As previously stated, it is important to use an indirect digital PMMA provisional restoration for aesthetic acceptance from the patient prior milling the zirconia restorations so that the contours will not need adjustment at the delivery appointment. Finished zirconia restorations that are glazed and/or polished should not be subject to facial postoperative changes chairside by the dentist.
For postoperative care, use a nonabrasive, small-particle size prophy paste that is proven to kind to ceramic surfaces (such as Proxyt Fine [Ivoclar Vivadent]) for all hygiene appointments. This will provide longevity to the surface of the definitive restorations, particularly ones that are glazed.
CLOSING COMMENTS
In the author’s opinion, the results seen in this clinical case report demonstrate that the new zirconia material (ArgenZ Anterior) is a viable aesthetic and high-strength option for anterior full-coverage restorations, when indicated.
Acknowledgment
The author would like to acknowledge the technical excellence of Mr. Vincent Devaud, CFC, MDT, Digital Smile Design Instructor and Consulting Services, Beverly Hills, Calif, for the restorations created and shown here.
Dr. Lowe received his DDS magna cum laude from Loyola University School of Dentistry (1982). Following graduation, he completed a general practice residency program at Edward Hines Veteran’s Administration Hospital. After completion of dental school, he taught restorative and rehabilitative dentistry on a part-time basis and an additional 5 years on a full-time basis at Loyola University School of Dentistry as well as building a private practice in Chicago, where he currently practices part time in addition to his full-time practice in Charlotte, NC. He is a member of Catapult Elite Speakers’ Bureau and has Fellowships in the AGD, International and American Colleges of Dentists, Academy of Dentistry International, Pierre Fauchard Academy, the International Academy of Dento-Facial Aesthetics, and the American Society for Dental Aesthetics. In 2004, he received the Gordon Christensen Outstanding Lecturer Award for his contributions in the area of dental education. In 2005, he was nominated to receive Diplomate status on the American Board of Aesthetic Dentistry, an honor shared by fewer than 50 dentists in the entire United States. Throughout his career, he has authored and published several hundred articles in many phases of cosmetic and rehabilitative dentistry. He can be reached at (704) 450-3321 or at boblowedds@aol.com.
Disclosure: Dr. Lowe reports no disclosures.
Also By Dr. Lowe
A One-Visit Option: An Alternative to Traditional Ceramic Restorations
Putting Material Science to Work: Use of a Self-Polishing, Universal Nanohybrid Composite
A New and Economical Concept for No-Prep Veneers











