Social acceptance and success have a direct correlation to perceived attractiveness.1 Despite the growing demand for and popularity of facial rejuvenation procedures, traditional techniques have not changed much during the past few decades.2,3 With the increase in noninvasive cosmetic procedures, the patients presenting for such treatments are becoming more diverse in needs and presentation. This article discusses grouping and subgrouping to better assess and treatment plan cases in order to provide optimal cosmetic results and patient satisfaction.
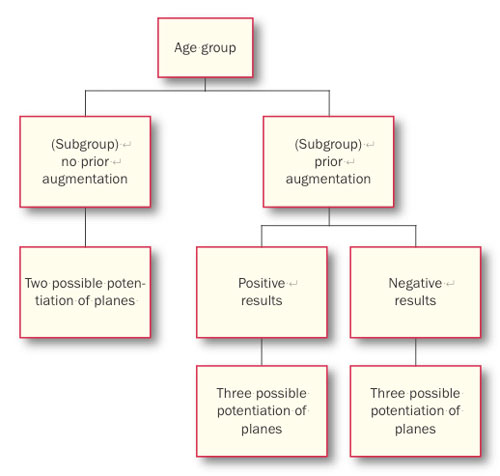
Patients can be sorted into 4 age groups when presenting for lip and perioral augmentation. These age groups are divided up into decades of aging and the oral facial signs of aging among these decades. The ages are 20 to 30 years, 30 to 40 years, 40 to 50 years, and 50 years and older. Within the 4 general age groups that present for lip and perioral oral augmentation are 3 potential subgroups. Further understanding these 3 subgroup classifications and their treatment possibilities are vital for successful augmentation. The 3 subgroups consist of patients with no previous lip augmentations, patients with prior lip augmentations with positive results, and patients with prior lip augmentations with negative results. This article also defines, describes, and communicates the potentials of each of these subgroups.
SIGNS OF FACIAL AGING
| Table 1. Effects of Facial Aging |
|
Lip and Perioral Effects of Aging:
|
The young face is characterized by an even distribution of ample fat and collagen that produces a “gently rolling plain” with more points of highlight than shadow. These points are complemented by a series of convexities and arcs. Aging produces dynamic and multifactorial facial changes (Table 1). Thus, the examination begins with looking for changes in appearance in the upper, mid, and lower face. Skin sags as muscle tone decreases, particularly in the chin and neck. The skin appears thinner and more translucent due to fat loss, the loss of elasticity and collagen, and it becomes drier and more wrinkled. Sun-damaged skin is more susceptible to these changes and appears to age faster than skin that has been protected by sunblock and/or the shade from a hat.3
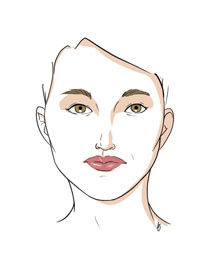
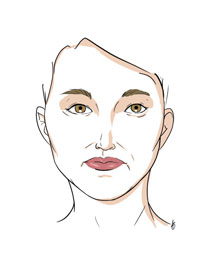
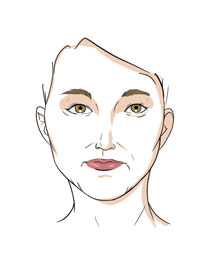
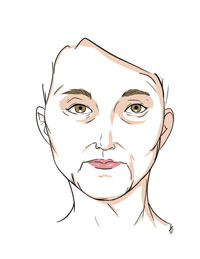
GROUPING BY AGE
The majority of times, the goal of lip and perioral augmentation is to reverse the signs of aging. These signs include loss of volume, definition, and flaccidity of tissue. These are direct visual aesthetic results of gravity, soft-tissue maturation, skeletal remodeling, and muscular facial activity.4 The lips reach their maturity in late adolescence. Women arrive at maxillary lip maturity at 14 years of age and mandibular lip maturity at 16 years of age. Men reach maxillary and mandibular lip maturity around 18 years of age.5-7 Yet throughout the decades of our lives, there are substantial changes per age group and the oral/facial skeletal dimensions continue to grow (Figures 1 to 4).8,9
|
From the late teens to the third decade of life, there is an average increase in the vertical dimension of our face from nasion to menton of 2.7 mm.10 Other studies tend to support the idea of anterior facial growth well into the fourth decade of life.1,11
Understanding these oral facial changes better prepares the practitioner to treatment plan aesthetic lip and perioral augmentation.
Beginning in the mid- to late 30s, changes become apparent throughout the face. Wrinkles and fine lines appear around the eyes and mouth. The dermal thickness is still relatively intact as in the earlier years of life, although gravity has weighed the face down. The telltale signs of aging occur in the upper face first.4,12 It is commonly believed that the weakest link in the chain of events to cause aging or drooping of the facial skin is the cohesive ability of the dermis and remodeling of fat distribution around the face.13 The lips still have significant tonicity to them and any request for augmentation will usually be for cosmetic volume increase, rather than any substantial sculpting.
In our 40s to 50s, the dermis tends to thin out due to hormonal changes and the loss of estrogen, which is particularly apparent in women. We see a decrease in the production of dermal collagen and a subsequent reduction in dermal thickness.14 We see labial rhytides develop around this time. The constant constriction of the orbicularis forms “sunbeam-like” wrinkles around the mouth. We also may start to develop “marionette lines” or a “Chinese mustache” at the angles of the mouth descending down to the inferior border of the mandible. This is the onset of ptosis that is commonly associated with the skin.15
As faces mature through the ages of the 50s and 60s, the jaw line sags and the corners of the mouth droop down. The lack of tonus from the musculature and the pull of gravity draw the overall expression of the mouth down. The intercommissural distance increases with age, whereas lip height decreases. As we mature, photographs will reveal that the lower incisors have become more prevalent when we talk. In photographs of younger people, on the other hand, the lip-line is higher during conversation and the incisal edge of the maxillary teeth is present.16
Defining and grouping patients by decades reveal several trends. Volume is lost in the lip and perioral area as we mature, and definition of lip anatomy diminishes as well.
| Table 2. Augmentation Need Related to Age | |||||||||||||||||||||||||
|
This becomes important particularly when treatment planning how much material needs to be used to acquire the desired outcome. For example, a patient in her 30s may only require one syringe of filler material to augment her oral facial area. A patient in her 50s may very well require 2 to 3 syringes, which can become rather expensive at 6- to 8-month intervals for reaugmentation. The latter patient may fare better with a conventional facelift and then sequential filler therapy, which would require less syringes and less cost to the patient (Table 2).
SUBGROUPS WITHIN THE AGE GROUPS
Understanding the various patient-presenting groups is vital in lip and perioral augmentation. This article generally divides the patients into 4 age groups. The 4 age groups present different augmentation needs to attain a successful, aesthetic result. Yet within these 4 age groups are 3 subgroups, which include: (1) patients with no previous lip augmentation treatments, (2) patients with prior lip augmentation with positive results, and (3) patients with prior lip augmentation with negative results.
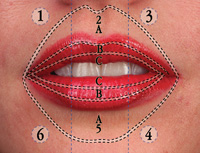
One must also understand the natural lip planes that exist in a lip (Table 3). There are 3 potential places fillers can go when we are injecting filling material into the lips for augmentation.
| Table 3. Natural Lip Planes |
 |
Natural Plane: This is the plane that naturally exists in the patient’s dermis. The junction of the dermal layer that the needle is placed in is right below the vermilion epithelium. This plane will relieve itself laterally to host the fillers as pressure is applied. The resistance to separation in this layer differs by skin type. The more keratinized the tissue, the more resistance, and vice versa. The lips have very little resistance in the dermal plane. The fill can be easily distorted by expressing too much pressure in the fill. The distortion comes from the material flowing into undesired zones of placement.
Acquired Plane: This plane has been established by a previous fill of a material that has occupied the space for a time. This plane may divert your filling material away from your planned augmented areas.
Path of Needle Insertion: This plane is created by the needle as it is injected into the dermis. If we apply very little pressure and withdraw the filler as we express the material, we will fill this space.
(Further in-depth description and planes augmentation can be found in the textbook, Vermilion Dollar Lips, by Dr. Robert Gordon.)
Patients With No Prior Lip Augmentation
Patients with no prior lip augmentation present physiologically with some distinct challenges. The tissue for implantation has had no previous fill, so the potentiated space is reliant more on the natural space or planes. When we are augmenting “virgin” lips with filler material, the filler has the propensity to glump or become bumpy in the lips. This is due to the tight tonicity of the vermilion tissue, and this pressure can lead to an uneven flow. This is particularly true of highly viscous materials such as cross-linked hyaluronic acid. An important point to remember is not to force more material into the lips at the time of occurrence. Instead there are several options available to remedy when an uneven flow of materials occurs:
- Wait until the one-week post-op to smooth out the filling material.
- Add additional filler material after one-week initial augmentation.
After waiting one week for reaugmentation, this allows the tissue that was previously taut to loosen up, via the natural pressure of the existing filler. We are also in a better situation to evaluate the fill without the natural swelling that comes from the trauma of filling a needle injection.
Patients With Prior Lip Augmentations: Positive Aesthetic Results
When we refer to a positive aesthetic result, we are categorizing the patient by effect resulting from:
- Lip augmentation fulfilling the patient’s cosmetic desires
- The augmentation presents with a natural pleasing appearance
- The prior lip augmentation has had no traumatic effect on patient’s lip and/or perioral tissue that may encumber sequential augmentations.
This subgroup of patients is the most “user friendly.” By this, I mean these patients have had previous experience in lip augmentation, which leads them to be more receptive to treatment modalities. They are usually less anxious during treatment and they are more patient in the postaugmentation phase. The planes in the lips of these patients have been filled, and there is a memory of plane saturation that responds well to a refill. That is why it is so important to fill your initial lip patients as well as possible and to abide by the natural planes of the lips. This focus will allow easier more pleasing sequential fills.
Patients With Prior Lip Augmentations: Negative Aesthetic Results
This is the most challenging of all subgroups. A bad lip augmentation will not only present unpleasantly; it has the potential to affect sequential fills on that patient, even when a resorbable material is used. An overzealous fill or improper lip plane placement will distend and relieve a space within the lips. When the augmenter readministers filler into the lips after resorption of a previously placed filler, the plane may still exist. The sequential augmentation will follow the path of least resistance and has the propensity to flow into the plane. The only solution when one encounters such a case is to slow down the injection process. Observe the flow carefully, and when the filling material deviates from the natural planes of the lips, STOP—Evaluate—and Relocate. Relocate the needle into an area of the lip that will allow the flow of the material to augment the natural plane. Logic dictates that one will have to inject in several more additional sites around the lips to facilitate the even distribution of the natural planes. My own clinical experience dictates that it only takes a couple of reaugmentations to resolve most bad augmentations.
Remember that when augmenting the lips, the material will want to fill the natural planes. The kinetic movements and static positions are conducive to the natural planes. Following these planes will allow for a more aesthetic, durable, and repeatable augmentation.
SUMMARY
This article has described the different age groups that present for noninvasive injectable lip and perioral augmentation, as well as the breakdown of 3 subgroups that present within the 4 general age groups. With the fundamental understanding of these presenting groups and subgroups, the practicing augmenter will be able to better treatment plan and educate the patient on realistic and optimal aesthetic outcomes.
References
- French M. Physical appearance and earnings: further evidence. Applied Economics. 2002;34:569-572.
- Hamra ST. Prevention and correction of the “face-lifted’’ appearance. Facial Plast Surg. 2000;16:215-229.
- Rendon MI. The aging face: initial assessment and consultation. Cosmetic Dermatology. 2006;19(suppl 2):6.
- Donofrio LM. Fat distribution: a morphologic study of the aging face. Dermatol Surg. 2000;26:1107-1112.
- Mamandras AH. Linear changes of the maxillary and mandibular lips. Am J Orthod Dentofacial Orthop. 1998;94:405-410.
- Genecov JS, Sinclair PM, Dechow PC. Development of the nose and soft tissue profile. Angle Orthod. 1990;60:191-198.
- Subtelny JD. A longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structures. Am J Orthod. 1959;45:481-507.
- Forsberg CM. Facial morphology and ageing: a longitudinal cephalometric investigation of young adults. Eur J Orthod. 1979;1:15-23.
- Forsberg CM, Eliasson S, Westergren H. Face height and tooth eruption in adults—a 20-year follow-up investigation. Eur J Orthod. 1991;13:249-254.
- Gormely JS, Richardson ME. Linear and angular changes in dento-facial dimensions in the third decade. Br J Orthod. 1999;26:51-55.
- Bishara SE, Treder JE, Jakobsen JR. Facial and dental changes in adulthood. Am J Orthod Dentofacial Orthop. 1994;106:175-186.
- Miller PJ, Wang TD, Cook TA. Rejuvenation of the aging forehead and brow. Facial Plast Surg. 1996;12:147-155.
- Bolognia JL. Aging skin. Am J Med. 1995;98:99S-103S.
- Spósito MM. New indications for botulinum toxin type A in cosmetics: mouth and neck. Plast Reconstr Surg. 2002;110:601-611.
- Lévêque JL, Goubanova E. Influence of age on the lips and perioral skin. Dermatology. 2004;208:307-313.
- Gordon RW. Vermilion Dollar Lips: Lip and Perioral Augmentation for the Cosmetic Dentist. Tampa, Fla: Vermilion Dollar Publications; 2008.
Dr. Gordon graduated from Marquette University School of Dentistry and continued his education in a residency program in periodontics as well as additional oral/surgery training. He practices in Miami and Tampa, Fla, and he lectures often, instructing oral/facial augmenters on his classification, diagnostic, and reconstructive lip and perioral augmentation techniques. He can be reached via e-mail at dr.g@vermiliondollarlips.com or visit the Web site vermiliondollarlips.com.
Disclosure: Dr. Gordon reports no conflicts of interest.