INTRODUCTION
During the past 10 years, immediate loading on a screw-retained prosthesis, also known as All-on-4 (Six), has enjoyed a meteoric increase in popularity in the surgical and prosthetic circles of the dental industry. Although the literature is flush with impressive 5-year follow-up documentation, there are some fundamental concerns for both clinicians and patients to consider. One of these concerns is managing the home care of the prosthesis. Most of these prostheses are designed to replace lost gingival architecture. This results in significant ridge lapping, thereby creating a cleansing challenge for the patient. The occurrence of mucositis (24% of “All-on-X” cases) and peri-implantitis (13.7% of “All-on-X” cases) secondary to inadequate hygiene has been documented.1 Soto-Penaloza et al2 reported that peri-implantitis was the second most common complication found in their systematic review. Many of the patients seeking the All-on-4 prosthetic solutions lost their teeth secondary to the most aggressive form of periodontitis. It is well-documented that patients with a history of periodontitis have an increased risk for peri-implantitis, which can result in implant failure.3
This article reviews a removable alternative that offers patients the security of a highly retentive and hygienic solution. The concept of telescopic (also known as “double crown”) retained prostheses is not new to dentistry. The use of retained roots to support an overdenture in periodontally compromised dentitions has a long history. Select teeth would receive intentional endodontic treatment, followed by telescopic retentive copings that engaged a “second crown” embedded in the prosthesis. There are a plethora of variations of this technique utilizing implants as opposed to retained roots.4-6 The Deutsch Removable Bridge is one example with which the author has had consistent success. It provides enhanced ease of hygiene maintenance. It is known for excellent retention, aesthetics, and function. An additional benefit is that significantly less bone reduction is necessary to accommodate the space requirements of this prosthesis.
CASE REPORT
A 71-year-old female presented for evaluation with a CC of multiple broken and decayed teeth and a desire for replacement. A complete exam yielded no contraindications to dental treatment (Figure 1). A range of treatment options was discussed, including conventional dentures, partial dentures, and an implant-retained prosthesis. Based on the patient’s goals, maxillary and mandibular implant-retained removable prostheses were treatment planned. The Deutsch Removable Bridge protocol was employed for both arches. Four months prior to the prosthetic phase, all maxillary teeth except Nos. 2 and 15 were removed, and 5 BioHorizons implants were placed in the maxillary arch (Figure 2). The 2 retained teeth had prior crown therapy, and it was decided to utilize them as additional supporting abutments. A clinical decision was made to retain teeth Nos. 22 to 26. At a second surgical visit, tooth No. 27 was removed, and 4 implants were placed: 2 each bilaterally (Figure 2). Following placement of the implants, 6 clinical visits precede prosthetic delivery.


Prosthetic Visit 1
After radiographic verification of completely seated impression copings, a traditional open tray (Miratray, cellophane is also acceptable) technique was employed (Figure 3).

Visit 2
At this visit, the lab returned a segmented verification jig and a custom tray for a pick-up final impression. The jig was then unified with a light-cured gel, such as LC (RH Supplies) (Figure 4).

Visits 3 and 4
The goal of these visits was to establish the patient’s proper vertical and centric record of occlusion. The lab provided a screw-retained bite rim. Additionally, full-face photographs were utilized to assist with midline, high smile line, and resting position. The fourth visit also included a screw-retained wax tooth try-in, which was critical to verify or alter aesthetics and phonetics as needed (Figures 5 and 6).
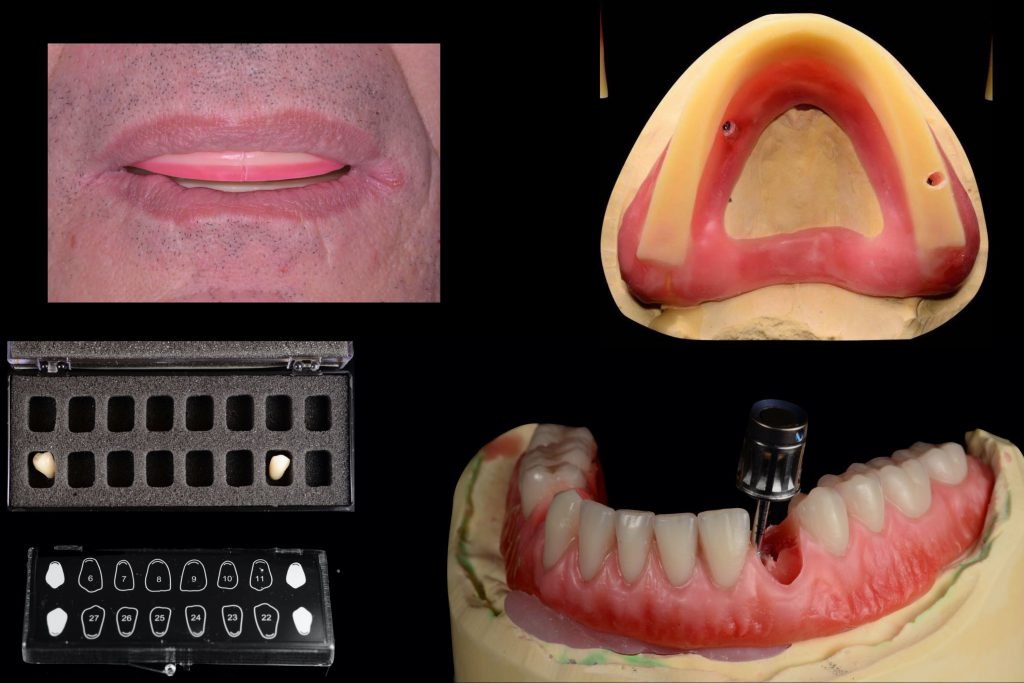

Visit 5
This is a critical step in the protocol. The lab provided the following:
- Abutments for the implants to be torqued at 30 Ncm.
- Gold anodized copings. These were numbered on the buccal by the lab and matched to specific implants.
- A tertiary structure to pick up the copings, which was adjusted as needed to seat completely and passively (Figure 7). Then a small amount (one-third of each receptacle) was filled with RelyX Unicem 2 (3M). This is a dual-cured cement that remained over the copings for 8 minutes and pulled out with the tertiary structure when it was removed.
- A temporary version of the final prosthesis to be worn for 4 to 6 weeks to work out any needed adjustments (Figure 8).


Final Delivery Visit
The final prosthesis was delivered, adjusted, and equilibrated (Figures 9 and 10). This visit is often quick, with little to no adjustments required, as the previous steps serve as a rock-solid path to success.


ACKNOWLEDGEMENT
The author would like to thank Arian Deutsch for his technical and didactic contributions to this article.
REFERENCES
1. Ülkü SZ, Kaya FA, Uysal E, et al. Clinical evaluation of complications in implant-supported dentures: a 4-year retrospective study. Med Sci Monit. 2017;23:6137-6143.
2. Soto-Penaloza D, Zaragozí-Alonso R, Penarrocha-Diago M, et al. The all-on-four treatment concept: systematic review. J Clin Exp Dent. 2017;9:e474-e488.
3. Courtney M, Cottrell D, Ayilavarapu S. Dental implant therapy in patients with a history of periodontitis: a literature review and clinical considerations. Compend Contin Educ Dent. 2012;33:e94-e97.
4. Yalisove IL, Dietz JB. Telescopic Prosthetic Therapy. George F. Stickley; 1977.
5. Fobbe H, Rammelsberg P, Bermejo JL, et al. The up-to-11-year survival and success of implants and abutment teeth under solely implant-supported and combined tooth-implant-supported double crown-retained removable dentures. Clin Oral Implants Res. 2019;30:1134-1141.
6. Seo JG, Cho JH. Clinical outcomes of rigid and non-rigid telescopic double-crown-retained removable dental prostheses: an analytical review. J Adv Prosthodont. 2020;12:38-48.
ABOUT THE AUTHOR
Dr. Rasner earned his DMD degree from the University of Pennsylvania. He has completed the Misch International Implant Institute curriculum and the Pikos Institute continuum. Dr. Rasner has been teaching for 20 years. His courses, “Atraumatic Extractions for the GP” and “The Bulletproof Guide to Implant Success,” have been popular at ADA and AGD component society meetings, as well as at the national ADA meeting. His newest course, “Hands-on Atraumatic Extractions for the GP,” features 2 days of live-patient experience in his office. He has authored 3 books and more than 50 industry and journal publications. He can be reached at drrasner@aol.com.
Disclosure: Dr. Rasner reports no disclosures.


