INTRODUCTION
The focus of modern restorative dentistry is both the preservation of residual tooth structure and the recreation of missing substrate layers in both aesthetic and functional realms. It is well-known that enamel varies significantly from dentin biomechanically and optically as both elements have key roles to play in everyday functional performance.
Enamel features an elastic modulus ranging from 73 to 77.9 GPa when measured along its prism length1 and extremely low fracture toughness, making it a brittle, glass-like structure. Dentin exhibits a significant interpenetrating collagen framework and acts as the hue source for the entire tooth, with chroma and value being modulated by the enamel thickness.
It is the interplay of interfaces of enamel and dentin that impart not only depth of aesthetic beauty but also a self-healing, fracture-tough behavior.
Modern indirect bondable ceramic substrates have flexural moduli that range from 66 GPa to 94 GPa and span options including feldspathic porcelain, leucite-reinforced glass-ceramic, and lithium disilicate. This level of flexural stiffness makes them well-suited to enamel replacements in biomimetic practice.
Dentin volumetric replacements are best matched with bonded composite resin as the elastic modulus of dentin is in the range of 16 to 20 GPa,2 which is well-matched to modern composites, and typically exhibits flexural moduli in the 10- to 20-GPa range.
The most common restorative procedure in modern dental practice is the replacement of posterior amalgam restorations. The goal of biomimetic dentistry is the replacement of nature in 4 spheres—biology, mechanics, function, and optics—with a non- or minimally invasive approach. The planning of these often extensive restorations is fraught with challenges. Ideally, a bondable, enamel-like material featuring a heightened elastic modulus and translucency is used to replace enamel.
A bondable, more fracture-tough material should be used for dentin and should be capable of both bonding to the more rigid enamel replacement and “fusing” with the existing residual dentin body at a shear bond strength representative of nature. This material should also have chromatic intensity and opacity imparted by dentin.
Modern adhesive protocols using gold standard adhesives have demonstrated microtensile bond strengths that closely replicate the bond strength between native enamel and dentin.
It is well-known that the cost of indirect restorations is often significantly greater than that of direct alternatives, posing a financial contraindication for many patients. There is significantly decreased coronal stiffness when the surface area of a bonded resin composite restoration exceeds 65% of the surface area of the tooth,3 and only bonded porcelain restorations are able to fully recover this lost coronal stiffness relative to a virgin control.
Despite these considerations, large, complex restorative defects are becoming increasingly treated with direct, superfilled composite resins due to improved material chemistry and optical and physical properties. This expanded function using modern “supercomposites” drives a pragmatic solution that simultaneously addresses the need for both cost efficiency and preservation of tooth structure.
Composite resin is a material that strives to mimic the missing enamel and dentin both functionally and optically. The compressive strength of enamel and dentin is rated at 384 MPa and 297 MPa, respectively. Comparatively, a modern composite such as GrandioSO (VOCO) features a compressive strength of 439 MPa, so it is a very suitable and strong replacement for both enamel and dentin. Flexural strength is only applicable to dentin as it has lower brittleness than enamel, which functions as a glass.
The flexural strength of GrandioSO is 187 MPa, and even after 5,000 thermocycles, it is rated at 158 MPa. These naturomimetic materials will strengthen residual structure due to the ability of adhesive bonding to adhesively bond to hydroxyapatite; however, their use is not limited to intracoronal applications.4 The material’s inherent stiffness and wear characteristics make it suitable for cusp-coverage expanded indications in the restoration of caries, post-endodontic cuspal coverage, or hypomineralization-compromised teeth.
CASE REPORT
A 12-year-old ASA 2 patient presented on referral from the pediatric dentist to manage bilateral maxillary bicuspid hypomineralization with secondary caries undermining all surfaces of the teeth as an extension of Amelogenesis Imperfecta Type II (hypocalcified variant). The teeth were reported to be hypersensitive.
Her medical history was unremarkable aside from status-post repair of an innocent heart murmur. She was under review by an orthodontist as she had bilateral posterior premolar crossbites, and these teeth were planned for retention. Clinically, enamel disintegration was noted with secondary caries noted on tooth nos. 4MOBL, 13MOBL, and 5MODBL; an overhang noted tooth No 12L with an isoform/amalgam MODBL crown with occlusal functional perforation; and a resulting distal marginal defect noted.
These findings were corroborated with the radiographic diagnosis of caries/hypoplastic enamel noted on these teeth with a distal marginal defect of the isoform crown on the distal aspect (Figure 1). All in all, exploratory restorations were required to remove caries as well as a proportion of the organic, matrix-rich, hypomineralized lesions to gain a more stable, mineralized base for predictable bonding.

Figure 1. Preoperative view of teeth Nos. 12 and 13 showing carious and restorative compromise of both teeth in this mid-mixed dentition hypomineralization case.
PROCEDURE
The patient was anesthetized using 3 carpules of 2% Lignocaine with 1:100,000 epinephrine (Septodont), and teeth Nos. 12 and 13 were isolated using a rubber dam before the removal of caries and hypomineralized structure (Figure 2).

Figure 2. Pre-op isolation with extensive cavitated hypomineralized lesions present on tooth No. 13 and a loose isoform perforated metal crown on tooth No. 12.
The resulting preparation was indeed similar to a traditional crown preparation as the caries and compromised enamel were ringbarked around the tooth, leaving virtually no viable enamel (Figure 3). Increased cervical access and hemostasis were gained using a super-pulsed, dual-wavelength diode laser (Gemini [Ultradent Products]) to refine the preparations after the rubber dam was removed.

Figure 3. Any superficial enamel was completely undermined by caries or hypomineralized regions. One can visualize some residual hypomineralized enamel cervicopalatally. A dual-wavelength super-pulsed diode laser (Gemini [Ultradent Products]) was utilized to trough/retract the edematous tissues and gain hemostasis simultaneously for the alginate impression.

Figure 4a. Alginate impression of the clinical situation before being poured up with Die silicone (VOCO).

Figure 4b. Die silicone model generated from the alginate impression.
A super-filled nanohybrid composite was sculpted in cured single-shade layers (A2, GrandioSO) to full anatomic form on the die silicone model, then removed, and contours were refined to ensure proper proximoaxial form and lack of overhangs.
The fissure system was characterized using a composite tint system (FinalTouch [VOCO]) before final extraoral finishing and polishing (Figure 5).

Figure 5a. Direct composite placement on the Die silicone model allows for patient comfort/respite and accessibility of contouring for lifelike results.

Figure 5b. Sectioned individual direct composite crowns, fully characterized and ready for try-in.

Figure 5c. Artistic lighting showing
The individual composite crowns were tried in after topping up anesthesia, and the contacts and marginal fit were verified. The intaglio surface of the composite crowns were treated using 33% orthophosphoric acid (Ultra-Etch [Ultradent Products]) before being treated with a silane coupling agent (G-Multi PRIMER [GC America]).
The preparations were micro-air abraded using 27-µm aluminum oxide before the placement of the retraction cord, and the teeth were etched using 33% orthophosphoric acid (Figure 6).

Figure 6. Retraction cords in place, and the adhesive bonding procedure initiated.
A 2% chlorhexidine solution was scrubbed into the dentin for 30 seconds to rewet the dentin and inhibit the activity of matrix metalloproteinases. After blot drying, a fifth-generation dentin adhesive was applied (OptiBond Solo Plus [Kerr Dental]) and air-thinned according to the manufacturer’s guidelines. The crowns were loaded with A2-shade Panavia SA Cement Universal (Kuraray America) and seated. The excess was removed, and contacts were cleared before flash curing the restorations.
An oxygen-inhibiting gel was placed pericervically before a final cure was imparted. The occlusion was adjusted to remove all lateral excursive interferences as composite is strong in compressive and weak in tension. Following final finishing and polishing, a postoperative bite-wing radiograph was taken, which confirmed the excellent marginal integrity and proximoaxial contours of the restorations (Figure 7).

Figure 7a. Occlusion-adjusted and post-finishing view of teeth Nos. 12 and 13.
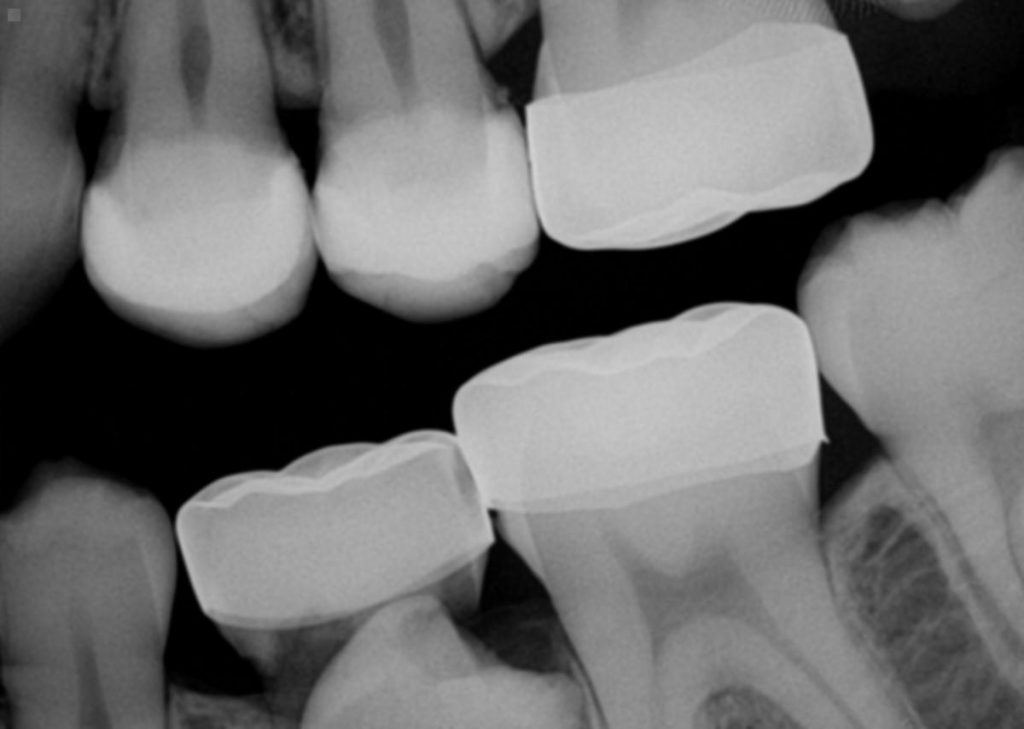
Figure 7b. Postoperative radiograph showing well-contoured and seated restorations with excellent marginal seal.
CONCLUSION
Modern composite resins exhibit exceptional physical and optical properties, allowing them to succeed and survive in clinical situations that would previously have been contraindicated. Bonded porcelain restorations are still the gold standard with large dose, large surface area replacement restorations; however, with controlled functional load, direct restorations can often equal that of their indirect counterparts.
An extreme example pertains to endodontically treated teeth. The ability of indirect resin composites to act as a viable alternative to overlay these compromised teeth over time shows that the ultimate determinant of prognosis is preservation of pericervical dentin.4
It is exciting that the benefits of residual structure preservation can now not only be the buzzword on everyone’s lips but can also be realized intraorally.
REFERENCES
1. Chrepa V, Konstantinidis I, Kotsakis GA, et al. The survival of indirect composite resin onlays for the restoration of root filled teeth: a retrospective medium-term study. Int Endod J. 2014;47(10):967-73. doi:10.1111/iej.12242
2. Magne P, Belser U. Bonded porcelain restorations in the anterior dentition: A biomimetic approach. Quintessence Publishing; 2002.
3. Spears IR. A three-dimensional finite element model of prismatic enamel: a re-appraisal of the data on the Young’s modulus of enamel. J Dent Res. 1997;76(10):1690–7. doi:10.1177/00220345970760101101
4. Zhang YR, Du W, Zhou XD, Yu HY. Review of research on the mechanical properties of the human tooth. Int J Oral Sci. 2014;6(2):61–9. doi:10.1038/ijos.2014.21
ABOUT THE AUTHOR
Dr. Tam completed her DDS and her general practice residency in pediatric dentistry at the University of Western Ontario and the University of Toronto, respectively. Her practice has a focus on restorative and cosmetic dentistry. She is well-published in both the local and international dental press, writing articles, reviewing submissions, and developing prototype products and techniques in clinical dentistry. She frequently and continually lectures internationally.
Dr. Tam is the immediate past chairperson and director of the New Zealand Academy of Cosmetic Dentistry. She is one of merely 2 dentists in Australasia who are board-certified, accredited members of the American Academy of Cosmetic Dentistry. Moreover, she maintains Fellowship status with the International Academy for DentoFacial Esthetics.
She sits on the advisory board for Dental Asia and is part of the Restorative Advisory Panel for Henry Schein Dental New Zealand. She sits on the board of Smiles for the Pacific, an educational trust and charity that aims to expand professional dentistry services across the entire South Pacific region.
She is involved with Delta Gamma Sorority and aims to spearhead projects harmonious with Service for Sight in the South Pacific.
She can be reached at clarence.tam@gmail.com.
Disclosure: Dr. Tam receives financial support from VOCO America.












