Walk into many of the dental schools in North America, and one will see cavity preparations being taught that are essentially the same as they were in 1890. In contrast, according to Dr. Marcos Vargas, the University of Iowa School of Dentistry devised a completely different cavity preparation for posterior composites 20 years ago.
Described as the Defect Specific Cavity Preparation, it abandons mechanical retention completely by simply removing caries and then beveling. This preparation is remarkably similar to the Clark Class II cavity preparation first published in 2007 described in this article.
The Bioclear Learning Centers are collaborating with schools to affect a patient-centered outcome for direct composite procedures. These schools include the Roseman University of Health Sciences College of Dental Medicine (South Jordan, Utah), Loma Linda University School of Dentistry (California), Université de Montréal Faculty of Dentistry (Quebec, Canada), and McGill University Faculty of Dentistry (Montreal, Quebec, Canada).
In addition, we are working with GPR programs at the University of Alberta Faculty of Medicine & Dentistry (Edmonton, Alberta, Canada), University of Minnesota School of Dentistry (Minneapolis), University of Texas Health Science Center at San Antonio School of Dentistry, and University of the Pacific Arthur A. Dugoni School of Dentistry (San Francisco). Sseveral other schools are in early stages of adoption.
 |
 |
| Figure 2. Preoperative view of the featured patient case: a failing composite procedure eight years postoperatively with incomplete fractures of the mesiobuccal (MB) and palatal cusps. | Figure 3. Mandatory for our schools, as with every modern composite procedure, is the disclosing of biofilm that is not removed by phosphoric acid and is virtually invisible unless it is disclosed. (Bioclear dual color disclosing agent was used here.) |
 |
 |
| Figure 4. A disclosing solution application magnified the inherent weaknesses of hand-spatulated, layered composite placed in a retentive parallel wall cavity prep that creates tension joints. (Note the cracks that undermined the MB cusp.) | Figure 5. Extra-Large Diamond Wedge (Bioclear) was placed as a “pre-wedge.” Note that the strong pressure of the wedge had already opened up the contact slightly. Pre-wedging throughout the procedure (while cutting the prep) has multiple benefits and is also a mandatory step for dental schools. |
 |
 |
| Figure 6. The cavity was flared with Calla Lilly shape on the palatal and distobuccal (DB) cusps. The MB and DP cusps would then be reduced by a minimum of 2.0 mm for full cuspal overlays. | Figure 7. The contacts were not broken. Larger burs (not shown here) were used for the bulk of the prep and removal of old composite. In contrast, a small coarse diamond (Bur #FSD3F.fg.008 [Komet]) (shown here) was utilized at oblique, safe angles to create the flair of the Clark Class II. |
 |
 |
| Figure 8. After finishing the prep and sanding the gingival area, the Bioclear Blaster was used to clean the prep and remove all biofilm (with a slurry of aluminum tri-hydroxide, air pressure, and water) in the infinity edge zone. The Filtek One/Filtek Bulk Fill Flowable Restorative (3M) was allowed to flow several millimeters past the radius bevel to cover the infinity edge. |
Figure 9. A large Sof-Lex XT Coarse Disk (3M) was used to optimize the previously “burnished” irregular point-contact of the neighboring bicuspid tooth. |
In 2007, we formalized the Clark Class I and Clark Class II cavity preparations, which now represent a foundation for progress. These new preparations are based on monumental changes that have occurred since the time of G.V. Black. This article addresses four of these changes that are accounted for in the Clark Class I and Clark Class II cavity preparations and include an example case.
Modern Engineering
A critical missing piece of dental education is that of engineering. In Black’s era, the level of engineering was nothing like it is today. The Black Class II is essentially a Mortis and Tenon interface, commonly used in cabinetry making.
Today, we understand that multi-cusped teeth are naturally put into tension, and these traditional preps further complicate an already tenuous engineering problem. When a traditional Class I or Class II restoration is loaded thousands of times, cyclic fatigue rears its ugly head, and a naturally brittle complex, the human tooth, becomes a profoundly weakened complex. Adhesive bonding alone cannot mitigate this weakening.
The outcome studies support what engineers have been trying to tell us for decades: Our long-used traditional cavity preparations and endodontic accesses are not properly designed from the perspective of modern engineering principles.
The Effect of Fluoride and Abundant Fermentable Carbohydrates
Teeth are decaying differently today than in Black’s era. Nowadays, clinicians routinely encounter teeth that are barely cavitated because of the effect of fluoride on the outs
ide of the tooth, but with catastrophic infected dentin internally because of the unfortunate simple carbohydrate-laden diets prevalent in these times.
The Importance of C-Factor
In early 2019, Bioclear and 3M formed an alliance to teach the Bioclear Method and embark on third-party research to substantiate the various aspects of the Bioclear Method.
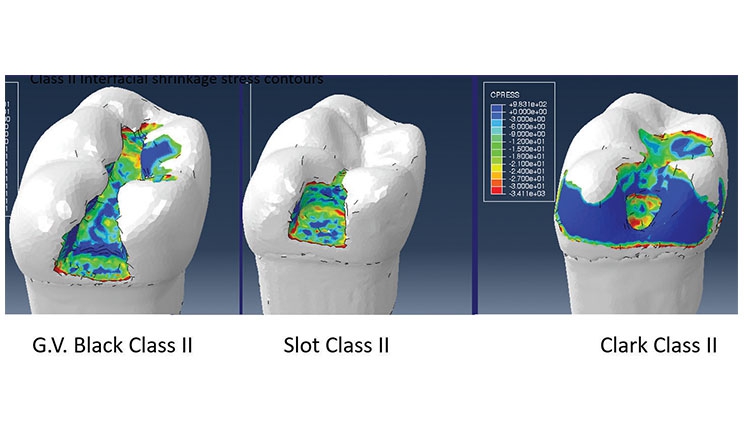
Figure 1 shows Finite Element Analysis of the anticipated shrinkage stress of three different cavity preparations. These images demonstrate the ideal pairing of the Infinity Edge, non-retentive Clark Class II preparation with the polymerization-shrinkage element of composite resins.
Additionally, the large areas of enamel rod engagement at 90° to the enamel rod openings are a more logical adhesive situation than dentin bonding with high C-Factor and tension as the composite shrinks away from the cavity walls in the 2 preparations on the left.
 |
 |
| Figure 10. The final blasted Clark Class II preparation (note that blasting helps to visualize the dentinal cracks present). | Figure 11. Palatal view of the Biofit 6.5 mm Matrix (Bioclear) and Extra-Large Diamond Wedge (Bioclear). Note the cuspal reduction of the MB and DP cusps along with the radius bevel areas. |
 |
 |
| Figure 12. Buccal view of the assembly. The severely cracked MB cusp was reduced by 3.0 mm, and then radius beveled. We have a new lexicon, and people will need to adopt it. A radius bevel is a convex bevel that becomes tangential to two skew lines or surfaces: in this case, the natural surface of the tooth and the initial cut into the tooth to access dentinal decay. A radius bevel is a convex bevel that becomes tangential to two skew lines or surfaces: in this case, the natural surface of the tooth and the initial cut into the tooth to access dentinal decay. | Figure 13. Full assembly with the yellow premolar Twin Ring Separator (Bioclear). The space was technically a bicuspid space, so the bicuspid separator was used to allow the strongest separation pressure. |
 |
 |
| Figure 14. Go/No-Go Probe (Bioclear) was used to measure the anticipated height of the interproximal area. Because it was no taller than the 5.0-mm height of the yellow band, the Filtek One was used here with no layering. This composite has a full 5.0-mm depth of cure when true three-point curing is employed. The buccal and lingual portions of three-point curing are made possible with the clear Biofit Matrix. | Figure 15. Magic Mix Pre-polish (Bioclear) was applied in a disposable prophy cup. Traditional polishers have limited shapes and were not designed to polish the large convex surface areas and interproximal areas of these “wraparound restorations.” |
 |
| Figure 16. Final polish of the Filtek One and infinity edge margins with the RSP diamond impregnated cup (Rock Star Polisher [Bioclear]). The patient had no postoperative sensitivity and reported that, after the procedure, he could chew whatever he wants with full confidence. He was happy that the restoration had better margins than a crown and would be healthier for him over time. |
Adhesion
Why do schools cling to preparations that are designed with mechanical retention for an adhesive material? Certainly, adhesion alone has not seemed to provide predictable long-term success in posterior teeth. Composite restorations are falling out of slot preps.
The problem is that enamel cohesion and dentin adhesion are not the same thing. Traditional retentive (Black and slot) cavity preps unfortunately maximize dentin engagement and minimize enamel engagement. For practicing clinicians, “in enamel we trust.”
In the featured case here, I am retreating a failed composite procedure. We need to stop calling it a failing composite or a failing restoration (Figures 2 to 16). In fact, it is not the material that is failing, per se. It is a much deeper and more troubling problem than that.
The patient is Dr. Pat Roetzer. (Pat is working diligently at University of the Pacific, where he is a faculty member, to implement the Bioclear method.) His tooth was originally treatment planned by a local prosthodontist for a crown.
Instead, Pat opted for this Clark Class II, cuspal overlay/Calla Lily preparation with the subsequent use of the Bioclear Matrix system and injection molded (heated) Filtek One Bulk Fill Restorative (3M) plus Bulk Fill Flowable Restorative (3M) and Scotchbond Universal Adhesive (3M).
Used correctly in a modern Venn diagram, our outcome study is showing a high survival rate for the Clark Class II procedures at more than 10 years. In addition, there are a handful of studies showing long-term success of Class II composite restorations when done very carefully.
The problem is that the Class II composite has so many points of failure that a new and more prescriptive and simplified approach is needed to achieve Class II composite restorations that will not only last for decades with beautiful embrasures and margins but also within the clinical implementation realities of the everyday practice of dentistry.
Closing Comments
The solution to the fairly woeful state of Class II composites is not likely to be found in some novel new adhesive, filler particle, resin chemistry, or combination thereof.
The true paradigm shift starts with a modern cavity preparation and a realization that composite is not a good “amalgam replacement.” Hand-packing cold paste composite into a boxy prep with abrupt margins is fractally wrong. This brief article serves to outline a framework for change.
The reader is encouraged to learn more at Bioclear Learning Center, online videos and articles at dentistrytoday.com, and 3M/Bioclear regional hands-on courses.
Dr. Clark maintains a private practice in Tacoma, Wash, and is the founder of the Academy of Microscope Enhanced Dentistry. He is also a course director at the Newport Coast Oral Facial Institute in Newport Beach, Calif, and director of the Bioclear Learning Center in Tacoma. Dr. Clark’s main areas of interest include the redesigning of restorative preparations and endodontic access preparations. He can be reached at bioclearmatrix.com.
Disclosu
re: Dr. Clark is the owner of Bioclear Matrix Systems.
Related Articles
Incommensurability in Endodontics: The Role of the Endodontic Triad


