Fixed, Full-Arch Treatment With a Cement-Retained Prosthesis
INTRODUCTION
Dental implants have predominantly used titanium alloys for the past 50 years. Ever since the introduction of the All-on-4 treatment by Maló et al1 20 years ago, titanium alloy implants have been established as the cornerstone for full-arch, implant-supported restorations. However, over the last 15 years, zirconia implants have undergone significant evolution,2 emerging as a reliable—though more complex—option for full-arch, implant-supported restorations.3,4 This progress, coupled with the success of ceramic implants, has led to growing patient demand for comprehensive, metal-free implant solutions in full-arch cases.
The reasons why patients seek metal-free dental implants are metal allergies,5 systemic inflammation, exacerbation of chronic diseases, or previous failures with titanium implants. However, from the practitioner’s standpoint, the most prevalent complications associated with titanium dental implants are peri-implant mucositis6,7 and peri-implantitis. Reports suggest peri-implant mucositis occurs in 40% to 80% of titanium implant patients, while peri-implantitis affects 10% to 56% of implant patients.8
Even though the etiology of peri-implant disease is multifactorial, more and more evidence has emerged correlating peri-mucositis and peri-implantitis to titanium alloy degradation9 and the cytotoxic effects of metal particles in the local tissues.10 Greater levels of dissolved titanium were detected in submucosal plaque around implants with peri-implantitis when compared to healthy implants.11 These findings continue to explore and establish the clear connection between titanium dental implants and the prevalence of peri-implant disease.
In zirconia implants, the prevalence of peri-implant disease seems to be less prevalent. One well-cited study reported that clinical experience with zirconia implants indicates that peri-implantitis seems to be less of a problem with ceramic implants than with titanium implants.2 A more recently published study showed zero peri-implantitis during a followup of ceramic implants for up to 12 years.12 Therefore, ceramic implants can potentially be a solution for this current global epidemic of peri-implantitis.13
The first 2 articles in this series (published in the March 2023 and October 2023 issues of Dentistry Today) focused on single-unit; extended edentulous; and full-mouth, removable treatment with ceramic implants. The following case report illustrates a full-mouth reconstruction with use of 100% metal-free zirconia dental implants to achieve a predictable and clinically optimal result.
CASE REPORT
Diagnosis
A 54-year-old female patient presented to our office for an evaluation of her existing dental condition in both her maxillary and mandibular arches. The patient had multiple provisional restorations on her upper anterior teeth (Figures 1 to 3) and was looking to restore her dentition to proper form, function, and aesthetics.
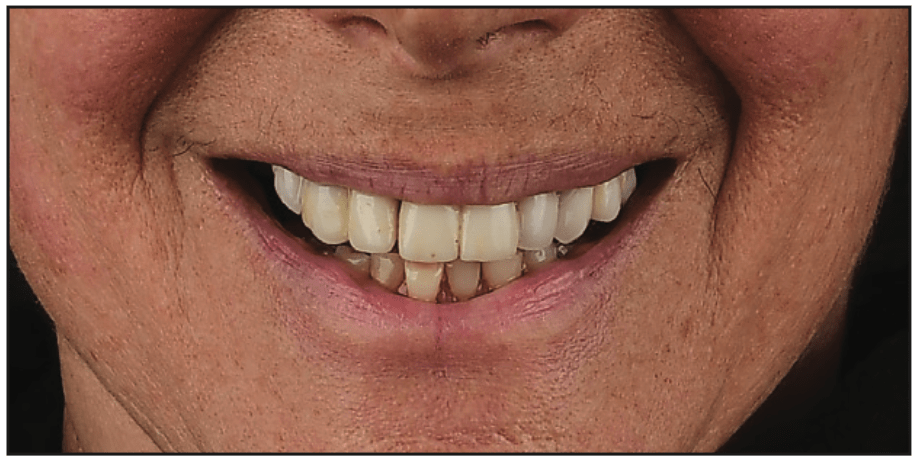

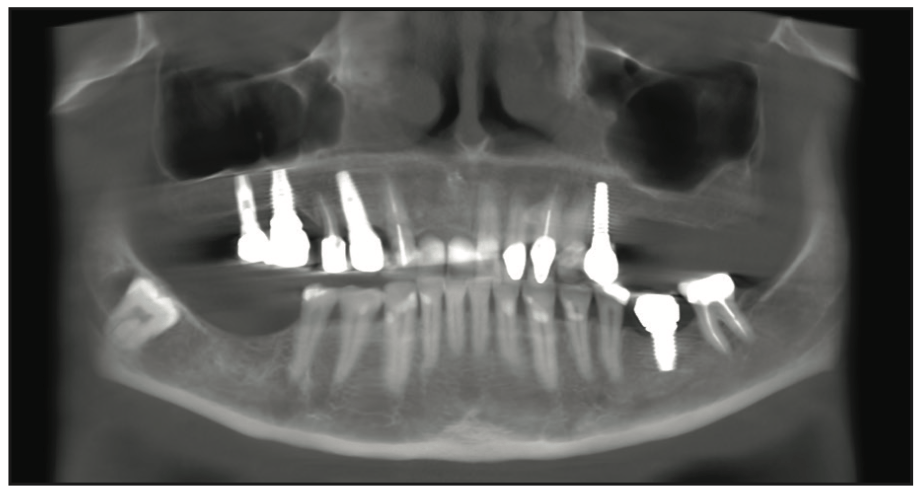
Upon clinical examination, deep periodontal probing depths with bleeding were present around implant Nos. 2, 3, 5, and 19, indicating localized peri-implantitis and peri-mucositis. The loss of dentition in various posterior quadrants resulted in the collapse of vertical dimension, causing further force and wear on the anterior teeth and restorations. Recently placed implant No. 13 had a poorly contoured provisional due to lack of restorative space. The patient had generalized wear and fractured restorations due to parafunctional habits and decay on the lower anterior teeth.
Relevant medical history included the following autoimmune conditions: Crohn’s disease, Hashimoto’s thyroiditis, and plaque psoriasis localized to the head and neck area. The patient, who herself was a health practitioner, described her main concern as inflammation in her mouth, which contributed to the rise of systemic inflammatory cytokines and potentially negatively affected her systemic health.
Treatment Plan
Due to a history of peri-implantitis, metal-free ceramic implants were requested, which the patient had difficulty finding for full-mouth reconstruction. All risks, benefits, and viable alternatives of other treatment options were reviewed with the patient. It was decided that full-mouth reconstruction would provide the best prosthetic, functional, and aesthetic outcome for the patient with an excellent long-term prognosis. The treatment entailed the removal of all failing teeth and implants and subsequent replacement with a fixed, full-arch, ceramic, implant-retained prosthetic. The approach in the mandible was to place zirconia implants in the posterior regions and place ceramic-bonded restorations on the lower natural teeth.
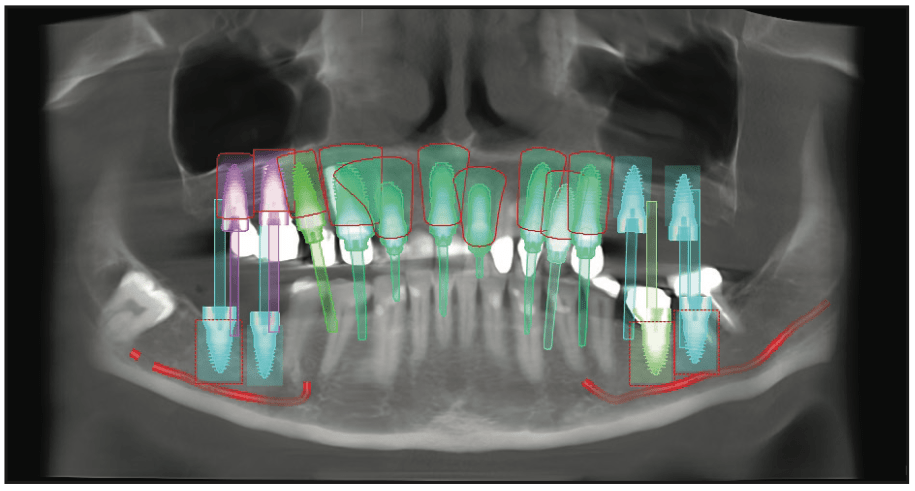
PreVu dental software (PreVu Software) was used to perform a simulated smile design (Figure 4) that guided the dental laboratory in creating a proper diagnostic wax-up for the case, which also allowed the patient to envision herself with her new smile and discuss aesthetic goals of the case. Using Planmeca Romexis CBCT planning software (Planmeca), the zirconia implants were virtually positioned, determining the exact placement sites and sizes of the ceramic implants (Figure 5). The dental implants chosen for this reconstruction were SDS Implants (Swiss Dental Solutions) monobloc, for immediate loading, and 2-piece, for delayed loading.
Surgery
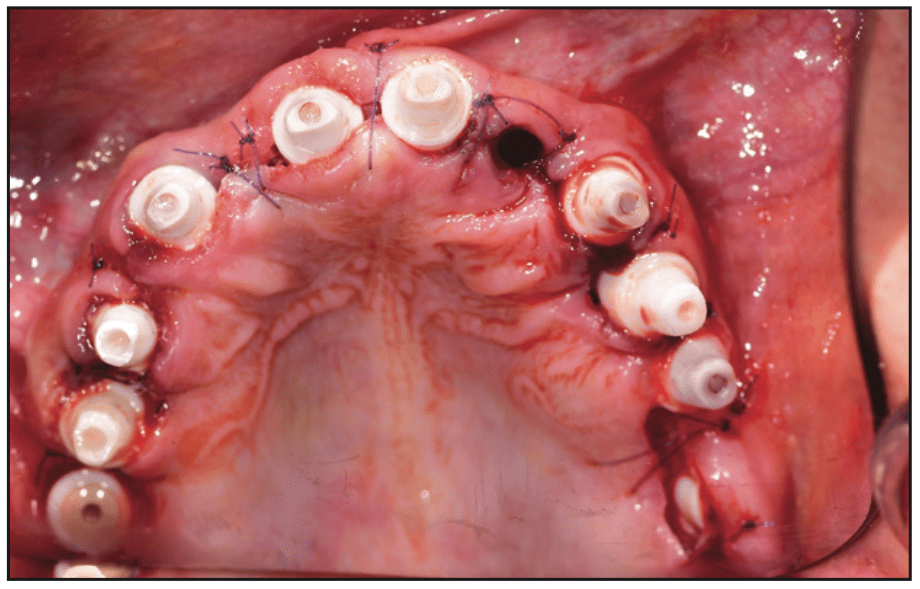
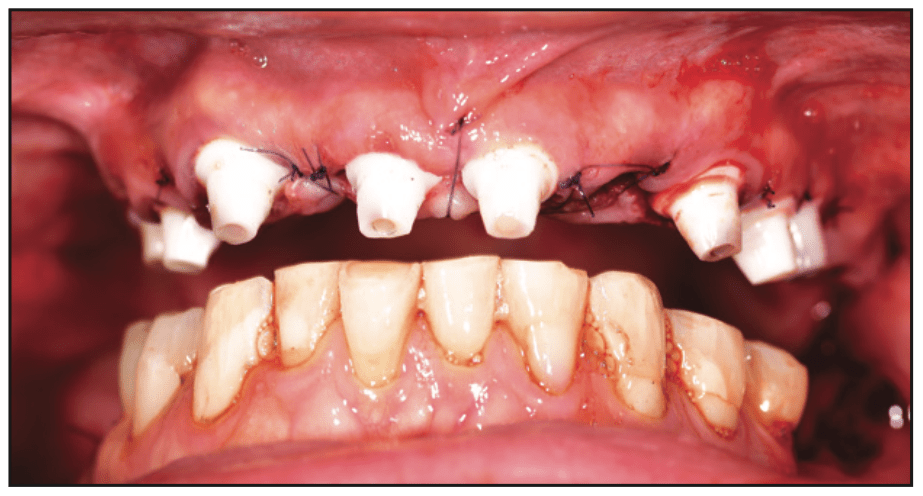
On the day of surgery, the patient was sedated, and local anesthesia was administered. Natural teeth were extracted with the use of elevators and forceps. Titanium implants were explanted by a reverse torque technique using a fixture removal kit (DMZ Dental). Non-restorable ceramic implant No. 13 was explanted using piezo surgery initially, then elevators and forceps. Osteotomy and placement of the new implants were performed by a socket-guided technique. Implants were placed at the tooth extraction sites, implant removal sites, or adjacent to an extraction site (Figure 6). A-PRF membranes were used in the extraction sockets to speed up the healing process and as a graft material for the internal sinus lift site Nos. 2, 3, 14, and 15. Soft tissue was re-approximated around the implants (Figures 7 and 8) using Glycolon 4.0 sutures (Osteogenics). Implant restorative posts and collars were adjusted to achieve a path of draw for the cementable temporary restoration. The maxillary arch was scanned using an intraoral i700 scanner (Medit). The provisional restoration was designed by GALA dental arts laboratory and produced in-house with a Flexcera Smile Ultra+ resin (Desktop Health) on a Max 3D printer (Asiga). The temporary was cemented using Bifix Temp cement (VOCO), and the occlusion was adjusted to spread the occlusal forces evenly during the healing phase (Figure 9).


Prosthetics Phase
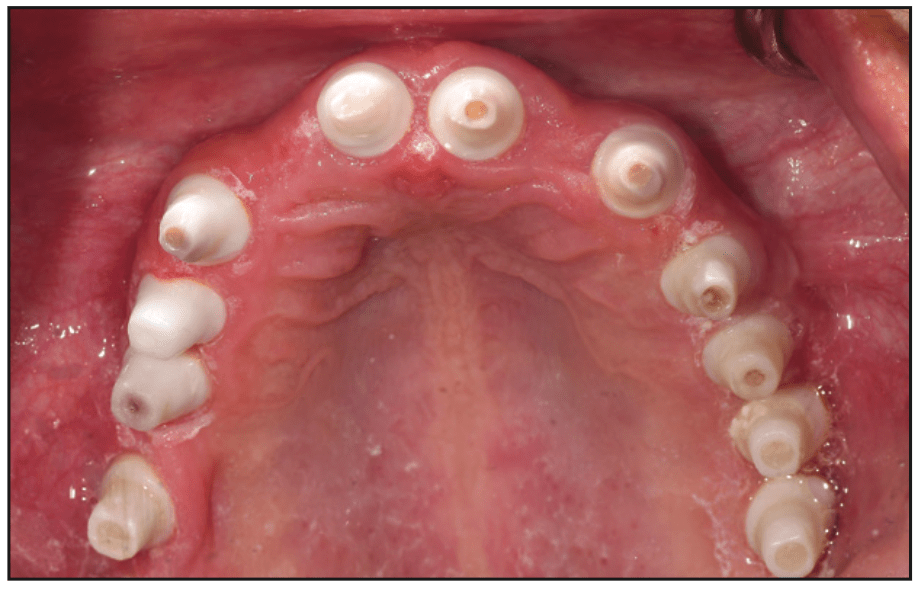
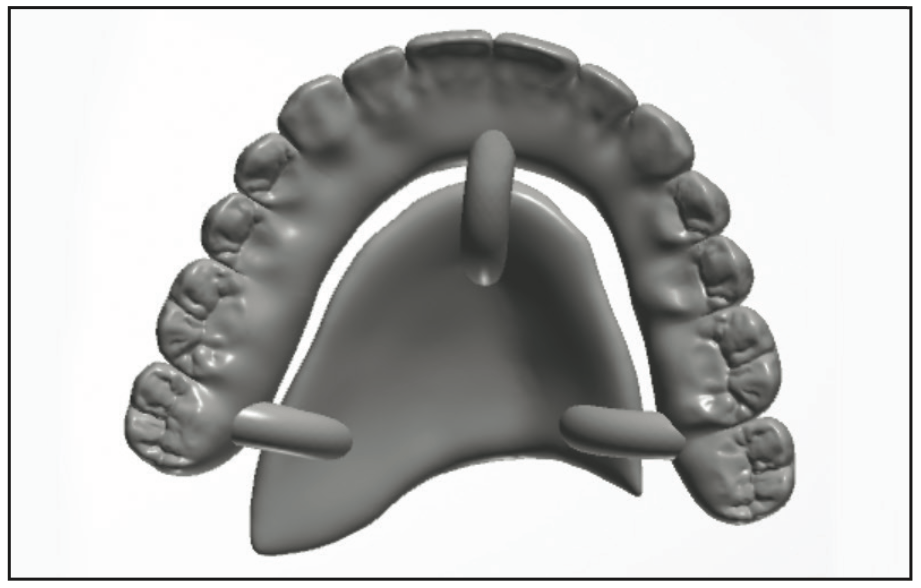
The final restorative phase of treatment was initiated after 5 months of healing to ensure full osseointegration. Temporary restorations were removed, and implant integration was verified using the Periotest device (Medizintechnik Gulden eK). Posts were delivered on the 2-piece implants, at site Nos. 2, 3, 14, 15, 18, 19, 30, and 31, using Ketac GI cement (Solventum) and PEEK screws torqued to 5 Ncm2 while the cement was setting. Implants were modified to ensure that the collars were in line with the level of the soft tissue (Figure 10). Mandibular anterior teeth and mandibular posterior implants were prepared using preparation guides to ensure adequate occlusal and facial reduction. A final intraoral scan of the preparations was taken using the i700 scanner. Temporary restorations were fabricated to an ideal vertical dimension. For the fabrication of the maxillary arch, a 3D printed spider shell (Figure 11) was used and relined with Structur bis-acryl material (VOCO). The palatal index ensured proper placement of the temporary bridge over the preparations. The provisionals for the lower arch were made using VPS putty mold and Structur bis-acryl material (Figure 12).

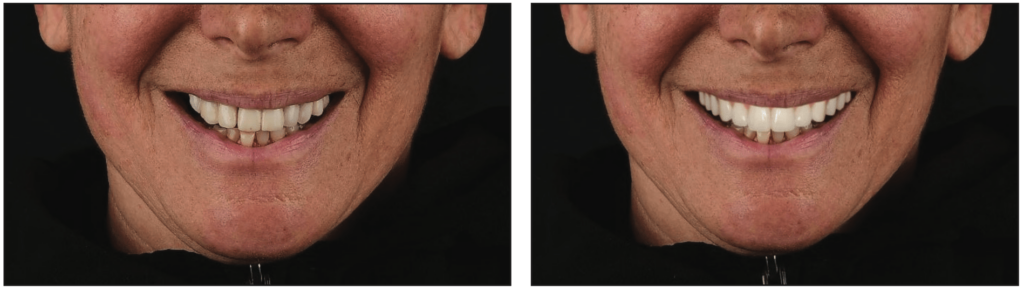
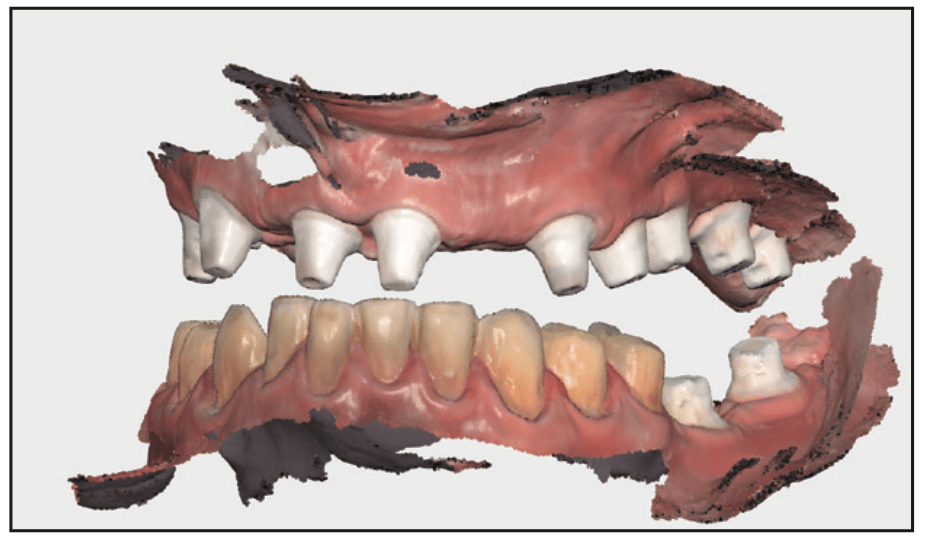
The temporary restorations were scanned using Medit Software and indexed to the preparation scans. Bite registration and the new vertical dimension were transferred from the temporary restorations to the final scans (Figures 13 and 14). Full-face photos were taken to evaluate the harmony with the facial structures and communicate tooth position changes needed for the final prosthesis fabrication (Figure 15).


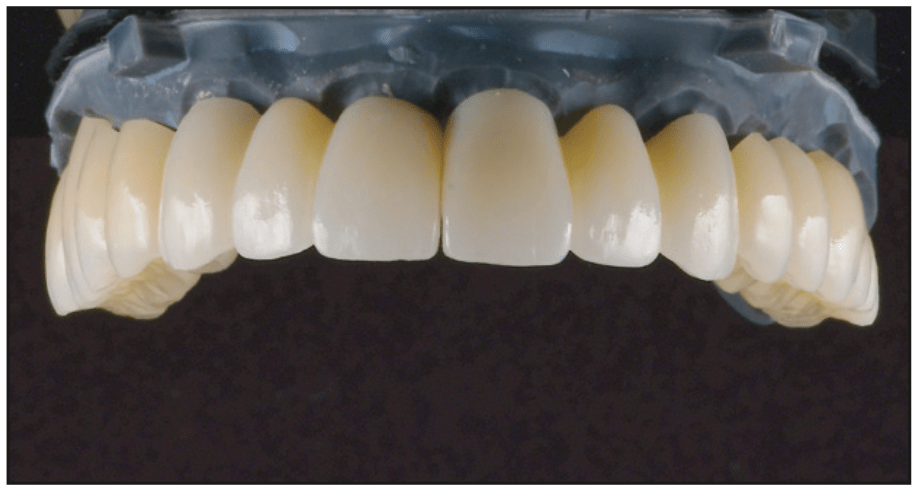
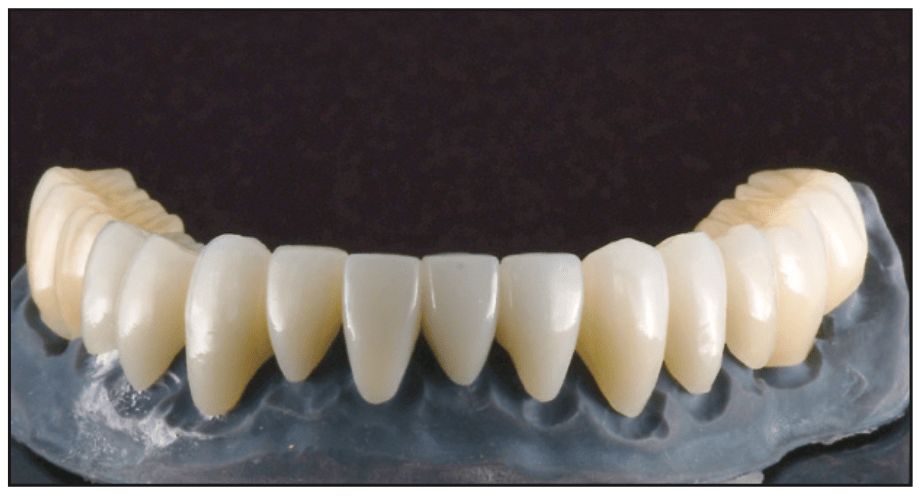
Laboratory Considerations
Final intraoral scans of preparations, temporary restorations, and the bite registration were forwarded to the dental laboratory (GALA Dental Art) along with the photos and detailed changes requested. The maxillary final restoration was fabricated in 4 fixed partial denture segments (2-3-4-5), (6-7p-8), (9-10p-11), and (12-13-14-15). The material used for the maxillary restoration was a combination of monolithic zirconia for the molar region and porcelain layered zirconia for units No. 5 to 12 to enhance aesthetics (Figure 16). The lower arch was restored with splinted monolithic zirconia crowns on implant Nos. 18 and 19 and 30 and 31. Natural teeth restorations on teeth Nos. 20 to 28 were fabricated with IPS e.max (Ivoclar) pressed layered ceramic to provide enhanced bonding strength to the tooth structure (Figure 17).
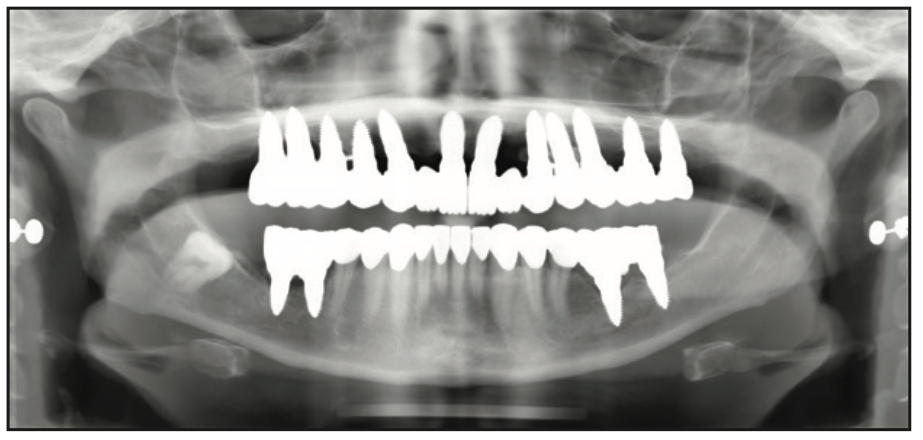
Delivery
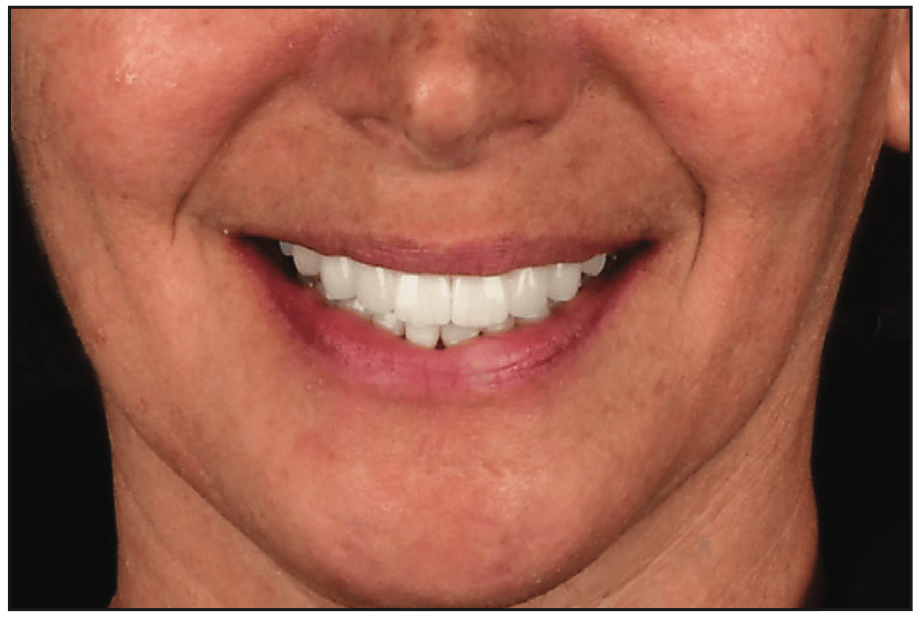
The patient returned for final restoration placement after 3 months due to her active travel schedule. Provisional restorations were removed, along with all remaining temporary cement. The final restorations were verified for fit. The patient examined the appearance and aesthetics of the final prosthetics and approved them for final cementation. Implant-supported zirconia restorations were cemented with RelyX Unicem 2 (Solventum), and the lower e.max restoration over natural teeth was bonded using ScotchBond universal (Solventum) and RelyX Veneer Cement (Solventum). A canine guidance occlusal scheme was used for the rehabilitation to reduce lateral forces on the posterior restorations to help prevent fracturing of the prosthetics. After the final delivery, an occlusal guard was also delivered to the patient with strict postoperative care and hygiene instructions. The final result was a complete functional and aesthetic rehabilitation that exceeded the patient’s own expectations (Figures 18 to 20).

DISCUSSION
Zirconia implants have shown high levels of success and survival in delayed- and immediate-loading cases.14-16 However, unlike titanium implants, which have multiple restorative abutment options, specifically for difficult-to-restore or surgically challenging cases, zirconia dental implants have limited restorative options. Multi-unit abutments, custom abutments, and non-engaging screw-retained abutments that are often used in full-arch, fixed prosthetic restorations are not widely available for zirconia implants. The particular case presented in this article was completed with a combination of one-piece mono-block ceramic implants and 2-piece ceramic implants with a combination of cementable and screw-retained posts. The main drawback of treatment with one-piece ceramic implants is the need to place the implants perfectly parallel to achieve a path of draw for a cemented prosthesis. In the hands of a skilled and experienced zirconia dental implant practitioner, much is possible with zirconia dental implants but often requires a higher degree of planning; more precise implant positioning; and achieving the desirable outcome of predictability, stability, and longevity. The SDS zirconia implant model that was used for this case had a dynamic thread tailored for immediate implantation and achieved the high primary stability needed for immediate loading. The implant had a large tulip, contributing to ease of preparation and customization of the restorative portion of the implant and enhancing emergence profile. A one-piece implant design streamlines the immediate temporization process after the surgery, as there is no need to deliver an abutment on the implant prior to placement of the temporary restoration. In the posterior region, due to the need to perform an internal sinus lift procedure, an SDS 2-piece zirconia implant design was chosen to minimize the tongue and mastication forces applied to the implants during the healing phase and to simultaneously prevent implant loss due to early loading.
Splinting implants helps distribute the forces exerted during biting and chewing across multiple implants and minimize micro-movements. This prevents excessive stress on individual dental implants and the supporting bone. This can be an important factor for implant success, as excessive movement can lead to bone resorption and compromise long-term stability.
CONCLUSION
With the evolution of ceramic implantology, various implant materials and restorative options are available to patients seeking full-arch implant solutions. Deciding which material and method to use in each case depends on clinical and patient demands. The treatment plan for this case proved to be successful because it achieved the patient’s goal of having an implant-supported, fixed prosthesis on 100% metal-free zirconia implants with healthy hard- and soft-tissue integration.
REFERENCES
- Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):2-9. doi:10.1111/j.1708-8208.2003.tb00010.x
- Cionca N, Hashim D, Mombelli A. Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000. 2017;73(1):241–58. doi:10.1111/prd.12180
- Sivaraman K, Chopra A, Narayan AI, et a. Is zirconia a viable alternative to titanium for oral implant? A critical review. J Prosthodont Res. 2018;62(2):121–33. doi:10.1016/j.jpor.2017.07.003
- Andreiotelli M, Wenz HJ, Kohal RJ. Are ceramic implants a viable alternative to titanium implants? A systematic literature review. Clin Oral Implants Res. 2009;20(Suppl 4):32-47. doi:10.1111/j.1600-0501.2009.01785.x
- Sicilia A, Cuesta S, Coma G, et al. Titanium allergy in dental implant patients: a clinical study on 1500 consecutive patients. Clin Oral Implants Res. 2008;19(8):823–35. doi:10.1111/j.1600-0501.2008.01544.x
- Heitz-Mayfield LJA, Salvi GE. Peri-implant mucositis. J Clin Periodontol. 2018;45(Suppl 20):S237-S245. doi:10.1111/jcpe.12953
- Froum SJ, González de la Torre E, Rosen PS. Peri-implant mucositis. Int J Periodontics Restorative Dent. 2019;39(2):e46-e57. doi:10.11607/prd.3976
- Atieh MA, Alsabeeha NH, Faggion CM Jr, et al. The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol. 2013;84(11):1586–98. doi:10.1902/jop.2012.120592
- Noronha Oliveira M, Schunemann WVH, Mathew MT, et al. Can degradation products released from dental implants affect peri-implant tissues? J Periodontal Res. 2018;53(1):1-11. doi:10.1111/jre.12479
- Messous, R., Henriques, B., Bousbaa, H. et al. Cytotoxic effects of submicron- and nano-scale titanium debris released from dental implants: an integrative review. Clin Oral Invest. 2021;25, 1627–1640. https://doi.org/10.1007/s00784-021-03785-z
- Safioti LM, Kotsakis GA, Pozhitkov AE, et al. Increased levels of dissolved titanium are associated with peri-implantitis — a cross-sectional study. J Periodontol. 2017;88(5):436–42. doi:10.1902/jop.2016.160524
- Karapataki S, Vegh D, Payer M, et al. Clinical performance of two-piece zirconia dental implants after 5 and up to 12 years. Int J Oral Maxillofac Implants. 2023;38(6):1105-1114.
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42(Suppl 16):S158–71. doi:10.1111/jcpe.12334
- Borgonovo AE, Ferrario S, Maiorana C, et al. A clinical and radiographic evaluation of zirconia dental implants: 10-year follow-up. Int J Dent. 2021;2021:7534607. doi:10.1155/2021/7534607
- Kiechle S, Liebermann A, Mast G, et al. Evaluation of one-piece zirconia dental implants: An 8-year follow-up study. Clin Oral Investig. 2023;27(7):3415–21. doi:10.1007/s00784-023-04935-1
- Grassi FR, Capogreco M, Consonni D, et al. Immediate occlusal loading of one-piece zirconia implants: five-year radiographic and clinical evaluation. Int J Oral Maxillofac Implants. 2015;30(3):671–80. doi:10.11607/jomi.3831
ABOUT THE AUTHORS
Dr. May received his DMD degree from the University of Connecticut School of Dental Medicine and completed his GPR residency at BronxCare Health System (formerly Bronx-Lebanon Hospital Center) in New York City. After working in private practice for a number of years, Dr. May started his own practice in Connecticut focusing on full-mouth reconstruction, oral implantology, and metal-free dentistry using the latest digital dentistry techniques and technology. He is an accredited member of the International Academy of Oral Medicine and Toxicology, a board member of the International Academy of Ceramic Implantology, and board-certified in integrative biologic dental medicine. He can be reached at drmaynaturaldentistry@gmail.com.
Dr. Noumbissi obtained his DDS degree from Howard University in Washington, DC. He attended the prestigious Loma Linda University full-time Graduate Program in Implant Dentistry, where he received 3 years of formal training in dental implantology, which culminated with a certificate in Implant Dentistry and an MS in Implant Surgery. He is a clinical and experimental researcher and author and has published book chapters and articles on implant dentistry with a focus on ceramic implants in peer-reviewed dental journals. He is a visiting professor at the University of Milan, an adjunct professor at the University of Chieti-Pescara in Italy, and a visiting researcher in the ceramic materials department at INSA Lyon in France. Dr. Noumbissi is the founder and current president of the International Academy of Ceramic Implantology, which is an independent association focused on metal-free implants and bioceramics in dental implantology. He is a Fellow and Ambassador at the Clean Implant Foundation, whose mission is to assess the production quality and purity of commercially available dental implant surfaces. Dr. Noumbissi has been practicing and educating dentists on metal-free implantology since 2009. He has extensive experience with ceramic implants, and his opinions and expertise are often sought by both clinicians and manufacturers. His practice is located in Silver Spring, Md. He can be reached at sammy@iaoci.com.
Dr. Boyer graduated from the University of California, Los Angeles (UCLA) School of Dentistry in 2008 and completed 2 hospital-based GPR training programs at Cedars-Sinai Medical Center and the VA Healthcare system, where he received advanced training in oral and maxillofacial surgery, complex and comprehensive treatment planning, and the placement and restoration of dental implants. Dr. Boyer has been in private practice in Los Angeles since 2010. In 2011, Dr. Boyer became a faculty member at the UCLA School of Dentistry, where he teaches dental students, as well as the residents in the Advanced Education in General Dentistry program. From 2018 to 2020, Dr. Boyer also trained at the UCLA Dental Implant Continuum, which is based on scientific research, current standards and protocols, and cutting-edge research and technology. In 2020, Dr. Boyer was invited to be one of 4 investigators in a 5-year, worldwide, multicenter ceramic implant osseointegration and stability study led by the International Academy of Oral Ceramic Implantology (IAOCI) and the Zirconia Implant Research Group. Dr. Boyer is active in multiple dental implant organizations and was recently appointed a board member of the IAOCI. He can be reached at dentist@ucla.edu.
Disclosure: Dr. May is a KOL and US Ambassador for Swiss Dental Solutions. Dr. May has not received any compensation for writing this article. Drs. Noumbissi and Boyer report no disclosures.



