INTRODUCTION
The use of provisional restorations is primarily seen as an interim step of transitioning treatment to the final outcome in the most expedient way possible. Provisional restorations serve several important purposes. They protect the prepared surfaces of the teeth from the dynamic assault of the oral environment during the time frame from preparation to definitive cementation of the final restorations. They provide a template for directing treatment outcomes aesthetically, phonetically, and functionally. They can be utilized as a confirmation tool prior to cementation in accessing uniform clearance for the final restorative material. They serve to secure and stabilize tooth positions. Lastly, segmental removal of the provisional restorations can provide validation of the definitive restorations for duplicating key factors such as incisal edge position, the midline, or the occlusal plane established in the transitional phase. The desired properties of a provisional material include biocompatibility, pleasing aesthetics, fracture resistance, ease of fabrication, the ability to shape and polish, nonporousness, dimensional stablility, a short setting time, and reparability.
 |
 |
| Figure 1. A long-span provisional restoration (LuxaTemp [DMG America]), reinforced with cast metal bars, secured on the central incisor and first molar abutments (4-tooth edentulous span, bilaterally), and used over several years during grafting and implant integration in the bicuspid and cuspid regions. |
Figure 2. Indirectly fabricated and opaqued metal bars were used to reinforce the long-span provisional bridge. |
A Brief History of Dental Materials Used for Provisionals
Traditionally, provisional restorations were fabricated using methyl methacrylate, ethyl methacrylate, or vinyl ethyl methacrylate. The chosen material was used to create a shell of the desired shape(s) and then relined intraorally or in the laboratory to fit the prepared teeth. Several challenges have existed with using methacrylate: the additional laboratory time required to create the acrylic shell, managing intaglio contours that did not allow the shell to fully seat intraorally, and accommodating for margin location mismatched with the margin location of the prepared teeth. Additionally, the heat and shrinkage of methacrylate during the curing phase of the material required more focused time from the operator to minimize exposure of the prepared teeth to excessive heat and to avoid locking the provisional restoration on the tooth preparation.1 Alternate methods of fabrication include prefabricated resin, polycarbonate, acrylic, or metal shells that can be relined intraorally.
The introduction of bisacryl provisional materials more than 20 years ago offered several advantages over traditional methacrylates, as well as some disadvantages. Importantly, the generation of heat and shrinkage upon curing methacrylates is comparatively reduced with bisacryls.1 Bisacryls also provide faster set times over methacrylates. These features allow provisional restorations to be fabricated intraorally more efficiently and with greater predictability. The downside of bisacryls is that these materials tend to be more brittle than methacrylates.2 Bis-GMAs have many of the positive features of bisacryl materials but may offer more resiliency.3 Even so, the flexural load of bisacryl and Bis-GMA appears adequate to serve the demands (degree of load and time under load) for the average provisional restoration. As a result, bisacryl and Bis-GMA materials have become the preferred choice for the chairside fabrication of provisional restorations over the last 2 decades.
Occasionally, there is a desire for a provisional material that provides greater resistance to fracture. This may be due to the size or span of the restoration, the length of time the restoration is anticipated to be of service, and/or the functional demands placed on the restoration. Scenarios that come to mind include the need to stage treatment over time for financial considerations, benefit vs value decisions for medically compromised and elderly patients, deciduous teeth, and the desire for fixed provisionals during the transition to implant-supported restorations (Figure 1). Greater flexural strength of both methacrylates and bisacryls can be enhanced by incorporating fibers or metal substructures into the restorations (Figure 2).4-6 The downside of this approach includes additional steps, time, and costs. Likewise, CAD/CAM-generated PMMA and composite-based materials offer higher mechanical strength but require additional steps, time, and costs over direct approaches.7
Introduction of a Newly Formulated Long-Term Provisional Material
Newer materials and techniques that utilize the ease, efficiency, and economy of a chairside approach are being developed to minimize areas of compromise and maximize areas of benefit. One such example is LuxaCrown (DMG America), a higher-strength material designed for chairside fabrication. The material is advertised to meet aesthetic demands while simultaneously providing increased flexural strength and fracture toughness. Although LuxaCrown is in the same family of materials by DMG America (eg, Luxatemp, Luxatemp Plus, and Luxatemp Ultra), it is more highly filled to provide greater longevity. In vitro testing by the manufacturer suggests the material can provide up to 5 years of service. As a long-time user of Luxatemp (more than 20 years now), I was interested in how the LuxaCrown material compared to it in handling, aesthetics; and, of course, serviceability.
CASE REPORTS
Case 1
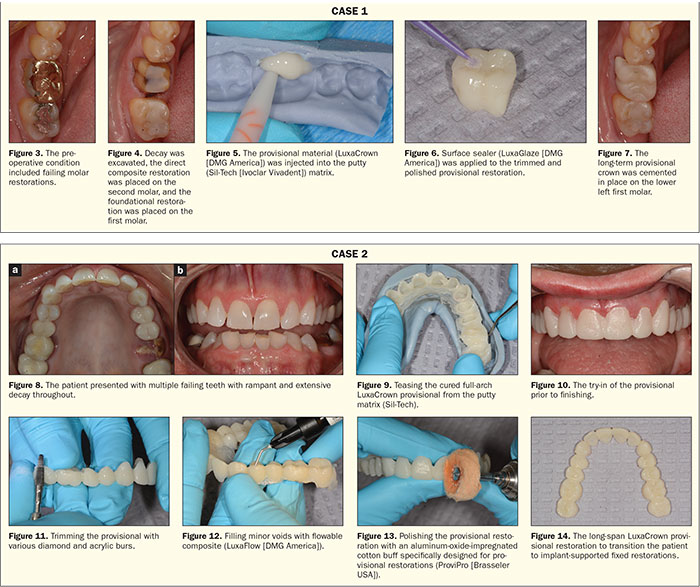
A patient presented with failing restorations on his lower left molars. The second molar displayed a cracked alloy restoration with recurrent decay, and the first molar displayed a failing gold onlay with faulty margins and recurrent decay (Figure 3). The patient, although concerned with the decay on both teeth, was not financially prepared at the time of the appointment to proceed with replacing the indirect restoration on the first molar. It was decided to remove the decay on both teeth and place a direct composite on the second molar and a long-term provisional restoration on the first molar. The patient understood that he, when financially able, would eventually need to proceed with a more permanent solution for the first molar.
The failing restorations were removed from both teeth, and the decay was excavated. The second molar was restored using direct composites (Bisfil 2B [BISCO Dental Products] and Filtek Supreme Plus [3M]). A foundational restoration was placed in the first molar (Bisfil 2B) prior to preparing the tooth for an indirect restoration (Figure 4). Next, a putty matrix (Sil-Tech [Ivoclar Vivadent]) of the modified preoperative anatomy was filled with the LuxaCrown long-term provisional material (Figure 5) and seated firmly over the prepared tooth. The matrix was removed from the mouth when the provisional material reached its initial set and then was allowed to ful
ly cure within the matrix extraorally. The long-term provisional restoration was trimmed and polished, and a surface sealer (LuxaGlaze [DMG America]) was applied and light cured prior to cementation (Figure 6). The restoration was cemented (CLING2 [CLINICIAN’S CHOICE Dental Products]), and the occlusion was checked and refined (Figure 7).
 |
Case 2
A patient presented with rampant decay, partial edentulism, and several hopeless teeth (Figure 8). Due to the patient’s high risk for biomechanical breakdown, the treatment plan would be to move toward implant-supported restorations. The patient wished to avoid removable appliances during the transition to implant-supported restorations. The decision was made to place fixed provisionals in both arches in preparation for tooth extraction, grafting, and implant placement. The implants were planned for the first molar, first bicuspid, and cuspid regions in both arches.
The maxillary teeth were prepared for full-coverage restorations. Foundational restorations were done only to the extent needed to avoid undercuts since all of the teeth would eventually be extracted. A putty matrix (Sil-Tech) fabricated over the diagnostic mockup was filled second molar to second molar with the LuxaCrown long-term provisional material, then seated firmly over the prepared teeth. The matrix was removed from the mouth when the material reached its initial set and allowed to fully cure extraorally. The full-arch restoration was then teased from the matrix (Figure 9) and inserted once again over the prepared teeth to confirm complete seating (Figure 10). The restoration was removed from the try-in and then trimmed extraorally using carbide and acrylic burs (Brasseler USA) (Figure 11). Any minor voids were filled with a flowable light-cure composite (LuxaFlow [DMG America]) (Figure 12). The restoration was polished using an aluminum-oxide-impregnated polishing buff (ProviPro Buff [Brasseler USA]), and LuxaGlaze was applied and light cured (Figures 13 and 14) prior to cementation (Temp-Bond NE [Kerr]).
The restoration will be loosened prior to visits with the surgeon to provide surgical access as needed. The next step will be extraction and grafting of the sites in the teeth Nos. 3, 5, 12, and 14 positions and partial extraction therapy and implant placement in the teeth Nos. 6 and 11 positions. As the extraction sites transition to pontic sites, LuxaCrown will be used to fill the pontics and develop the tissue contours. The intaglio surfaces of the provisional restoration will be cleaned using particle abrasion, etched with phosphoric acid for 20 seconds, filled with LuxaCrown, seated, allowed to cure, and then shaped and polished. The fixed provisional will continue to serve the patient until the implants are integrated and an implant-supported provisional bridge is placed in service.
DISCUSSION
While flexural strength and fracture toughness are important qualities for the success of long-term provisional restorations, numerous factors must be taken into consideration when selecting a material, mode of fabrication, and luting agent. Marginal seal is important to prevent recurrent decay and any dislodgement of the provisional restorations. No matter the luting agent used, principles of retention and resistance form in prep design must be followed to optimize results. Additionally, a cement appropriate for the situation must be selected and used with care. Cements specifically designed for short-term provisionalization can be incorporated, even with a provisional that will be used long term, if there is a need for retrievability at various intervals (eg, TempoCem [DMG America], Temp-Bond [Kerr], CLING2, etc). Long-term provisional restorations that will stay in place for several years are best secured using a cement that provides antimicrobial properties, such as zinc phosphate,8 or one that provides an improved marginal seal, such as self-etching resin cements.
The design of a long-term provisional restoration, like with all provisional restorations, must provide access for oral hygiene. The material must be strong enough in thin applications to allow acceptable marginal integrity. The material must be wear-resistant and stain-resistant. Aesthetics of the material are also a consideration.
The LuxaCrown material has several of the qualities needed for long-term provisional applications. The material comes in 8 shades to meet a variety of aesthetic demands, though a bleach shade would be a welcome addition to the shade offerings. The material was easy to handle, with only minimal voids—even in large-span applications. These voids were easily filled with a flowable composite designed specifically to work with the material, although it is hypothesized that most flowable composites would serve the need. The material carved similarly to other bisacryl materials, with perhaps the need to apply a bit more pressure, most likely due to the higher filler content.
It will be interesting to see how the material holds up in thinner applications. With the advent of stronger monolithic porcelains (such as lithium disilicate and various zirconia formulations and other newer hybrid ceramics), there is a need for less clearance and tooth reduction, both in the occlusal and axial dimensions. A stronger provisional material has the potential to fill a need for even short-term provisional applications where there is a minimal tooth reduction and clearance.
CLOSING COMMENTS
There will always be a need for long-term provisional restorations. Staging treatment to accommodate financial constraints or healing times is only one indication. The chairside fabrication of provisional restorations has the advantages of efficiency and economy over indirect fabrications. Newer materials, such as LuxaCrown, are designed and manufactured to fill a need for materials that can be fabricated chairside and yet have excellent fracture toughness, flexural strength, and wear resistance. Time will tell if in vitro studies translate to similar in vivo results.
References
- Michalakis K, Pissiotis A, Hirayama H, et al. Comparison of temperature increase in the pulp chamber during the polymerization of materials used for the direct fabrication of provisional restorations. J Prosthet Dent. 2006;96:418-423.
- Tom TN, Uthappa MA, Sunny K, et al. Provisional restorations: an overview of materials used. Journal of Advanced Clinical & Research Insights. 2016;3:212-214.
- Kadiyala KK, Badisa MK, Anne G, et al. Evaluation of flexural strength of thermocycled interim resin materials used in prosthetic rehabilitation—an in-vitro study. J Clin Diagn Res. 2016;10:ZC91-ZC95.
- Hamza TA, Rosenstiel SF, Elhosary MM, et al. The effect of fiber reinforcement on the fracture toughness and flexural strength of provisional restorative resins. J Prosthet Dent. 2004;91:258-264.
- Peñate L, Basilio J, Roig M, et al. Comparative study of interim materials for direct fixed dental prostheses and their fabrication with CAD/CAM technique. J Prosthet Dent. 2015;114:248-253.
- Bluche LR, Bluche PF, Morgano SM. Provisional fixed prosthesis reinforced with a metal casting. J Prosthet Dent. 1997;77:634-635.
- Alt V, Hannig M, Wöstmann B, et al. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater. 2011;27:339-347.
- Daugela P, Oziunas R, Zekonis G. Antibacterial potential of contemporary dental luting cements. Stomatologija. 2008;10:16-21.
Dr. Bakeman maintains a full-time private practice in Grand Rapids, Mich. She is an adjunct faculty member at
the Kois Center in Seattle. Dr. Bakeman is a member of the American Academy of Restorative Dentistry and the American Academy of Esthetic Dentistry and an accredited Fellow of the American Academy of Cosmetic Dentistry (AACD). She currently serves as president-elect for the AACD and is also both the accreditation and Fellowship examiner for the AACD. Dr. Bakeman was the recipient of the AACD’s 2013 Award for Excellence in Cosmetic Dentistry Education. She can be reached at betsy@bakemandds.com.
Disclosure: Dr. Bakeman reports no disclosures.
Related Articles
AACD Launches Cosmetic Dentistry Residency Program
Provisionalization for Implant Dentistry
Aesthetic Success in the Anterior Region: Immediate Placement and Temporization


