INTRODUCTION
Full-arch, implant-supported restorations have become an essential treatment option for patients who wish to have a fixed prosthetic replacement.1-3 Technological advances enable clinicians to provide implant-supported restorations via comprehensive, 3D planned guided surgery protocols for immediate loading and delivery of transitional prostheses on the same day.4-7 The ability to link restorative planning with the surgical placement of dental implants has been made possible with a combination of software applications and improved hardware components for both the surgical and restorative phases of implant reconstruction. Many of these concepts were previously presented by the authors in 2 recent articles that appeared in Dentistry Today.8,9 Guided dental implant surgery provides excellent and consistent accuracy for implant placement within the desired receptor sites while controlling trajectory, depth, and rotational timing. The challenge has been to first plan with the simulated virtual restoration in mind, followed by the prefabricated transitional restoration, which can be delivered to the patient on the day of surgery or soon after with precision and ease.
In the past, a denture conversion was used to connect the prosthetic to the implants using titanium sleeves and screws that either attached directly to the implants or via intermediate abutments. Managing the denture position at the time of surgery—usually with a silicone bite registration—was often a time-consuming and difficult task. The process required large cutouts through the acrylic of the denture for which the titanium sleeves would protrude and where cold-cure acrylic was then injected to surround the sleeves to stabilize them within the prosthesis. This process, although successfully completed thousands of times, involves many points of inaccuracy with bite registrations and ideal prosthetic hole placement. The use of interchangeable, or “stackable,” surgical guides helped to obviate the difficulties with denture conversion, providing a stable foundation for prosthesis orientation and pickup with dual-cure resin. One area that has largely remained the same has been the size of the holes within the prosthesis to overcome the protruding titanium sleeves through the prosthesis. The transitional prosthesis was often thick and bulky to accommodate large holes and could interfere with tongue space, speech, and larger-sized access holes, resulting in improper occlusion.
Regardless of the fabrication process or the material utilized, when a solid prosthesis is subjected to subtractive drilling, the structure is weakened, leading to potential chipping and/or fracture, which could place the implants at risk if not immediately addressed. This article will introduce an innovative product called C2F (Conversion to Final) Small Access Hole Technology, which can help clinicians achieve an improved fit, a higher strength, and preserved occlusion through an extraoral conversion of the transitional prosthesis (CHROME GuidedSMILE [ROE Dental Laboratory]).
The main benefits of small access hole technology are:
- Stronger and narrower prosthetics
- More accurate planning possibilities
- Preserved ideal occlusion
- An extraoral conversion process
- Master casts that are created at surgery appointments can also be used for final prostheses
- Extraoral equilibration for highly accurate bites on every case
CASE REPORT
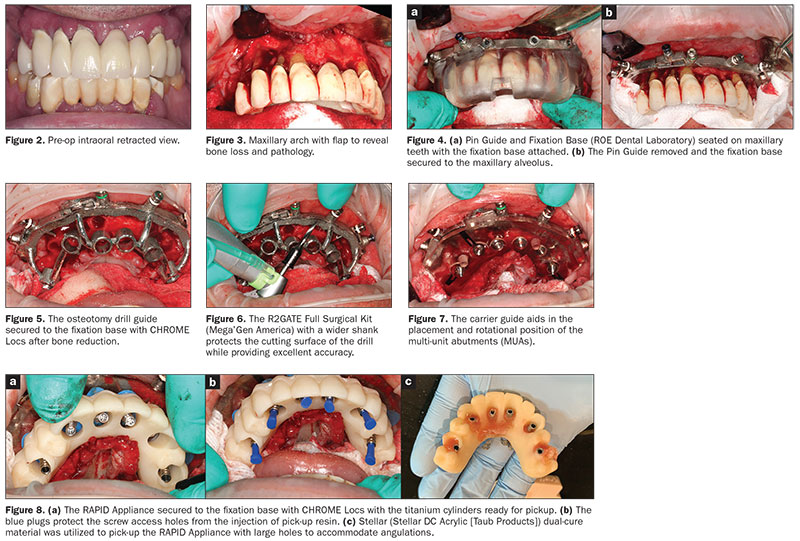
A 58-year-old male presented with failing dentition in both the maxillary and mandibular arches. The pre-existing maxillary fixed ceramo-metal restoration and areas of significant bone loss and pathology can be visualized in both arches on the panoramic reconstructed view taken from the CBCT scan (CS 9600 [Carestream Dental]) (Figure 1). The intraoral retracted photo revealed poor oral hygiene as well as swollen and edematous gingival tissue (Figure 2). The procedures were reviewed with the patient, and after hygiene visits, the patient was ready to receive a dual-arch reconstruction using the CHROME GuidedSMILE (patent-pending) methodology.
 |
| Figure 1. Preoperative panoramic radiograph revealing failing dentition. |
As per the procedures described in our 2019 Dentistry Today article,8 all implants were carefully planned with interactive treatment planning software (BlueSkyPlan [BlueSkyBio]) to determine appropriate implant receptor sites for immediate extraction, immediate placement, and immediate loading. Six implants were planned for the maxilla and 5 for the mandible. The patient was taken to the operatory and sedated for the long surgical intervention. A full-thickness mucoperiosteal flap was elevated to expose the alveolus and areas of significant pathology (Figure 3). To facilitate the positioning of the surgical guides, the Pin Guide and Fixation Base (ROE Dental Laboratory) were then delivered over the existing dentition (Figure 4a). The fixation base was then secured to the facial alveolus by drilling through the metal guide cylinder and placing 4 anchor pins (Figure 4b). An alveolectomy was completed based upon the CBCT scan plan as guided by the fixation base and carrier guide (not shown). Once the bone level had been verified, the osteotomy drill guide was then secured to the fixation base with CHROME Locs (Figure 5). Sequential osteotomies were then prepared with wide shank drills to maintain accuracy (R2GATE Full Surgical Kit [Mega’Gen America]) (Figure 6). Six Neodent GM Helix implants (Straumann) were then placed, and ISQ values were recorded as a baseline to track the integration process and determine if immediate loading was warranted. All values were found to be sufficient for loading. The carrier guide was then used to straightly place and correctly orient the angled multi-unit abutments (MUAs), which were torqued to the manufacturer’s tolerance (Figure 7).
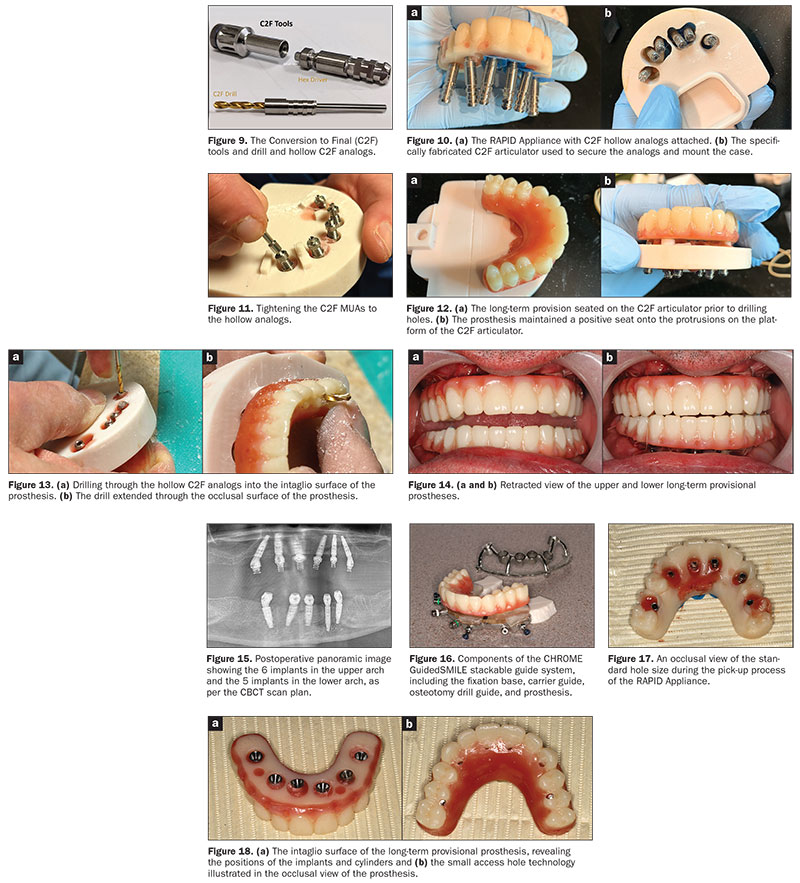
The carrier guide provided a positive interface to link and then secure the MUAs to the transitional prosthesis with temporary titanium sleeves and screws (Figure 8a). The RAPID appliance is an exact duplicate of the surgical prosthetic. The blue plugs protect the screw-access holes from the injection of pick-up resin (Figure 8b). The printed RAPID appliance serves a variety of strategic purposes, the first being to pick up the location of the implant MUAs at the time of surgery (Figure 8c). This protocol, however, requires a second set of temporary titanium cylinders. The MUAs were protected with special green rubber dam material block-out gaskets, and the access holes were protected with blue block-out plugs to prevent resin infiltration. Each access hole is then injected with a dual-cure resin and allowed to cure until fully set (STELLAR DC Acrylic [TAUB Products]). With the C2F workflow and specially fabricated tools and hollow analogs (Figure 9), the RAPID appliance then transfers these positions to a C2F articulator. The analogs are attached to the titanium cylinders (Figure 10a) and then delivered to the C2F articulator for mounting (Figure 10b). To facilitate the small access hole technology, specially designed MUAs are attached to the hollow analogs as seen in Figure 11.
The articulator has similar resin extrusions that provide a positive seat for the Lucitone long-term provisional prosthesis (Dentsply Sirona) (Figure 12). Note that there are no holes in the prosthesis at the time of mounting to the C2F articulator. The innovative design allowed for the holes to be drilled through the hollow C2F analogs from the base of the articulator until the occlusal surface was breached (Figure 13). The C2F articulator then allows for extraoral bite adjustment, so when the
prosthesis is delivered to the patient, the occlusion should already be equilibrated. The long-term surgical provisional upper and lower prostheses were delivered to the patient (Figure 14). The postoperative panoramic radiograph can be seen in Figure 15.
DISCUSSION
Full-arch, implant-supported reconstruction is a proven treatment alternative for patients with terminal dentitions or those who are already in an edentulous state. As each patient’s anatomical presentation is unique and different, a thorough preoperative 3D evaluation is required to understand each case’s pre-existing bone and soft-tissue conditions. Planning for guided surgery treatment modalities allows for a total appreciation of the patient’s occlusion and the desired functional and aesthetic outcome. The dilemma, however, has often been how to relate the prosthetics to the planned position of the implants at the time of surgery for immediate loading protocols. This problem has been resolved with advances in diagnostic imaging and software applications that can position implants based on the restorative outcomes accomplished with current digital workflows.
 |
With the original CHROME GuidedSMILE stackable guide system, the long-term prosthetic was picked up from the carrier guide directly in the mouth at the time of surgery (Figure 16). This required large openings in the prosthetic to accommodate the temporary titanium sleeve positions. The loss of material inherently weakened the resulting patched prosthesis, with large rings of material left to surround the titanium sleeves. In addition, if there were bite discrepancies, they would require intraoral equilibration. The innovative C2F concept obviates these issues, with the caveat that there are extra steps and extra components required for the process to be successful.
The incorporation of small-diameter access holes established from the initial software planning results in the fabrication of narrower prosthetics by positioning the access hole more accurately within the buccal-lingual dimension of the prosthetic design, which helps to maintain structural integrity. Large access holes often will result in wider prosthetics in all dimensions. Additionally, larger access holes require far more “pick-up” material to fill the spaces. The original design specifications for CHROME GuidedSMILE called for 7-mm-diameter access holes to allow for the divergence of titanium sleeves during the pick-up process. Therefore, 6 implants, incorporating 6 holes that are 7 mm in diameter, could result in approximately 280 mm2 of lost occlusal space. Small access holes also help to preserve ideal tooth morphology and occlusal anatomy. The RAPID Appliance pickup for the maxillary arch can be seen in Figure 17. Note the size of the holes and the amount of material utilized. Compare this with the C2F fabricated maxillary prosthesis with small access holes (Figure 18).
Utilizing the RAPID appliance, the C2F protocol provides a more accurate extraoral conversion of the long-term immediate-load prosthetic. With the RAPID appliance seated, the registration is completed on the carrier guide. The bite is then transferred to the C2F articulator, and any discrepancies are adjusted on the articulator and not in the mouth, leading to next to zero adjustments intraorally.
The RAPID appliance (the duplicate prosthetic) is “picked up” intraorally during the surgery using large holes and transferred to a specially designed model and articulator. Once removed from the mouth, the laboratory technician can convert the long-term prosthetic using the C2F protocol while the surgical procedure continues with grafting, tissue approximation, and final suturing. The physical model will then be utilized to fabricate the definitive monolithic zirconia prosthesis once hard- and soft-tissue healing has fully matured.
 |
CONCLUSION
Full-arch dental implant reconstruction is constantly evolving as new and innovative techniques are developed to improve the workflow, efficiency, and accuracy of the process. This includes both the surgical and restorative phases. This article reviewed an innovative protocol to aid in the fabrication of long-term provisional prostheses that results in several important improvements. The benefits of small access hole technology include, but are not limited to, stronger and narrower prosthetic designs; enhanced, restoratively driven planning capabilities; preservation of the occlusion; an extraoral conversion process; master casts created from surgery that can also be used for final definitive prostheses; and extraoral equilibration for near-perfect bites on every case. Disadvantages include the need for extra components over other methods; an increase in luting material use; a moderate cost increase; and, perhaps, additional time needed for the conversion with the specially designed, new protocol. The C2F concept is still being fully developed and evaluated, and as more cases are completed, additional modifications may be forthcoming.
Acknowledgments:
The authors wish to thank Shahab Kokabiyan, for his expert assistance with the onsite C2F conversion process, and Alan Banks of ROE Dental Laboratory.
References
- Morton D, Gallucci G, Lin WS et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:215-223.
- Barootchi S, Askar H, Ravidà A, et al. Long-term Clinical Outcomes and Cost-Effectiveness of Full-Arch Implant-Supported Zirconia-Based and Metal-Acrylic Fixed Dental Prostheses: A Retrospective Analysis. Int J Oral Maxillofac Implants. 2020; Mar/Apr;35(2):395-405. doi: 10.11607/jomi.7833. PMID: 32142577.
- Gallardo YNR, da Silva-Olivio IR, Gonzaga L, et al. A Systematic Review of Clinical Outcomes on Patients Rehabilitated with Complete-Arch Fixed Implant-Supported Prostheses According to the Time of Loading. J Prosthodont. 2019 Dec;28(9):958-968. doi: 10.1111/jopr.13104. Epub 2019 Oct 18. PMID: 31433096.
- Pikos MA, Magyar CW, Llop DR. Guided full-arch immediate-function treatment modality for the edentulous and terminal dentition patient. Compend Contin Educ Dent. 2015 Feb;36(2):116, 119-26, 128.
- Lerner H, Hauschild U, Sader R, et al. Complete-arch fixed reconstruction by means of guided surgery and immediate loading: a retrospective clinical study on 12 patients with 1 year of follow-up. BMC Oral Health. 2020 Jan 16;20(1):15. doi: 10.1186/s12903-019-0941-z. PMID: 31948414; PMCID: PMC6966809.
- Luongo, G, Ciabattoni G, Acocella D. Digital Implantology (2018). Milan, Italy: Quintessenza Edizioni SRL.
- Testori T, Robiony M, Parenti A, et al. Evaluation of accuracy and precision of a new guided surgery system: a multicenter clinical study. Int J Periodontics Restorative Dent. 2014;34 Suppl 3:s59-69. doi: 10.11607/prd.1279. PMID: 24956092.
- Ganz, SD, Tawil I. Full-Arch Implant Surgical and Restorative Considerations: Utilizing a Full Template Guidance Technique. Dent Today. 2019;38(9):72-78.
- Ganz, SD, Tawil I. Full-Arch Implant Surgical and Restorative Considerations: Innovative Digital Workflow Using a Verification Jig With
Teeth. Dent Today. 2020;39(1):70-76
Dr. Ganz received his dental degree from University of Medicine and Dentistry — NJ Dental School and a specialty certificate in maxillofacial prosthetics/prosthodontics at the MD Anderson Cancer Institute in Houston. He is a Fellow of the Academy of Osseointegration, a Fellow of the International College of Dentists, a Diplomate of the International Congress of Oral Implantologists (ICOI), US Ambassador of the Digital Dental Society, and co-director of Advanced Implant Education (AIE). Dr. Ganz was recently honored by the American Academy of Implant Dentistry and the Digital Dentistry Society for his lifelong contributions. He is on the faculty of the Rutgers School of Dental Medicine, is the director of oral restoration at Park40 in New York City, and maintains a private practice in Fort Lee, NJ. He can be reached at drganz@drganz.com.
Dr. Tawil received his DDS degree from the New York University College of Dentistry and his Master of Biological Sciences degree from Long Island University. He is co-director of AIE. He is a Diplomate of the International Academy of Dental Implantology as well as a Fellow of the ICOI and the Advanced Implant Academy. He has received recognition for outstanding achievement in dental implants from the Advanced Implant Academy and has received the President’s Service Award for his volunteer work. Dr. Tawil lectures internationally on advanced dental implant procedures. He maintains a general private practice in Brooklyn, NY, where he focuses on implant therapy. He can be reached at tawildental@gmail.com.
Disclosure: Dr. Ganz recieves lecture honoraria for lectures from ROE Dental Laboratory, Osstell, and Carestream Dental. Dr. Tawil reports no disclosures.
Related Articles
Digital Technologies: A Roundtable Discussion on Changing the Face of Dentistry
Guided Applications for Partial Extraction Therapy



