Despite the remarkable progress of vaccination in the United States and other countries such as the United Kingdom, the COVID-19 pandemic is unfortunately far from over. The catastrophic situation in India and Brazil highlights the tragic consequences of the sidelining of science.
Meanwhile, healthcare professionals still face several challenges given the threat of new variants, the lack of biomarkers to identify those at risk for severe complications and death, the lack of predictable treatment, and the scarcity of knowledge on the duration of the immunity conferred by the vaccines. It has become clear that hidden sources of infection may play a crucial role in the pathogenesis of severe COVID-19.
The Role of Oral Health
Last year, after reading about the importance of inflammatory markers in the progression of COVID-19 lung disease, particularly IL-6, my research partner Carla Cruvinel Pontes, DDS, MsC, PhD, and I wrote an article suggesting a link between periodontal disease and its potential to contribute to elevated local and systemic IL-6 levels.
Since then, our findings have been corroborated by clinical studies suggesting high IL-6 levels to be a strong predictor of severe acute respiratory syndrome in COVID-19 patients and periodontitis to be a risk factor for complications. Notably, the study from Marouf et al. (2021) showed that periodontitis resulted in 8.8 times higher risk for death, 4.6 times higher risk for needing mechanical ventilation, and 3.5 times higher risk for ICU admission after accounting for significant confounders, such as age, comorbidities, and smoking.
At the beginning of 2021, I was contacted by an experienced radiologist and medical educator from the UK, Dr. Graham Lloyd-Jones. He had also been in contact with a professor from Birmingham and former president of the European Academy of Periodontology, Iain Chapple. Together, Dr. Cruvinel Pontes, Dr. Lloyd-Jones, Prof. Chapple, and I decided to expand our understanding of the role that oral health, particularly periodontitis, can play in the pandemic.
Our collaboration resulted in the development of a solid medical hypothesis, recently published in the Journal of Oral Medicine and Dental Research, which has been in the spotlight on more than 200 websites worldwide, live radio, and TV. Here, we explain the reasons behind the vast public interest in our study and why it has the potential to change the course of the pandemic.
When a Hypothesis Is More Than a Concept
Many hypotheses are born from scientific exploration. It is crucial to mention that our hypothesis study was born from radiologic lung image findings from COVID-19 patients, and not simply from scientific curiosity. Simply put, Dr. Lloyd-Jones noticed that the disease pattern seen radiographically in COVID-19 lung disease did not match other viral lung infections.
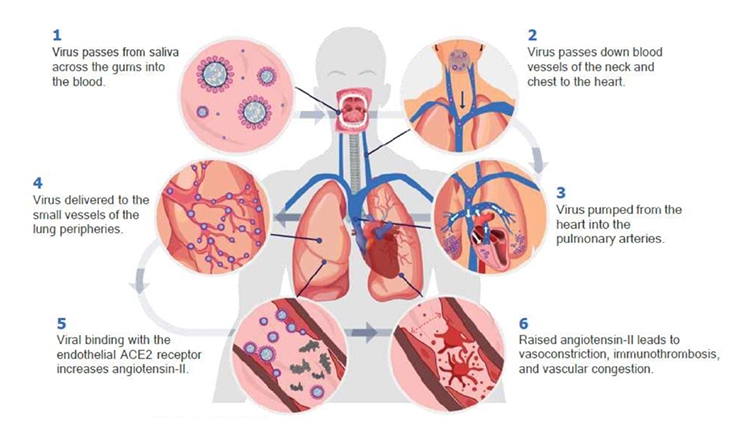
COVID-19 lung disease develops in the base of the lung, as opposed to the mid- and upper areas, as typically seen with infections caused by inhaled pathogens. Vascular changes in small lung vessels are evident early in the disease process in computed tomography (CT) images, including peripheral vasodilation, immunothrombosis, and small filling defects (clots). Microangiopathy and pulmonary infarcts, characterizing thrombosis on both sides of the capillary bed (in both venules and arterioles), have been confirmed in lung autopsies.
Based on the radiological findings, COVID-19 initial lung disease seems to be vascular in nature, as opposed to a primary disease of the trachea and airways. But how does it reach the lung vessels?
With the knowledge that saliva is a reservoir for the virus and that salivary viral levels are strong predictors of poor outcome and disease severity, as well as findings suggesting that SARS-CoV-2 does not reach the lungs through inhalation, we propose that the virus enters the blood circulation in the mouth, from where it reaches the lungs.
The oral cavity biological foundation for this model includes:
- Many oral and gingival cells express ACE-2 receptors, including cells from the gingival sulcus.
- SARS-CoV-2 RNA has been found in saliva and gingival crevicular fluid. The virus can invade salivary glands and mucosal and gingival cells.
- The periodontal environment can favor viral replication and passage through the permeable sulcular or pocket epithelium. Poor oral hygiene, periodontal inflammation, and viral-bacterial synergy can potentially mediate SARS-CoV-2 entrance to the mucosal or gingival blood circulation.
- Higher severity of COVID-19 and risk of death have been linked to periodontitis.
- Other respiratory conditions have been linked to periodontal disease and poor oral hygiene.
COVID-19 and periodontitis have multiple common risk factors, such as aging, specific ethnic groups, male sex, type A blood group, obesity, cardiovascular disease, diabetes, chronic kidney disease, chronic obstructive pulmonary disease, dementia, Down syndrome, learning difficulty, and physical disability (see the figure).
What Does It Mean If This Model Is Correct?
If the hypothesis is proven correct, decreasing the viral load in saliva can mitigate transmission and decrease the risk for lung complications and death. Simple measures can prevent the virus from entering the blood circulation in the oral cavity.
For example, maintenance of optimal daily oral hygiene can fight infection, including toothbrushing twice daily for at least 2 minutes with a fluoridated toothpaste, along with daily interdental cleaning. Periodontitis patients are likely to need longer brushing times.
Also, the use of commercial mouthwash products can inactivate the virus in vitro, whether it’s 15 ml of 0.05% to 0.1% cetylpyridinium chloride (CPC) for 30 seconds twice a day, or 20 ml of 0.147% ethyl lauroyl arginate (ELA) for 30 seconds twice a day. However, daily oral hygiene cannot be replaced by the use of oral rinses.
Regular dental visits are essential to preventing infection as well.
Can Oral Rinses Prevent COVID-19 Lung Disease?
Currently, there is a scarcity of clinical studies on the effect of oral rinses in COVID-19. However, because these over-the-counter products are widely available and have been proven to be safe for unsupervised home use, we suggest the use of CPC and ELA mouthwashes before and after social interactions.
This simple measure can potentially lower the risk for viral entrance to the blood circulation and COVID-19 lung disease while we wait for clinical studies to confirm their efficacy. In places where oral rinses may not be available, studies on pulmonary conditions indicate that even boiled water that has cooled down or a saline solution can be used as an oral rinse to decrease the salivary viral load.
Simple Preventive Measures Can Make a Difference
The reason why health authorities worldwide are not implementing non-invasive, inexpensive, and preventive measures is obscure. In countries such as Brazil and India, the devastating situation has been linked to the overlooking of science. In fact, scientific opinions have been ignored in multiple countries.
As healthcare professionals, we have strong reasons to believe that the mouth plays a crucial role in the pandemic. We urge health authorities and professionals to recommend preventive measures in private and public contexts, especially CPC and ELA oral rinses. Due to their availability, general safety, and potential to decrease COVID-19 lung disease, need for mechanical ventilation, and death, we believe that this recommendation can truly make a difference.
Results from ongoing studies will certainly shed more light on the efficacy of mouthwash products against COVID-19. Meanwhile, let’s do our part and listen to what science is telling us. It strongly suggests that COVID-19 lung complications can start in the mouth, so this is also where preventive measures should begin.
Reference
Lloyd-Jones G, Molayem S, Pontes CC, Chapple I. (2021) The COVID-19 Pathway: A Proposed Oral-Vascular-Pulmonary Route of SARS-CoV-2 Infection and the Importance of Oral Healthcare Measures. J Oral Med and Dent Res. 2(1):1-25.
Dr. Molayem received both his bachelor of arts in history and DDS at UCLA. Thereafter, he completed a specialty program in periodontics at the Herman Ostrow USC School of Dentistry. He is the founder of both the UCLA and USC Journals of Dental Research, which have been going on for 13 and 11 years, respectively. He has lectured and has published in dental implants and periodontics and is the co-founder of Synergy Specialists, the largest agency for traveling dental specialists in the United States. Dr. Molayem has been practicing periodontics in a private practice setting in Southern California for the past 10 years. More recently, he has been conducting research and has published the most comprehensive connection to date between the mouth and COVID-19 in the Journal of the California Dental Association. He can be reached at smolayem@gmail.com.
Related Articles
Delayed Dental Treatment Negates the Mouth-Body Connection
COVID-19 Patients With Periodontitis Face Greater Risk of Dying
Today’s Dental Practices Need On-Point Messaging to Improve Oral and Systemic Health



