The impact of a smile often has untold ramifications on a patient. A new smile can often be the catalyst to spark a change in a person’s brain chemistry and mindset to put them on a new path in life. A smile being altered can create a chain reaction of events, starting from happiness and excitement, that releases endorphins, serotonin, dopamine, and oxytocin in the brain. This chemical release can be the needed stimuli to reduce cortisol levels in the brain, allowing someone to be happier and more confident, potentially creating a new path and different opportunities over the rest of his or her life.
When the body is stressed, the hormone cortisol is released into the bloodstream. Although certain amounts of cortisol are healthy, it is a contributor to depression.1 Many people live with the daily mental challenges that play on the mind because of being stressed or unhappy. Psychological doubt and stress hinder a person’s brain chemistry, defeating them so that they will not work as hard and push forward through adversity. Brain chemistry and chronic external stressors are all contributing factors in the etiology of depression. Not having an attractive smile and not being happy with oneself in the form of one’s confidence and capabilities can create a constant stress and negativity.
The following clinical case report will clearly demonstrate the positive impact that improving the aesthetics and function of a smile can have on one’s life.
CASE REPORT
Diagnosis and Treatment Planning
A 53-year-old male, who was slightly overweight and not sleeping well, presented with an extremely worn dentition. He had missing, worn, and discolored teeth. He wanted to be able to chew food again and bite into food with his front teeth. He did not like to smile and had a beard to hide his teeth, and he would often look down when talking. His persona in how he showed up was weak, defeated, self-conscious, ashamed, frustrated, and worn out. He noted that he had a problem with getting a good night’s rest and of being tired during the day. Adding further to his psychological state, he had also been diagnosed with and was fighting cancer, but he was in remission at the time of this visit.
We started by having a discussion with the patient about his present condition first and then his future goals; the gap between the 2 is challenging as most patients are not inclined to make themselves uncomfortable until the pain of staying the same is higher than the pain that change requires. Real roadblocks, such as finding the money required for treatment, need to be addressed. A patient’s unrealized subconscious and self-imposed roadblocks must be dealt with as well. Strategic questions were asked to help the patient come to his own conclusion. We discussed his needs and desires by creating an honest and open conversation that also kept him focused on the objective at hand. It was obvious that this patient needed a full-mouth rehabilitation, and, thankfully, the patient arrived at the same conclusion.
 |
We then took photos and showed him one potential new appearance using digital simulation software (PreVu). Upon seeing the imagery of what could be created, the patient altered his existing thought process. The excitement in being able to see a new alternate reality opens the mind to the possibilities available. This visualization process helps patients feel good because solutions are presented that will help them.
Next, photos, followed by upper and lower impressions, were taken using an accurate and dimensionally stable vinyl polysiloxane (VPS) alginate substitute material (CounterFit [Clinician’s Choice Dental Products]). Once set, this VPS impression material allows multiple models to be poured, if needed going forward. A face-bow transfer was also taken and used to mount the case onto a semi-adjustable articulator (SAM 3 Articulator [Great Lakes Dental Technologies]) (Figures 1 and 2).
Referral to the Sleep Specialist
The patient was referred out for a sleep study to determine if his excess weight, sleep disturbances, and daytime tiredness were caused by sleep apnea. The results of the study revealed that he did have sleep apnea. A CPAP machine was prescribed for him, and once he started to use it, he was immediately sleeping better and feeling better. He stated that he had more energy in the mornings as well as throughout the day.2
Final Pre-Restorative Phase
A superior repositioning appliance (SRA) was prescribed and then sent to the dental laboratory team for fabrication. The SRA assists the clinician in making a more accurate evaluation of the jaw position. An anterior ramp to create canine disclusion and anterior protrusive guidance would only be present on the lower 4 incisors. The posterior teeth would have point contacts on a flat plane surface. The appliance would be relined every 2 to 3 weeks on the occlusal surface to allow for jaw position changes that would occur. Due to the lack of teeth interdigitating, the jaw was no longer inhibited to maintain the existing CO. The jaw could now move to a more homeostatic position where muscles that were stretched, and the muscles that were overactive in positioning the jaw, could relax.
After 3 relines of the occlusal surface, the jaw position appeared to be stable with no visible slide being perceived. A hinge axis recording (SAM 3 Articulator) was done to determine if, in fact, a stable and repeatable jaw position had been achieved. Two upper diagnostic models were mounted to the articulator: one with a split cast and the other without. The wax bites were used to mount the mandibular model to the articulator. Wax bite registrations had also been taken at 3 different thicknesses and were used to verify the mount of the patient’s upper cast. Based on his jaw and tooth positions, as well as tooth loss from wear, the incisal pin was opened to create the space necessary to re-create ideal-length anterior teeth that would then properly couple and contact. A second mandibular model was mounted to the articulator so that there were 2 sets of mounted models: One set could be maintained as a record, and, on the other set, the teeth could be altered during the diagnostic wax-up.3 Next, the case was sent to the dental lab team to have a diagnostic wax-up done for all the teeth as well as missing teeth Nos. 13, 14, and 15.
Following the return of the completed diagnostic wax-up, a duplicated stone model was used to create a beadline over-impression4 with Template VPS material (Clinician’s Choice Dental Products) to make provisional restorations on the same day as the crown preparations (Figures 3 and 4).
The patient was then sent to the periodontist to evaluate position Nos. 13 to 15 for the placement of 3 dental implants. Radiographic stents were created to evaluate implant positions and bone access via a CBCT radiograph.
Crown Preparations
The next week, the patient presented back to our office for conventional crown preparations done under general IV sedation along with local anesthetic. Teeth that had existing crowns were sectioned off and removed, while existing direct restorations were removed and replaced using a conventional glass ionomer restorative material (EQUIA Forte [GC America]). Crown preparations were complete
d on all the upper teeth (Figure 5), and then a bite registration was taken to mount the upper cast. Next, the lower teeth were prepared, and then a bite registration was taken that would be used to mount the lower cast. Shade photos were taken of the prepared teeth to allow the ceramist to see the colors of the prepared teeth (Figure 6). A #00 woven retraction cord (Ultrapak [Ultradent Products]) was then placed (with no hemostatic solutions). Impressions were then taken utilizing a VPS impression material (Thermo Clone [Ultradent Products]) and thermoplastic impression trays (Heatwave [Clinician’s Choice Dental Products]) (Figures 7 and 8). The maxillary beadline over-impression was then filled with B1-shade bis-acryl provisional material (Inspire [Clinician’s Choice Dental Products]), then placed with pressure over the upper teeth and held in place for one minute longer than the manufacturer-recommended set time. This allowed the material to fully harden and shrink to completion before removing the beadline over-impression to reveal the new provisionals. The lower beadline over-impression was then filled with the same material, held in place until set, and then removed. A few small adjustments were made to the occlusion of the beadline provisional restorations before the patient was awake and dismissed (Figure 9). The patient was immediately delighted to see his larger and more aesthetic teeth.
The models were poured and mounted on the articulator (Figures 10 and 11). To achieve both great aesthetics and high strength, the master ceramist Hiroaki Tada of Ultimate Styles in Irvine, Calif, created the restorations using a high translucency (HT) zirconia (Noritake). Each of the anterior crowns were made using a facial cutback technique, and feldspathic veneering porcelain was added over the cutback areas for maximal aesthetics, all supported by the strong zirconia substructure. The posterior crowns were mostly monolithic other than some small areas of facial layering porcelain having been added in the aesthetic zone (Figures 12 to 14).
The patient returned 3 weeks later for delivery of the restorations. The provisionals were removed, and the teeth were cleaned and rinsed. The restorations were tried in using a water-soluble try-in paste (Try-In Paste [BISCO Dental Products]), and the margins, contacts, occlusion, and color were evaluated. After the patient saw and approved the aesthetics, the restorations were removed from the mouth and then rinsed. The restorations were delivered in segments of 4 to 6 crowns at a time using a bioactive cement (Ceramir [Doxa Dental]).5 After holding a segment in place for 3 minutes, all excess cement was removed, and the contacts were flossed. Then the next segment was cemented in the same manner until all the restorations had been cemented. Subsequently, the occlusion was checked, and a couple of spot adjustments were made. The beautiful restorations can be seen in Figures 15 and 16. The patient was very pleased with the results thus far.
 |
Implants, Restorations, and a Nightguard
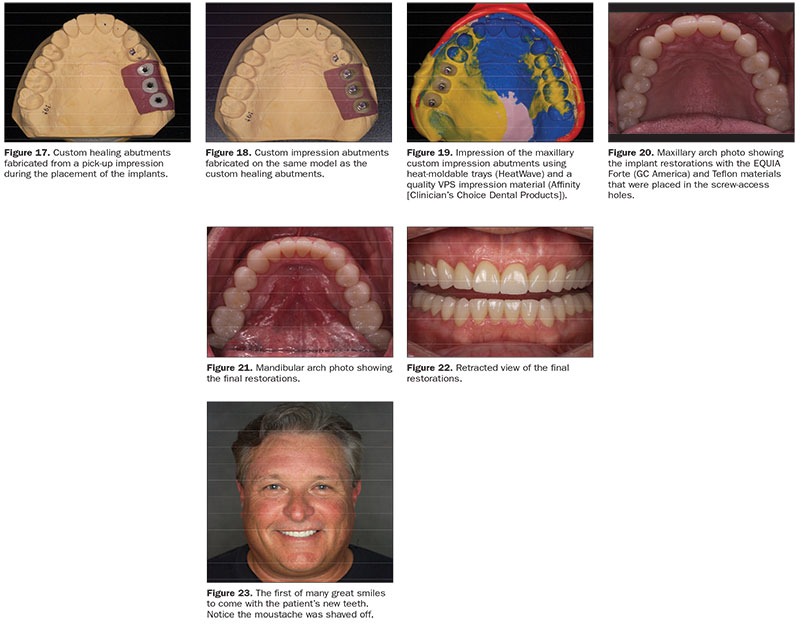
Next, the patient had implants placed by a periodontist, and they were allowed to heal for a few months. The implants were uncovered, and custom healing abutments were placed to allow for tissue conditioning to achieve the desired contour and health over a period of weeks. Next, custom implant impression analogs that mirrored the same shape as the custom healing abutments were used to capture the position of the implants in relation to the teeth and gums (Figures 17 and 18). An extra-light impression material and a heavy-body tray material (Affinity [Clinician’s Choice Dental Products]) were used in a HeatWave thermoplastic impression tray that had been lined with adhesive. The material easily captured the teeth and implant impression analogs (Figure 19). A centric occlusion bite was taken at this time since the implants would be intentionally built slightly out of occlusion due to not having periodontal ligaments. Excursive movements would be dictated by the canine guidance such that no posterior interferences would be introduced. The implant crowns were screw-retained and torqued to 35 Ncm, followed by the use of Teflon tape to cover the screw heads. A conventional glass ionomer (EQUIA Forte) was used to fill in the screw access channels in the crowns, followed by adjustment with a fine diamond underwater spray.
Impressions were taken to fabricate a new nightguard to be worn at night when also wearing the CPAP to protect the new restorations from damage. Then, one week later, the nightguard was delivered, and postoperative photos were taken (Figures 21 and 22).
CLOSING COMMENTS
The Impact of Dental Treatment on a Patient’s Life
The patient returned for a 4-month post-op checkup and cleaning. At that time, he felt much better, had lost weight, was sleeping better, and could bite through food with his front teeth. The whole dental team noticed a drastic difference in him, both mentally and physically. He talked about how he was not as grumpy and tired. He had even shaved off his moustache that he had maintained for years to help hide his teeth and smile. He was more inclined to have conversations and stated that he was happier and more friendly with coworkers and family members. He noticed that he now received the same energy and happiness mirrored back to him by others. His home life had improved, and he had become financially more successful since altering his smile and using the CPAP for sleep apnea (Figure 23).
References
- Davidson RJ, Pizzagalli D, Nitschke JB, et al. Depression: perspectives from affective neuroscience. Annu Rev Psychol. 2002;53:545-574.
- Batool-Anwar S, Goodwin JL, Kushida CA, et al. Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA). J Sleep Res. 2016;25:731-738.
- Snyder TC. Complex cosmetics and occlusion: an interdisciplinary approach. Dent Today. 2019;38:98-101.
- Snyder TC. Beadline provisionals. Pract Proced Aesthet Dent. 2009;21:E1-E7.
- Jefferies SR, Pameijer CH, Appleby DC, et al. A bioactive dental luting cement—its retentive properties and 3-year clinical findings. Compend Contin Educ Dent. 2013;34(special issue 1):2-9.
Dr. Snyder received his doctorate in dental surgery at the University of California, Los Angeles (UCLA) School of Dentistry and has trained at the F.A.C.E. institute. He is an Accredited Fellow of the American Academy of Cosmetic Dentistry and is a member of Catapult Education. Dr. Snyder was on the faculty at UCLA, where he created and co-directed the first 2-year graduate program in aesthetic and cosmetic restorative dentistry. In addition to lecturing internationally, he has co-authored 3 books and written numerous articles in publications around the world. He is the owner of Aesthetic Dental Designs in Laguna Niguel, Calif, and also has an online dental education program at legionpride.com. He can be reached at drtoddsnyder.com.
Disclosure: The author reports no disclosures.
Related Articles
Exceptional Direct Restorations: New Diagnostics, Composite Materials, and Sectional Rings
Easier and Faster Aesthetic Bonding: The Keys to Success
Modern Composites for Minimally Invasive Cosmetics


