The Dental AI Council (DAIC) has found vast inconsistencies in diagnosis and treatment planning between dentists.
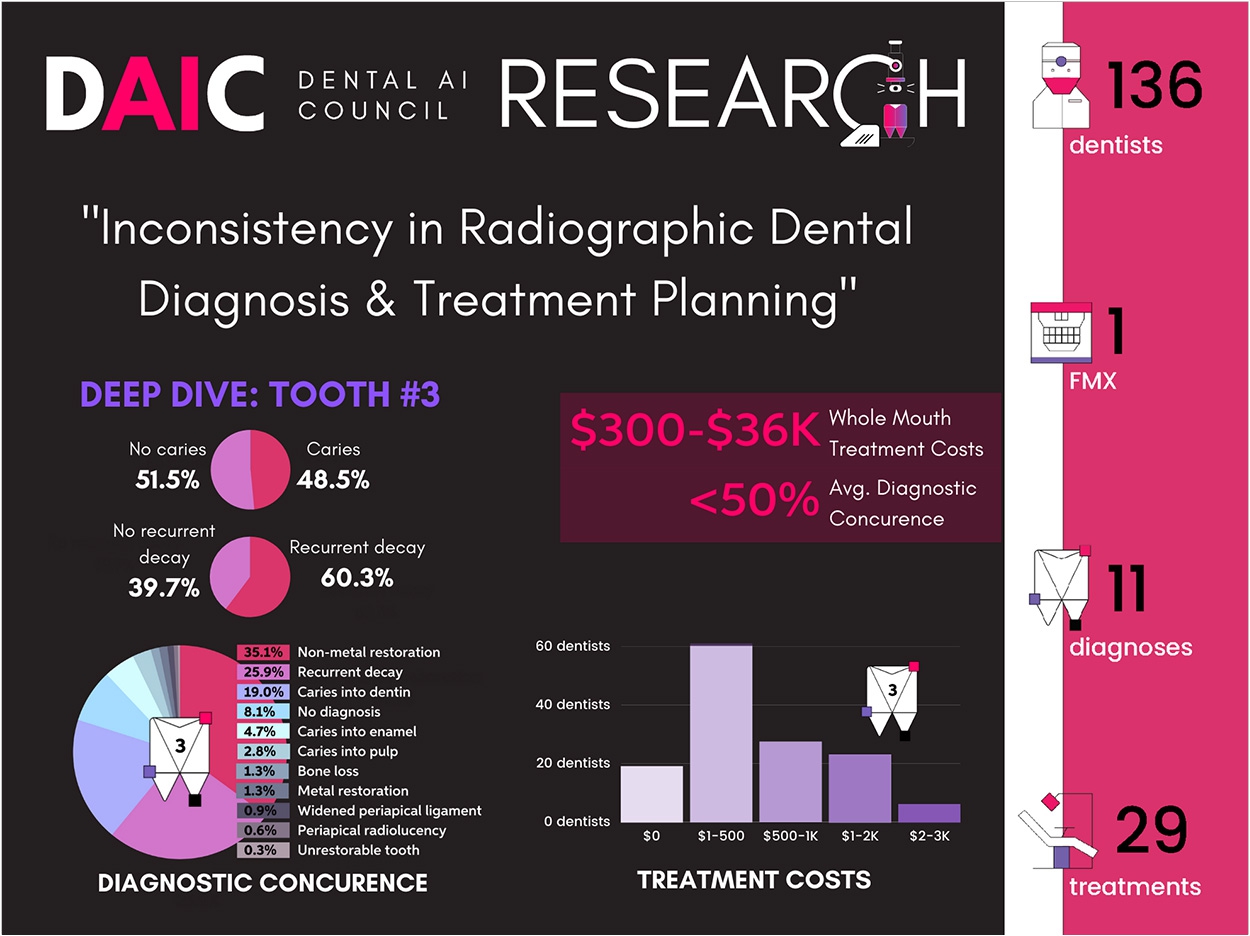
The research spanned 136 licensed practicing dentists across 14 countries who were asked to review and diagnose pathologies presented in a full-mouth radiographic image series.
As the dentists made individual pathology diagnoses, they recommended corresponding standardized-cost treatment plans, allowing the researchers to accurately compare full-mouth treatment plan fees across each participating dentist.
Across study results, diagnoses and treatment plans varied significantly from dentist to dentist. Consensus was infrequent. There were no cases where all of the respondents agreed unanimously upon the existence of tooth decay.
Where dentists agreed on the existence of decay, the determination of its severity, its penetration level, and whether it was recurrent or not varied widely.
The study also found:
- In no instance did more than 81% of respondents concur in a diagnosis.
- The highest levels of agreement occurred in identifying the presence of non-metallic fillings (81%), impacted molars (65%), and recurrent decay (63%).
- Tooth No. 16 was identified by 89 respondents as impacted, but only one respondent outside the United States proposed extracting it, while 51 of 66 US respondents did.
Perhaps most striking among the results, the researchers said, was the variability across whole-mouth treatment costs. For example, the highest-cost whole-mouth treatment plan ($36,000) was 20 times greater than the lowest cost plan (a few hundred dollars). Five dentists determined treatment costs in excess of $18,000.
“There’s been anecdotal inconsistency in diagnosis and treatment planning between dentists, but the scope of the problem is hard to quantify or understand at scale,” said DAIC founding member Ron Bolden, vice president of dental market insight at Cigna.
“Practicing dentists certainly want to make the most accurate diagnosis using all available resources and tools, but broad awareness of how technologies like AI can improve the quality and consistency of care has yet to take root. This study is helpful because anyone who sees the numbers can’t help but want to find ways to be better,” Bolden said.
While it’s reasonable that different dentists would select different treatments for a given condition, the scale of variability is troubling, DAIC said, particularly in light of the fact that treatment inconsistencies have a direct impact on what patients and insurers pay for treatment.
When treatment variability leads to overtreatment of excessive treatment cost, which itself is a common impediment to acceptance of essential treatment among patients, loss of patient trust becomes a concern with significant implications for the oral health of patients and the financial health of the industry, DAIC said.
“For a study tethered to standardized costs to show fee differentials of $30,000 or more is disconcerting,” said Dr. Sanjay Mallya, DAIC founding member and chair of oral and maxillofacial radiology at the UCLA School of Dentistry.
“My hope is that this study will provide a little gut check for the industry and that, as the DAIC rolls out additional research in 2021 and beyond, we’ll bring more evidence like this that inspires efforts to establish more consistent standards of dental care,” Mallya said.
The study, “Inconsistency in Radiographic Dental Diagnostics & Treatment Planning,” is available online.
Related Articles
Dental AI Council Looking for New Members
Dental AI Council to Tackle Future of Artificial Intelligence in Dentistry
Artificial Intelligence Beats Dentists in Tooth Decay Diagnoses












