INTRODUCTION
Matrix techniques are commonly used to transfer the shape and form of a planned new smile from a digital or analogue wax-up model to a patient’s teeth by using some form of stent and a suitable restorative medium, such as composite resin, to allow placement of a definitive restoration. There have been many variations of this technique, and all have inherent limitations and inadequacies. A flowable resin material is often advocated for ease of placement and the idealized property of low viscosity, but this comes at the sacrifice of mechanical strength and wear resistance. Many attempts have been made to improve the matrix transfer technique, but all have fallen short. In 2018, SmileFast launched a new concept in the United Kingdom and have since trained more than one quarter of all practicing UK dentists. This novel stent and application technique, which uses the preferred and superior paste resin composite, has now become commonplace and is the ideal solution for composite smile restorations using a matrix transfer. The following case presentation describes this technique in detail, with both the clinical sequence and the evidence-based rationale discussed.
CASE REPORT
Patient History
The patient was a medically fit 24-year-old female and was deemed a low caries risk with no concerning social habits. Her oral hygiene was good, and she was a regular dental attendee. She had excellent periodontal health, and there were no concerning radiographic findings.
Diagnosis
Her main concern was the size discrepancies and the spacing within her smile, specifically between the dominant central teeth and the microdontic lateral teeth. She was a Class I occlusion with only minimal canine tip tooth surface loss indicative of some tooth grinding, likely during the night. The alignment of her teeth was generally good. However, the upper anterior 4 teeth had slight rotations and lacked symmetry. She had a low lip line and slightly deficient buccal corridors (Figure 1). Her aim was to achieve a brighter, whiter, and more balanced smile.

Treatment Planning
After a full consultation and discussion of initial costs, timeframes, ongoing maintenance, and repair costs, the patient proceeded to explore her options. A full set of clinical photos and an intraoral scan of her dentition was submitted to SmileFast, where a digital mockup for a restorative solution was returned (Figure 2). The SmileFast integrated 3D software allowed her to visualize and understand the proposed options with both a 6-unit and a 10-unit smile makeover setup for discussion. It was explained that by taking the veneers onto the premolars, the smile could be broadened, and the deficient buccal corridors could be filled. The longevity and aesthetics of each type of anterior restoration were explained, with both ceramic and composite options discussed.

A putty trial stent was made on the 3D wax-up model of both the 6-unit and 10-unit mock-up, and the proposed smiles were separately transferred over her teeth using a temporary crown and bridge bis-acryl material. This allowed the patient to visualize both of the different smile enhancement options and ensure she was happy and fully consented on the expected aesthetic result. She decided to restore only the anterior 6 teeth. This visual try-in is essential to stimulate and engage in these conversations with patients to ensure complete understanding and that full consent is attained. In addition to ensuring the patient fully agrees and consents to the planned clinical procedure, the trial appointment also allows the clinician to assess the teeth and smile for balance and function. This better assesses how the restorations will affect the bite and guidance, which allows for more diligent planning and the opportunity for changes ahead of the final planned permanent restorations.
It was decided to enhance the patient’s smile using 6 direct composite veneer restorations, which would better balance the smile by improving the color, size, and proportions of the teeth. This was certainly a very minimally invasive treatment option for such a young patient and carried the most minimal biological risks to the teeth when compared to other, more invasive treatment options, such as ceramic veneers. All occlusal and potential parafunction influences were considered, and as there were no contraindicatory factors, it was deemed that a direct composite veneer approach would be the most favorable for this patient at this time.
Treatment Process
The patient began with a course of home tooth whitening using 10% carbamide peroxide whitening gel worn in trays overnight for 3 weeks. Once whitening is completed, any adhesive dentistry should be delayed by 2 weeks to allow the whitening process and oxidation effect to finish and for full rehydration of the teeth to occur before the patient returns for composite restorations.
Within this time, the SmileFast stent was received with the chosen enamel shade of BLXL IPS Empress Direct composite (Ivoclar Vivadent) (Figure 3). The key feature of this stent, which improves upon all existing techniques, is that it has 0.038-mm metal separators built within the stent itself. This means that when the stent is loaded with composite resin and is placed, the separators slide between the teeth and fully separate them from each other. This prevents the composite from sticking together between the teeth and allows for up to 10 teeth to be fully restored in only one application. Additionally, the stent is made from an inner clear silicone transfer medium encased within a hard acrylic carrier; this allows for excellent dimensional stability and an extremely accurate transfer of shape and texture from the digital wax-up to the natural teeth.
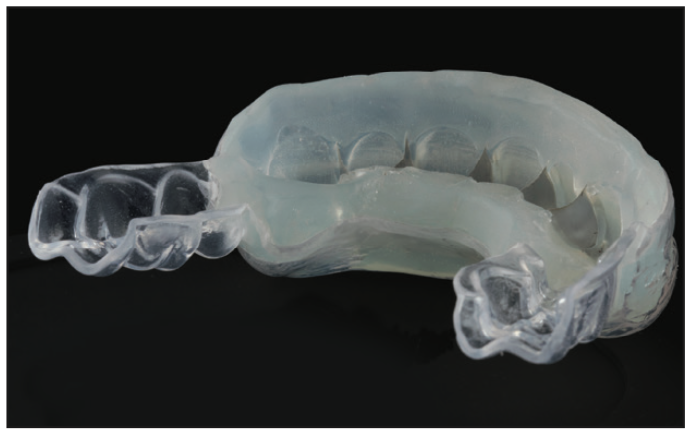
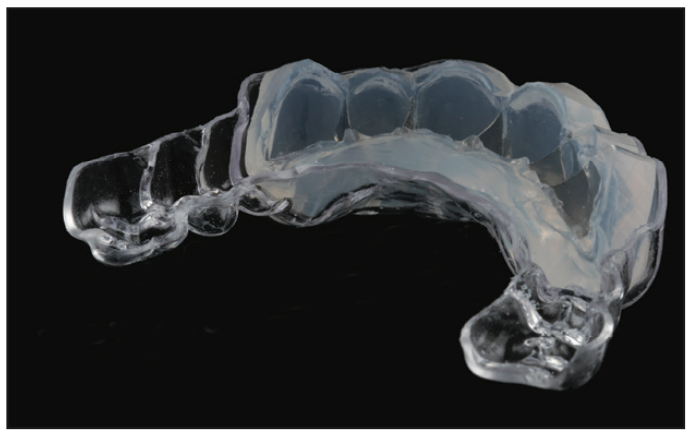
The SmileFast stent presented in this case presentation is of the older generation (Figure 3), with the new generation of stent shown in Figure 4. The enhancement over the previous design is the scalloping around the tooth margins and a thinner volume of silicone transfer medium with a more rigid outer acrylic carrier. This scalloping allows access to the gingival contours of the teeth. Therefore, a much closer and more refined cleanup of any excess composite extruded at the gum margins can be completed before the composite resin is cured. The thinner inner silicone gives enhanced visualization during seating and allows the light-cure unit to be closer to the teeth for enhanced light penetration during curing. Finally, the thicker outer carrier ensures absolute dimensional stability and complete confidence when restoring multiple teeth. The thicker carrier of the stent assists in resisting over-compression during placement. Therefore, the shapes and sizes of the restorations remain precise, both facially as well as in accurately restoring vertical dimensions.
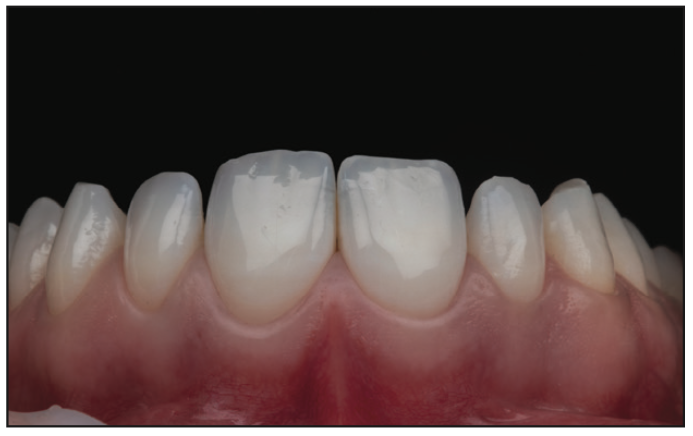
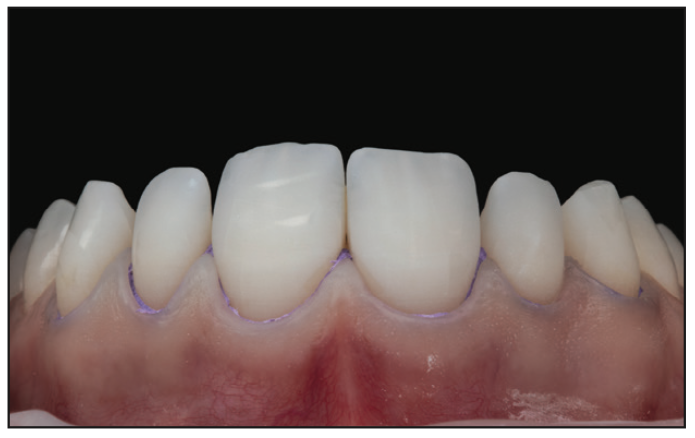
On the day of placement (Figure 5), the stent was tried onto the patient’s teeth to ensure accurate fitting before the teeth were isolated by placing a hydrophobic barrier of PTFE tape down into the sulci from tooth No. 6 to 11 (Figure 6). This acted as a barrier to prevent both gingival crevicular fluid from contaminating the bonding zone and composite from traveling into the sulcus during the composite placement.
The neighboring teeth were protected with a metal matrix strip, and the teeth planned for restoration were microetched using an air abrasion unit with 50 µm aluminium oxide powder to remove biofilm and increase micro-mechanical retention, followed by acid etching (Figure 7) and bonding protocol. A 3-step, fourth-generation adhesive bonding system was chosen as the entire surface to be treated on all teeth was within enamel. This technique first places a separate acid etch on the enamel before it is rinsed off. Then a priming stage is completed, and the primer is allowed to evaporate before the third stage of the adhesive bond placement (Figure 8). A total-etch technique using a fourth-generation system has been shown to offer the highest bond strengths to enamel when the technique is employed carefully and correctly. When there is exposed dentin, a selective-etch technique utilizing a sixth- or seventh-generation bonding system should ideally be used. This does not place a separate etch on the dentin first and utilizes the short-acting and mild acidic component of the self-etching adhesive on the exposed dentin during the priming stage, which creates a thin, hybrid layer. This is less prone to hydrolysis than using a total-etch technique. Additionally, a more stable and durable bonding interface is created as there is only partial demineralization of the dentin and subsequent bonding to the hydroxyapatite crystal that remains.1,2


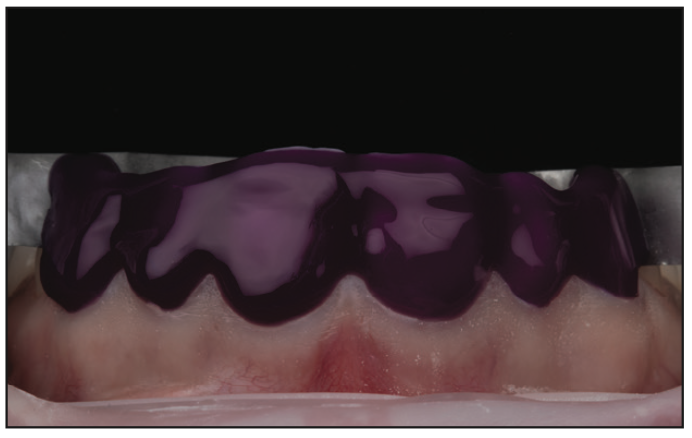
Once tried in, the SmileFast stent was preloaded with heated paste composite and then placed on a heater to heat the entire stent to 140°F (Figure 9). Heating composite to this temperature is well-researched and shown to significantly improve the mechanical qualities of the material due to higher levels of monomer conversion when curing.3-5 Better strength and wear resistance means that the SmileFast restorations will be more durable, less prone to failure, and maintain their luster for far longer than those made using inferior flowable composite resin techniques.6 Heating the material decreases the viscosity, which then allows it to flow under pressure when the stent is applied to the teeth. The excess material comes out of the palatal-incisal evacuation vents. With the new scalloped-design stent (Figure 4), any excess composite that extrudes gingivally can now be easily cleared away before the restorations are cured through the stent, whereas in the old design, cleaning around tooth margins was impeded (Figure 10).


Upon removal of the stent, the exact replication of the 3D virtual wax-up is perfectly transferred onto the teeth. The teeth are assessed for any voids or repairs before a glycerine gel or similar is placed to seal the composite, and they are given a final cure (Figure 11). Sealing composite is essential as the outer layer of resin is inhibited from fully curing due to the surrounding oxygen.7,8 This leaves a sticky, resinous layer on the outside of all freshly cured composite known as the oxygen-inhibited layer (OIL). If this OIL is not considered and removed before polishing begins, one will find that composite will gather extrinsic stains very quickly and will also lose its luster.
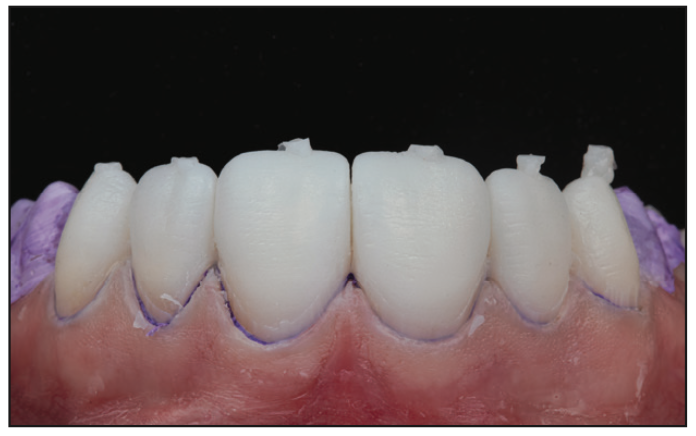
A careful sequence of marginal finishing burs were used to remove any excess composite and refine the margins to ensure a smooth transition from composite veneer to the tooth (this is made significantly easier with the new-generation stent as most of the excess material is removed before light curing). Figure 12 shows the result after stent removal. The primary marginal finishing was then completed before the excess composite material, which extruded through the vents, was removed from the incisal edges. The finishing sequence was then repeated, and interproximal strips were used to smooth the cervical contours before the final occlusal checks and any adjustments were made. Figure 13 shows the bleeding that occured after removal of the PTFE. This was due to an influx of blood into the previously compressed capillaries and did not indicate gingival disease. After final margin refinement, a simple 2-stage polish was completed using diamond-impregnated rubber wheels. In most circumstances, and with experience in the system, a 6-unit restoration case such as this one can be completed in 60 minutes (Figure 14).




The patient returned after 2 weeks, and the composite restorations were given a second enhanced polish using cotton buffs and a 5-µm polishing paste. All margins, occlusion, and excursions were re-checked, and any adjustments were made (Figures 15 and 16). Note the beautiful tooth morphology and the detailed surface texture that was all provided through the SmileFast stent. No shaping or additional texturizing was necessary. Any evidence of occlusal disease or parafunctional habits were addressed and managed with occlusal splint therapy prior to placing the composite restorations. For patients with no signs of previous occlusal disease, a minimum of an Essix retainer is provided.
REFLECTION
Achieving perfect and natural smile aesthetics with composite has always been an incredibly time-consuming and high-skill procedure; however, now with the SmileFast system offering mentor-assisted case selection, patient participation in the design and consent process, and the guided delivery of the restorations using the unique SmileFast stent, dentists can now feel very confident in offering this type of treatment modality to their patients. Providing patients with a planning pathway that shows them all the options and allows them to explore different routes to achieve better smiles is incredibly important. This not only builds trust but also ensures better consent so that their ultimate decisions are based upon a more informed understanding of the techniques, risks, and expected results.


By approaching multiple veneer restorations in the same methodical and planned approach every time, the SmileFast protocol guarantees predictable and consistently excellent aesthetic results. Figure 17 shows the composite veneer makeover as a direct comparison of the final result to the planned digital design; the accuracy of transfer is very precise, with the natural texture and the detailed morphology precisely replicated. For restorations such as these to last well and maintain their luster, the choice of composite material is a critical component as it is essential to have the very best mechanical and aesthetic properties. A nano-hybrid or micro-hybrid paste composite resin is ideal when delivering these smile makeovers that need to be both beautiful and long-lasting.9 This is where the SmileFast technique revolutionizes what has come before by allowing the delivery of up to 10 restorations simultaneously using a direct resin approach and the superior properties of a paste composite.
This patient’s smile is now better balanced, with whiter teeth and more symmetry to the shapes (Figure 18). She was involved in every step of the planning and was able to trial the smile as both a 6-unit and a 10-unit makeover before she decided to proceed. This step is essential to ensure that the patient’s expectations have been met and also to assess the function of the teeth within the smile to test that your planned restorations will not cause interferences or speech changes, etc. The final composite smile will require twice yearly polishing to maintain luster, and the literature supports an expected longevity of 5 to 7 years, with only minimal repair, if necessary, within that timeframe.10-12 For a patient of only 24 years of age, this is a carefully considered and modern approach to smile improvements that minimizes biologic risk to the teeth but also ensures predictability and superior function and aesthetics.
REFERENCES
1. Van Meerbeek B, Yoshihara K, Yoshida Y, et al. State of the art of self-etch adhesives. Dent Mater. 2011;27(1):17-28. doi:10.1016/j.dental.2010.10.023
2. Van Landuyt KL, Yoshida Y, Hirata I, et al. Influence of the chemical structure of functional monomers on their adhesive performance. J Dent Res. 2008;87(8):757–61. doi:10.1177/154405910808700804
3. Daronch M, Rueggeberg FA, De Goes MF. Monomer conversion of pre-heated composite. J Dent Res. 2005;84(7):663–7. doi:10.1177/154405910508400716
4. Wagner WC, Aksu MN, Neme AM, et al. Effect of pre-heating resin composite on restoration microleakage. Oper Dent. 2008;33(1):72–8. doi:10.2341/07-41
5. Calheiros FC, Daronch M, Rueggeberg FA, et al. Effect of temperature on composite polymerization stress and degree of conversion. Dent Mater. 2014;30(6):613–8. doi:10.1016/j.dental.2014.02.024
6. Vajani D, Tejani TH, Milosevic A. Direct composite resin for the management of tooth wear: a systematic review. Clin Cosmet Investig Dent. 2020;12:465–75. doi:10.2147/CCIDE.S268527
7. Ruyter IE. Unpolymerized surface layers on sealants. Acta Odontol Scand. 1981;39(1):27-32. doi: 10.3109/00016358109162255
8. Finger WJ, Lee KS, Podszun W. Monomers with low oxygen inhibition as enamel/dentin adhesives. Dent Mater. 1996;12(4):256–61. doi:10.1016/s0109-5641(96)80032-7
9. Baroudi K, Rodrigues JC. Flowable resin composites: a systematic review and clinical considerations. J Clin Diagn Res. 2015;9(6):ZE18-24. doi:10.7860/JCDR/2015/12294.6129
10. Peumans M, Van Meerbeek B, Lambrechts P, et al. The 5-year clinical performance of direct composite additions to correct tooth form and position. Clin Oral Investig. 1997;1(1):12–8. doi: 10.1007/s007840050003
11. Wolff D, Kraus T, Schach C, et al. Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent. 2010;38(12):1001–9. doi:10.1016/j.jdent.2010.08.017
12. Gresnigt MM, Kalk W, Ozcan M. Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. J Dent. 2012;40(9):766–75. doi:10.1016/j.jdent.2012.05.010
ABOUT THE AUTHOR
Dr. Sealey graduated from Leeds Dental University in 2006 and also holds an MSc degree in endodontic practice and a master’s degree in medical education. He is a multiple-award-winning cosmetic dentist and joint owner of 2 private cosmetic dental practices in Essex, UK, where he lives. He is the co-inventor and co-owner of SmileFast and inventor of the Single-visit Orthodontic Lingual and Invisible Dual (SOLID) retention system. He has a special interest in achieving cosmetic smile makeovers using a minimally invasive approach and lectures on his techniques internationally. Dr. Sealey received the highly prestigious accomplishment of full accreditation to the British Academy of Cosmetic Dentistry in November 2022, making him one of only 14 dentists in the United Kingdom to have achieved this. He can be reached at thomas@smilefast.com.
Disclosure: Dr. Sealey reports no disclosures.


