University at Buffalo (UB) researchers have received part of a $1.5 million grant to investigate light therapy as a replacement for prescription opioids in treating oral mucositis, painful ulcers, and swelling in the mouth that result from chemotherapy and radiation treatment for cancer.
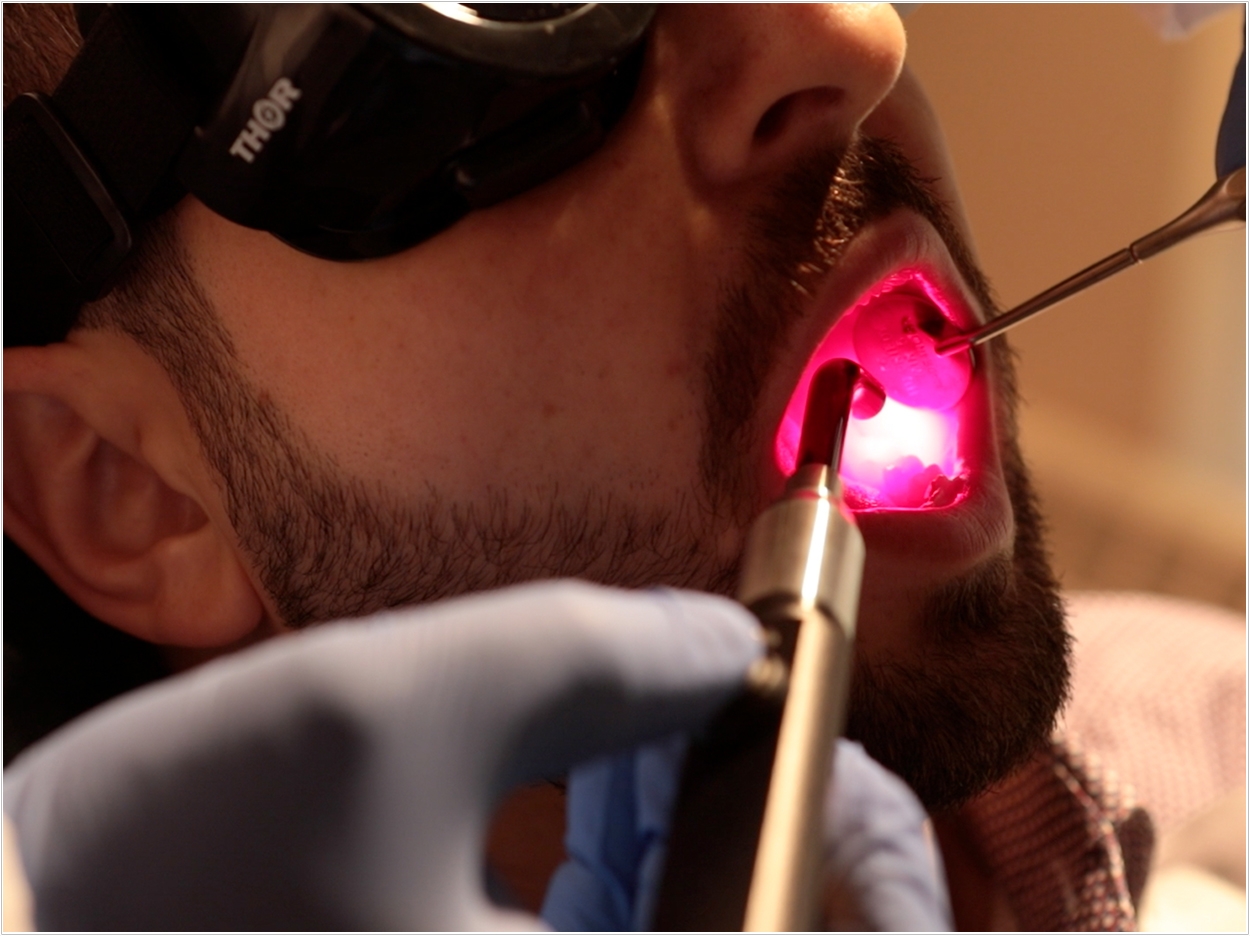
Funded by the National Institutes of Dental and Craniofacial Research Small Business Innovation Research program, the grant will help researchers determine the effectiveness of photobiomodulation, a form of low-dose light therapy, in preventing and treating oral mucositis after cancer treatment.
The grant was awarded to Cleveland-based MuReva Phototherapy, a spinoff company of lighting solutions manufacturer Lumitex, to further develop the light technology. UB received $511,000 of the award to test the technology.
“The current epidemic of opioids has impacted cancer care, especially for cancer pain relief. This treatment offers a simply, non-drug, non-invasive treatment approach to relieve pain and improve quality of life for cancer patients,” said Praveen Arany, DDS, PhD, assistant professor at the UB School of Dental Medicine.
“The striking lab and clinical evidence for photobiomodulation treatments in supportive cancer care has demonstrated tremendous promise and is becoming popular,” said Arany.
Oral mucositis is caused by damage to mucous tissue from chemotherapy or radiation treatment or stem cell transplant. It occurs in nearly 40% of patients receiving chemotherapy and nearly 80% of patients receiving radiation therapy for cancer, according to the Centers for Disease Control. Nearly 70% of those receiving stem cell transplants develop mucositis, Arany adds.
Multiple studies have found that patients report oral mucositis as the worst side effect of their cancer treatment. Pain from the condition can slow or delay treatment, and in severe cases it can require hospitalization and feeding tubes.
“In addition to the pain, it compromises a patient’s ability to eat and swallow and may even interfere with their planned treatment,” said Mukund Seshardi, DDS, PhD, professor and chair of the Department of Oral Oncology at the Roswell Park Comprehensive Cancer Center, which is collaborating in the study.
“Given these significant adverse effects on the quality of life in our patients, it is a high priority for us to find new and better ways to prevent or treat this condition,” said Seshardi.
“Right now, opioids are the most commonly prescribed drugs to address those symptoms, but they come with a whole host of problematic side effects of their own, including the potential for addiction and abuse,” said Anurag Singh, professor of oncology and director of radiation research at Roswell Park.
“So we have been looking at a number of ways to treat those symptoms while limited the need for opioids, including photobiomodulation,” said Singh, who also is a professor of medicine in the Jacobs School of Medicine and Biomedical Sciences at UB.
Light therapies have existed for decades, but improvements in the technology have made the treatment more affordable for wider use, Arany said. At a high power, light, often in the form of a laser, is used in medicine to cut or destroy tissue. But at a low level, light can relieve pain and promote healing.
Photobiomodulation’s effectiveness in treating pain and stimulating healing has been documented in hundreds of clinical trials and thousands of academic papers, UB reports. It is used widely across Europe, Canada, Australia, and elsewhere in the world. Consensus has not, however, been reached on the proper dosage for treatment, said Arany.
Using the technology developed by MuReva Phototherapy, UB and Rosewell Park researchers will examine the effectiveness of photobiomodulation treatments for oral mucositis, as well as determine the proper dosage to limit pain and stimulate healing in tissues damaged by cancer treatment.
“Current approaches for delivering a photobiomodulation-utilizing laser for oral mucositis requires a physician to spend 30 minutes per patient, per day, and is too impractical an approach for mass adoption,” said Vedang Kothari, president and CEO of MuReva Phototherapy.
“MuReva’s innovative mouthpiece, which can be self-administered, simultaneously targets a much larger portion of the oral cavity and delivers a full treatment in six minutes or less. We believe this technology has the potential to revolutionize the treatment for oral mucositis and finally present a market-ready solution to this debilitating side effect,” Kothari said.
“We are excited to partner with the University at Buffalo and esteemed clinician and professor Dr. Praveen Arany on this cutting-edge research. We believe that strong industry and academic relationships are important to advance innovative technologies to the marketplace,” said Kothari.
Arany, also president of the World Association for Photobiomodulation Therapy and co-chair of the committee on light therapy for supportive oncology care of the Multinational Association of Supportive Care in Cancer, is an advocate for wider use of photobiomodulation in the United States.
Recently, Arany participated in the first Congressional briefing on photobiomodulation before the House Science, Space and Technology Committee in Washington, DC. The briefing, held of October 11, 2018, invited a panel of international experts on the therapy to discuss the potential of photobiomodulation to improve healthcare and reduce opioid dependence.
“The ability of low-dose light therapy to promote healing has been established since the 1960s,” said Arany. “A major obstacle with its widespread use has been a lack of understanding of its precise biological mechanism. Recent work from our group has outlined both therapeutic and dose-limiting molecular pathways that are aiding development of safe and efficacious clinical protocols.”
Related Articles
Q&A: Dr. Samuel Low and Laser Dentistry
Low-Level Laser Therapy: An Alternative to Opioids in Dentistry












