“Muddy waters” is what I refer to as the real condition that exists in many hygiene departments of dental practices today. It is the common practice of providing prophylaxis treatment to patients who also have “moderate bleeding,” “4- to 5-mm pockets around posteriors,” and “stressed flossing” recorded in their treatment notes. The doctor has not made a diagnosis; therefore, there is no plan that offers the patient a treatment for his or her condition.
In these practices you will typically see a large, red S on the hygienists’ backs, because in their attempt to provide preventive care in an already diseased condition, they are trying to do everything the patient needs in one appointment, hence the “Superman syndrome.” Most dental hygiene departments operating this way do so for one of several reasons:
(1) “It is the way patients have always been managed in this practice.”
(2) “In school I was taught that a ‘cleaning’ removed all the plaque, calculus, and stains, and besides, that is how I received my license to practice…removing it all!”
(3) “If I asked my patients to come back after all these years of cleaning their teeth, then they would think something was wrong with me!”
Hygienists and doctors in practice for any length of time can appreciate how much has dramatically changed over the last 5 to 10 years in dentistry: materials, techniques, technology, and so on. However, an area more resistant to change has been the hygiene department when it comes to clinical treatment. Generally, it’s not because we do not see a need to make a shift in the way care is given. It is because we don’t know where or how to begin when it involves a departure from the way we have always done things. And frankly, we often fear rejection, or worse; fear that the patient may mistrust our motives keeps us conducting “business as usual.”
A STARTING POINT
First of all, the entire team must share and support changes that are made in the hygiene department in terms of technique, protocol, philosophy, and procedure. The quickest way to make a patient feel secure about any significant changes he or she may question is to have continuity in responses from any team member, including the doctor. So for any dental team wishing to “un-muddy” its waters, the place to begin is making sure the entire team understands the rationale and reasons behind the process.
The following are key concepts that all members of the team should carefully understand:
(1) There is no “cure” for periodontal disease, therefore early detection and treatment are paramount in achieving the best clinical results. Additionally, it is episodic and can be site specific in nature, requiring careful monitoring once it is under control in order to detect any recurrence.
(2) Periodontal disease (including gingivitis) affects the majority of adults, so it should not be a surprise that the majority of patients in any given practice could benefit from therapeutic treatment to get disease under control.
(3) Gingivitis is the earliest stage of periodontal disease, and when treated, it can be reversed to a healthy condition because there is no permanent bone loss. The downside to this reality is that until there is evidence of bone loss, most dental insurance plans do not assist the patient with any type of reimbursement to treat gingivitis beyond a routine prophylaxis visit. (Patients wanting maximum insurance benefits should be informed that if they wait, bone loss may occur, and they will receive a percentage of assistance for periodontal therapy!)
(4) Ample scientific evidence supports a 3-month, closely monitored interval for disruption of pathogenic bacteria in the subgingival environment. Maintaining this interval for periodontal patients is more likely to prevent the need for additional therapy, surgical intervention, or tooth loss.
(5) Hereditary factors as well as the numerous contributing factors that change throughout a person’s lifetime (eg, stress, hormones, medications, diet, tobacco use, etc) may affect an individual’s susceptibility to periodontal disease. Therefore, screenings at each hygiene visit are critical to assess each person’s level of periodontal health prior to any “cleaning.”
(6) We now know that periodontal disease is a bacterial infection, and the most common form of periodontitis is either a localized or generalized chronic infection.
(7) Current research indicates that periodontitis may have widespread systemic effects and serves as a risk indicator for certain systemic diseases or conditions.
(8) There are limits to successful nonsurgical treatment, so practices must establish clear guidelines for referrals based on the philosophies of both the general dentist and the periodontist.
SCREENINGS DETERMINE HEALTH VERSUS DISEASE
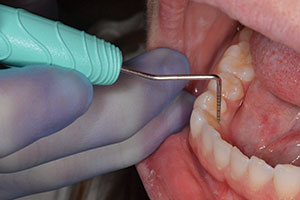
Second, a critical step to “un-muddying” the waters is beginning every hygiene visit with enough screening data to determine if the patient needs a prophylaxis today in order to maintain a healthy status or if prophylaxis is perhaps a preliminary procedure prior to active therapy due to the presence of disease.
This approach eliminates confusion on the part of the patient, who may not be informed until the end of the cleaning appointment that he or she needs to return because of “too much deposit” or “too much bleeding today.” If all hygiene appointments begin with the statement, “Let’s move you back and see how healthy your tissue is today,” then when clinical signs of periodontal infection are discovered, and the patient is able to view what is happening in his or her own mouth, it is easy to have a basis on which to discuss what can be done about it.
Before proceeding with their scheduled prophylaxis, patients should be moved into an upright position. Then the hygienist should explain (with the use of visuals) what these early signs of periodontal disease mean and how the research has changed from an emphasis on simply removing calculus to total debridement of calculus and removal of biofilm site by site to control infection.
The hygienist should be able to discuss probable treatment options even prior to a confirmed diagnosis from the doctor, so that important questions can be answered. Existing patients being presented with a diagnosis for the first time generally want a clear explanation of why “all of a sudden” they need to come back when “nothing is bothering them.” If the doctor and hygienist share the same philosophy about early detection and treatment of disease, then a united front is formed, with the hygienist being responsible for collecting data and discussing its significance with the patient and the doctor delivering a clear diagnosis upon examination. Doctors and hygienists alike must have continuity in the semantics they use to communicate with the patient, the sincerity expressed to the patient, and their inherent belief that all patients deserve to know what their current diagnosis is along with options for treatment.
Most patients, when given appropriate information, do not choose to leave periodontal infection untreated in their mouths. It simply goes untreated because either they are not aware it exists or they became convinced somewhere along the way that bleeding gums are somewhat normal for them.
USE RESOURCES WE ALREADY HAVE
The ADA made our jobs easier by giving us very clear definitions of procedures typically provided in the hygiene department. All practices, whether or not they are taking insurance assignment, should have and be familiar with the 2005 version of Current Dental Terminology (CDT 2005) in order to clarify procedures and answer patients’ questions related to insurance expectations. In the CDT 2005, the “D1110 adult prophylaxis” is described as a procedure to “remove plaque, calculus, and stains from the tooth structures and is intended to control local irritational factors.”
The definition of prophylaxis no longer states that it is restricted only to healthy patients. If a patient presents with all of the clinical signs of disease, ie, “moderate bleeding, and 4- to 5-mm pockets,” and his or her last procedure was a prophylaxis, it should be apparent that prophylaxis itself cannot control the disease. Obviously, the patient needs appropriate diagnostic data, a diagnosis of the condition, a proposed treatment plan, and appropriate information to make a wise decision about whether or not he or she wishes to treat the infection.
Once the patient is educated about the need for treatment beyond the scheduled cleaning procedure, the prophylaxis can become the initial part of the patient’s treatment. Patients should clearly be informed that prophylaxis helps to prevent disease in healthy sites, but teeth with periodontitis require a more definitive treatment procedure. A note should be made both in the record and on any claim filed for insurance that states, “Active periodontal disease diagnosed during the prophylaxis, and additional therapy is required to treat the infection.” This eliminates any confusion about prophylaxis preceding nonsurgical treatment. Of course, for patients requiring an initial debridement due to excessive deposits on the teeth, the CDT 2005 procedure “D4355 full-mouth debridement to enable comprehensive periodontal evaluation and diagnosis,” would be appropriate initially.
Depending on how current the radiographs and periodontal charts are at the time of diagnosis, the patient’s next visit following the prophylaxis (or full-mouth debridement) may be for collecting additional diagnostic data and developing the treatment plan. This could be scheduled with either the hygienist or the doctor, but it must include a doctor’s examination following the collection of comprehensive periodontal data. The CDT 2005 offers either “D0180 comprehensive periodontal evaluation” or “D0150 comprehensive oral evaluation” as options along with necessary radiographs, as indicated. If the patient already has complete diagnostic data, or it is updated during the prophylaxis appointment, then the next visit following the prophylaxis and diagnosis should be the CDT 2005 procedure, “D4341 or D4342.” The distinction between the two codes defines whether it is localized or generalized per quadrant.
Incorporation of locally applied antimicrobials (D4381) into nonsurgical periodontal treatment can assist with improved, clinically significant results compared to scaling and root planing alone, and should be included with the treatment plan to obtain the best clinical results long-term.
Once a patient has been treated for periodontitis, the appropriate procedure for all future cleanings is not prophylaxis, but rather the CDT 2005 “4910 periodontal maintenance.” This procedure will have insurance implications with less assistance than prophylaxis, but the definition describes it as “removal of the bacterial plaque and calculus from supragingival and subgingival regions, and site specific root planing where indicated for the lifetime of the dentition.” This is consistent with the understanding that disease may be episodic throughout the patient’s lifetime depending on various risk factors, the length of time between visits, daily disease control, etc. When dental teams understand that periodontal maintenance is for controlling recurrence of disease previously treated, and prophylaxis is intended to prevent disease initiation, then patients can be well-informed of the value and the difference of each.
If we are clinically providing periodontal maintenance treatment but documenting it as prophylaxis, or worse yet, alternating it with a prophylaxis to the insurance companies, then it should be no wonder that patients are confused as to why they need to come in so often or why one procedure costs more than the other when all the hygienist did was “clean their teeth.” Waters can easily be “un-muddied” here, as hygienists begin each visit with screenings to determine health versus disease. When disease recurs beyond what is realistic to treat during a scheduled periodontal maintenance visit, a new diagnosis and a new treatment plan should be presented to the patient. Communication clarifying the need for closely monitored periodontal maintenance (not prophylaxis) following additional therapy should be part of the education given at the time of a new diagnosis.
OKAY, BUT WHAT ABOUT THE GINGIVITIS PATIENT?
In cases where the periodontal infection has not progressed to the supporting periodontal structures, yet there are clinical signs of an inflammatory response present throughout the gingival tissue, patients should be informed of their diagnosis of gingivitis and given therapeutic options to treat the disease, according to the American Academy of Periodontology’s Parameters of Care. When the level of biofilm and bacterial toxins is greater than the patient’s immune response to handle it, therapeutic debridement site by site is still necessary to create an environment that is conducive to health regardless of the pocket depths.
The CDT 2005 does not specify a procedure code to treat gingivitis. Rather, it leaves it up to the discretion of the practice to include a narrative describing the need for additional appointments and/or increased fee with either a “D1110 adult prophylaxis” or “D4999 un-specified periodontal procedure, by report.” The bottom line with this issue is not how you code it, since the majority of insurance plans do not assist the patient in treating gingivitis prior to permanent bone loss.
The point is that you treat it, since gingivitis is the only stage of periodontal disease that is reversible. The number of subsequent visits necessary to treat gingivitis would depend on the severity of the infection and relevant contributing factors.
CLARITY INCREASES VALUE TO PATIENTS AND TEAM
One of the greatest benefits of clarifying the “muddy waters” in hygiene departments is that it creates a realistic framework from which to diagnose and treat a disease that can have potential health and/or legal implications for the patient and/or practioner, if ignored.
In practices willing to begin the process of “un-muddying” the waters, a heightened enthusiasm occurs when the dental team experiences the rewards of helping patients to become truly healthier. Additionally, it becomes an opportunity for patients to see the real value of consistent preventive care, since the beginning of every visit begins with a screening to detect disease. Seldom now do we hear patients say, “I need to reschedule my appointment for next week…it’s just a cleaning.” By recognizing disease, informing patients of it, and treating it appropriately, the value of various procedures truly becomes clear. The end result is a hygiene department that offers a pathway to optimal oral health, with support from the entire team, and patients who own their health.
Don’t let your own comfort with the way things have always been done stop you from practicing on the cutting edge of your profession. Instead, use this information as your springboard to start un-muddying your own waters, and enjoy crystal-clear rewards.
Ms. Davis is a private practice hygienist, consultant for The JP Institute, and an international speaker in the dental profession. She may be reached at (972) 669-1555 or karen@karendavis.net.