INTRODUCTION
Losing a tooth can be traumatic for dental patients—affecting their ability to chew, digest, and speak, as well as their self-esteem.1 Implant protocols have been redefined to satisfy patients’ expanding expectations for comfort, aesthetics, and shorter treatment times.2 All of these are excellent reasons to explore immediate implant placement procedures rather than delayed implant placement.3 Utilizing a final titanium abutment at the time of implant placement has also been shown to additionally compress treatment times.
My introduction to the concept of using definitive abutments at the time of implant placement resulted from a fortuitous circumstance. Following an extraction and an immediate implant in a patient, I discovered that I only had a final titanium abutment instead of a provisional abutment. I placed the final abutment, covered the grafted area with platelet-rich fibrin (PRF) to promote bone and soft-tissue regeneration, prepared and provisionalized the abutment, and recalled the patient one week later.
The peri-implant tissue response looked magnificent. I subsequently used this paradigm for several additional cases, all with the same outcome. These experiences led to an interesting paradigm change for me—and I hope, after reviewing this case report, for my colleagues as well.
One Abutment-One Time
I am among a group of clinicians who now use a final definitive abutment at the time of surgery. The concept of “one abutment-one time” was the focus of a clinical trial by Canullo et al4 in 2010. The aim of the randomized clinical trial was to evaluate the influence of restoration on marginal bone loss using immediate definitive abutments vs provisional abutments later replaced by final abutments. Dr. Marius Steigmann has noted that foregoing the temporary abutment prevents apical movement of the tissue and, as a consequence, apical resorption of the crestal bone. This actually stabilizes the dentogingival complex, making the soft-tissue architecture more stable both short- and long-term.
The term “one abutment-one time” refers to the connection of an immediate non-removal abutment in a post-extractive implant.5 A study by Grandi et al noted another study’s findings on the concept: “Within the limits of this study, it can be suggested that the non-removal of abutments placed at the time of surgery results in a statistically significant reduction of the crestal bone resorption around the immediately restored implants in cases of partial edentulism….”6
Bone Remodeling
Many factors affect bone remodeling for the success of a dental implant. They include:
l A microgap at the implant/abutment interface
l Micromovement at the implant-abutment interface
l Microleakage between the implant and the abutment
l Abutment disconnection or reconnection7
CASE REPORT
Socket Shield Technique
This patient was treated using the socket shield technique. The technique involves partial extraction of the tooth while leaving a buccal fragment in situ, followed by the immediate placement of a dental implant. This dentin shield is designed to prevent the buccal cortical bone from resorbing.8
The case study included in this report involves a 21-year-old, white, female patient. The chief complaint was external resorption of the maxillary right central incisor. Radiographs found an erosive lesion distal to the root of tooth No. 8 (UR central incisor). Clinically, a 5-mm circumferential resorptive lesion was observed below the CEJ that had a hopeless prognosis (Figure 1).
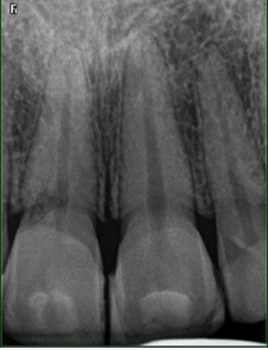
Figure 1. Initial radiograph with evidence of external resorption.
A CBCT scan was obtained to determine the position of the tooth within the alveolus. The tooth was in a Type I position with the root positioned to the facial. This made it an ideal candidate for partial extraction therapy. An extraction was planned with immediate implant placement and a final titanium abutment. The implant used was a Ditron ULT Ultimate 3.75- × 15-mm implant (Ditron Dental USA) with an 11.5-mm, narrow, straight titanium abutment.
The patient obtained medical clearance for implant surgery. Informed consent for the procedure was reviewed, and the consent form was signed and witnessed. Whole blood was drawn for the fabrication of PRF and for hydration of bone graft material with autologous fibrin. The patient was sterile draped and monitored and had a preoperative chlorhexidine rinse for one minute. Two carpules of 2% carbocaine containing 1:20,000 levonordefrin were administered facially and palatally, and surgery was commenced.
Using a long diamond bur, the clinical crown was removed to 1 mm above the gingival margin (Figure 2).

Figure 2. Cutdown of clinical crown.
The pulpal canal was identified and used as the guide for the socket shield burs that were used sequentially to enlarge the root preparation (Figure 3).

Figure 3. Preparation of root to create a socket shield.
Root cuts were performed at the mesio-palatal and disto-palatal line angles, and a No. 2 surgical length round bur was used to separate the apex from the facial root complex. The palatal root segment was carefully removed from the osteotomy, and the socket shield was thinned and reduced occlusally to 1.5 mm above the parabolic crestal architecture (Figure 4).
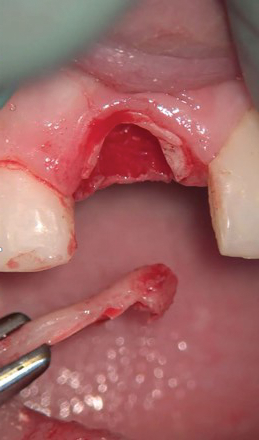
Figure 4. Removal of the palatal segment and apex.
An Er,Cr:YSGG laser (Waterlase iPlus [BIOLASE]) was used for final debridement of the osteotomy, removing remnants of the gingival sulcus and periodontal ligament and any potential periapical pathology. A Ditron ULT Ultimate implant (3.75- × 15-mm) was coated with autologous serum to condition the titanium oxide surface (Figure 5) and placed to an ideal axial position within the osteotomy (Figure 6).
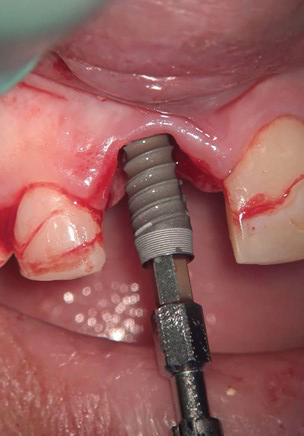
Figure 5. The implant was coated with autologous serum.
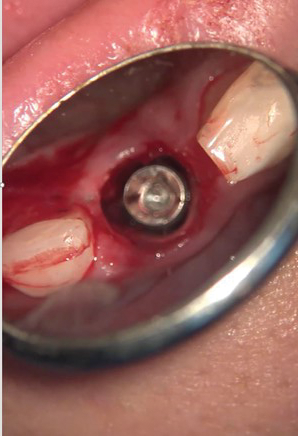
Figure 6. Ideal axial placement of the implant.
A cover screw was placed prior to the grafting procedure to prevent contamination of the internal part of the implant.
The extraction site gap was grafted circumferentially with an OsteoGen (IMPLADENT LTD) bone strip hydrated with autologous plasma (Figure 7). The graft was adapted to the height of the implant body, and the cover crew was removed (Figure 8).
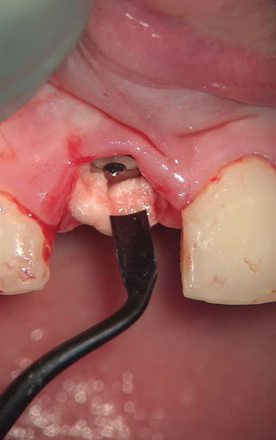
Figure 7. OsteoGen (IMPLADENT LTD) bone graft in the extraction site gap.
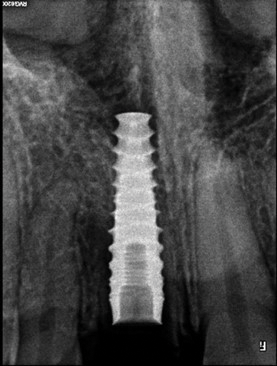
Figure 8. Grafted implant with the cover screw removed.
A final 11.5-mm, narrow, straight titanium abutment was placed and torqued to 35 Ncm (Figure 9).

Figure 9. Placement of the definitive titanium abutment.
A Teflon plug was placed, and the screw access chamber was sealed with light-cured flowable composite. A final circumferential PRF membrane was placed to fill the soft-tissue defect and protect the gap from contamination during preparation of the abutment (Figure 10).
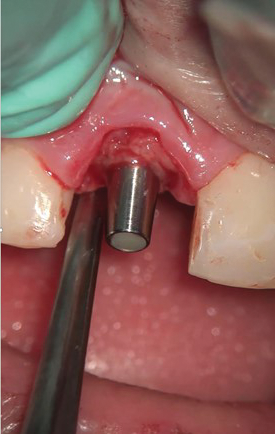
Figure 10. Circumferential PRF membrane.
The titanium abutment was then prepared with a new 558 crosscut fissure bur to ideal parameters (Figure 11). The abutment was then provisionalized with Protemp (3M) resin material and cemented with temporary Implant Cement (Premier Dental).

Figure 11. Prepared final titanium abutment.
The implant site was then followed postoperatively for 2 months while the hard- and soft-tissue complex matured (Figures 12 and 13).

Figure 12.

Figures 12 and 13. Preoperative and 2-month postoperative photographs of the dentogingival complex.
Why Specific Implants Were Chosen
For this patient, I chose the Ditron ULT Ultimate because of its excellent initial stability. This implant’s architecture is ideal for creating a stable implant interface at the time of extraction. Two features of this implant particularly concentrate on immediate load stability. According to Ditron USA, the Reverse Concave Neck (RCN) increases the implant contact surface area to preserve marginal bone and soft tissue.8 The taper, concavity, and microthreads of the collar provide atraumatic implant-to-bone contact by decreasing pressure to the cortical bone. The RCN design provides greater stability and improved distribution of the stress to the bone-implant interface.
In this case, a CBCT scan was taken to evaluate healing and the condition of the socket shield (Figure 14).

Figure 14. Two-month post-op CBCT evaluation.
The old veneers were removed from teeth Nos. 7, 9, and 10.
Final impressions were then taken for the definitive restorations, and the case was restored 2 weeks later.
DISCUSSION
Prevention of crestal bone loss is an essential element in extraction/immediate implant placement, especially in the aesthetic zone. Selection of an implant system that gives us excellent initial stability and is combined with an abutment connection system that significantly reduces microleakage contributes to success in this paradigm. A precise abutment connection, known as MolecuLock, improves stability by reducing micromovement to further protect the healing tissue complex and contributes to successful osseointegration.
The seal reduces the egress of bacteria, protecting crestal bone and soft-tissue from the risks of peri-implantitis. The biomechanical implant-abutment seal is designed to reduce microgaps to less than 0.5 μm—too narrow for bacteria to penetrate. The implants share one abutment platform: a 2.45-mm internal hex implant-abutment connection across all diameters.
In addition, the soft-tissue attachment to the definitive titanium abutment actually stabilizes the position of the tissue on the prosthetic interface and also prevents crestal bone resorption as a consequence.
CLOSING COMMENTS
Staying current on techniques and implant systems that boost initial stability is a key component of maintaining the integrity of the implant site over the long term. While my past protocol involved using a healing or provisional abutment, waiting for the site to heal, and then taking impressions and making the final abutment, to my pleasant surprise, placing the definitive abutment at the time of implant placement shortens treatment time and gives me a better clinical outcome.
REFERENCES
1. Singh M, Kumar L, Anwar M, et al. Immediate dental implant placement with immediate loading following extraction of natural teeth. Natl J Maxillofac Surg. 2015;6(2):252–5. doi:10.4103/0975-5950.183864
2. Tettamanti L, Andrisani C, Bassi MA, et al. Immediate loading implants: review of the critical aspects. Oral Implantol (Rome). 2017;10(2):129-139. doi:10.11138/orl/2017.10.2.129
3. Ebenezer V, Balakrishnan K, Asir RV, et al. Immediate placement of endosseous implants into the extraction sockets. J Pharm Bioallied Sci. 2015;7(Suppl 1):S234-S237. doi:10.4103/0975-7406.155926
4. Canullo L, Bignozzi I, Cocchetto R, et al. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow-up of a randomised multicentre clinical trial. Eur J Oral Implantol. 2010;3(4):285–96.
5. Santos JS, De Santana Santos T, Martins-Filho PRS, et al. One abutment at one time concept for platform-switched morse implants: systematic review and meta-analysis. Braz Dent J. 2018;29(1):7-13. doi:10.1590/0103-6440201801686
6. Grandi T, Guazzi P, Samarani R et al. Immediate positioning of definitive abutments versus repeated abutment replacements in immediately loaded implants: effects on bone healing at the 1-year follow-up of a multicenter randomized controlled trial. Eur J Oral Implantol. 2012;5(1):9-16.
7. Dayakar MM, Waheed A, Bhat HS, et al. The socket-shield technique and immediate implant placement. J Indian Soc Periodontol. 2018;22(5):451–5. doi:10.4103/jisp.jisp_240_18
8. Ditron Dental USA. ULT: Ultimate Precision Implants. https://www.ditrondentalusa.com/ult-ssp.
ABOUT THE AUTHOR
Dr. Miller received his BA degree from New York University and his MA degree from Hofstra University. He graduated with honors from the New York University College of Dentistry in 1981 and then completed his residency at Flushing Medical Center in New York City.
Dr. Miller is a Fellow of the American College of Dentists, a Diplomate of the American Board of Oral Implantology, an Honored Fellow of the American Academy of Implant Dentistry, a Diplomate of the International Congress of Oral Implantologists, a Fellow of the Academy of Osseointegration, and the chairman of the Department of Oral Implantology at the Atlantic Coast Dental Research Clinic in Palm Beach, Fla.
He is director of the Center for Advanced Aesthetic and Implant Dentistry in Delray Beach, Fla, where he has a full-time practice dedicated to implant dentistry and revision surgery.
He can be reached at drrjmiller1@aol.com.
Disclosure: Dr. Miller has a financial relationship with Ditron Dental USA.











