INTRODUCTION
A narrow upper jaw (maxilla) can cause cross-bite in the lateral region and different gradations of overbite in the anterior region. This can cause an aesthetic appearance problem and is often associated with psychological discomfort for the patient. In order to accomplish normal occlusion, function, and a better overall look, orthodontics and extensive surgical treatment are often required in adults. However, orthodontic treatment combined with an osteotomy is not always the first treatment of choice because of the many uncertainties of these complex treatments.
Aesthetic rehabilitations using composite resins are becoming more attractive especially for patients who seek a minimally invasive and a straightforward approach to their aesthetic problems.1 In order to acquire excellent aesthetic results using composite resin that serves the needs of each particular patient, extensive communication with patients and comprehensive treatment planning are essential.2-5
The best way to improve communication with patients is to show them the possible aesthetic results that can be achieved with the proposed treatment before beginning any operative procedures. Moreover, the visualization of the final aesthetic outcome previous to a treatment will increase the patient’s acceptation of the post-treatment alterations.3-5 Finally, the dentist can use this visualization to discover all possible obstacles that can be met during the treatment.3-5 This aesthetic visualization can be achieved with different methods. For aesthetic changes that can be performed without tissue reduction, it is possible to visualize the result by employing nonadhesive composite addition and shaping (composite mock-up). In more complex cases, where the correction of teeth position and changes in occlusion and articulation are needed, the visual presentation of the final result by using the nonadhesive addition of composite could be insufficient. Moreover, patients might need to take their time to consider whether suggested aesthetic results are acceptable, or they might need to discuss the projected aesthetic changes with their family. For those patients, a composite mock-up might be an inadequate option. In such cases, the treatment planning can be performed digitally (dental imaging) using a specially selected drawing-tool set (eg, Paint Shop Pro X [Corel]) and a methodology developed by the authors.
In cases of complex and extensive dental corrections, it might be preferable to split the treatment into 2 or more phases. After the initial aesthetic correction, the patient can take some time to get acquainted to the proposed changes and to think about the possibility of embracing a more extensive correction. Moreover, after the period of customization to the first alteration, the patient will gain more trust for the clinician, thus enhancing the success rate of the ultimate aesthetic improvement.
This case report describes the dynamic approach to an aesthetic correction of a tapered upper jaw with composite resin restorative materials. Due to the complexity of the aesthetic correction, the clinical treatment was divided into 2 phases: the initial correction and the final correction. Part 1 of this article presents the initial preparation of a 2-phase complex aesthetic rehabilitation and the treatment planning of the ultimate aesthetic improvement achievable with composite, by means of digital visualization. Part 2 of this article will cover the composite mock-up of the initial result, and the clinical procedure of the final treatment will be discussed in detail.
CASE REPORT
Diagnosis and Treatment Planning
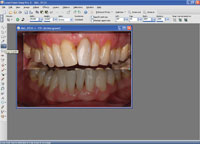
A 38-year-old male patient with a tapered upper jaw, moderate overbite, midline displacement, and extensively restored anterior teeth (tooth No. 9 had a history of endodontic treatment) expressed the need for improved aesthetics of his smile (Figures 1 and 2). After evaluation of the patient’s wishes and expectations, the clinical data were collected. Gypsum models and 3 identical wax indices were made for the occlusion and articulation analysis and for the initial wax-up (Figure 3). For this particular patient, an orthodontic treatment was not a consideration and he wished for an optimal aesthetic result with minimum tooth preparation of healthy tissues.
 |
 |
| Figure 1. Preoperative frontal view. | Figure 2. Preoperative lateral view. |
 |
| Figure 3. A diagnostic wax-up model was fabricated to assess the practical possibilities for improved aesthetics and to produce a silicone index for later use in the provisionalization phase. |
The authors could clearly see that a more extensive treatment with composite was required in order to meet the patient’s desire for improved dental aesthetics. Therefore, the treatment was divided into 2 phases; the first phase was reserved for the initial aesthetic correction of the frontal area.
In order to establish better symmetry in the frontal area with only slight corrections, it was chosen to make a composite buildup of the left central incisor No. 9, a Class IV composite restoration of the mesioincisal aspect of the right central incisor No. 8, and composite veneers on the left lateral and central incisors, teeth Nos. 9 and 10. The second phase of the treatment was reserved for composite buildup of the buccal and occlusal aspects of the 4 upper incisors, left and right canines, and the premolars; this would be done to simulate an expansion of the buccal corridor. The patient was informed that, depending upon his satisfaction after the initial treatment, a choice could be made to continue with more extensive treatment with composite.
Initial Treatment
Before the start of the initial treatment, the basic color of anterior teeth was assessed visually using VITA Classical shade tabs [Vident]. The determined color was A3. After color determination, the old fillings in the central incisors (Nos. 8 and 9) were removed and the left central and lateral incisors (Nos. 9 and 10) were slightly grinded buccally in order to prepare the surface for composite facings (Figure 4). The buildup of the facings was done by freehand technique with aid of a silicone index (Memosil [Heraeus Kulzer]) that was fabricated from the initial diagnostic wax-up.6,7 The silicone index was cut through in order to obtain a palatal and a buccal section. The palatal index helped to appropriately shape the palatal surface of the incisors and to omit incisal disturbances and material excess.7 The buccal section of the index was used to get an indication whether the amount of tissue that has been removed buccally provided sufficient space to mask the teeth discolorations with composite.2 In order to keep the mesial and distal aspect of the restored teeth in a tight but separated contact, very thin Teflon tape (0.02 mm) was used (Figure 5).6 First the tooth No. 8 was restored in order to assess the vertical midline and to determine the shape of tooth No. 9, then mesial and distal surfaces of each upper incisor were restored with hybrid composite (Z250 [3M ESPE]). Thereafter, the facings were made using the transparent Contour strips (Ivoclar Vivadent) with a microhybrid composite (Anterior Shine [Cavex]) (Figure 6).
 |
 |
| Figure 4. Maxillary anterior teeth after the removal of the old composite restorations. | Figure 5. Palatal index and Teflon tape in situ for buildup of tooth No. 9. |
 |
 |
| Figure 6. The use of Contour strip (Ivoclar Vivadent) for proximal and vestibular buildup. | Figure 7. Frontal view directly after the initial aesthetic correction. |
 |
 |
| Figure 8. Lateral view 2 years after the initial correction. |
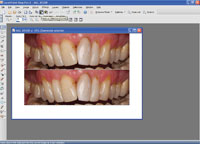
Figure 9. Two years after the initial aesthetic correction. |
The patient was very satisfied with the look of his anterior teeth after the initial treatment (Figures 7 to 9). Within several weeks he had gotten accustomed to the new form and function of his teeth. This resulted in his wish to find out more about the possibilities to improve his smile with more extensive treatment, as suggested earlier. In this stage, the authors decided to visualize the possibilities of the more extensive treatment using a digital mock-up.
Digital Imaging and Image Manipulation (Visualization)
Digital imaging is a noninvasive and effective communication means for presentation of treatment options.3,4,8 A clinician can use digital imaging to discover whether the possible treatment options can satisfy the patient’s needs and to discover possible obstacles (Figures 10 and 11).3-5
 |
 |
| Figure 10. Example of digital imaging for closing of diastemas. | Figure 11. Example of digital imaging for the replacement of restorations and adjusting the shape of teeth. |
 |
 |
 |
 |
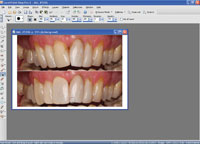 |
| Figures 12 to 16. Different phases in digital image manipulation (crop, canvas, paste, push/sculpt). |
For the purpose of the digital mock-up of the presented case, standardized photographs of the initial treatment result were used. They were analyzed in order to discover discrepancies to normal jaw relations and symmetry, and to brainstorm about possible corrections with composite resin. For dental imaging, Paint Shop Pro X and a graphic pen tablet (Wacom [Bamboo One]) were used. First, the original photograph was cut out (Figure 12) with the “crop” tool, then copied and pasted underneath the original (after enlarging the canvas) (Figures 13 and 14). The upper part in the enlarged canvas was used as a reference and the lower part for imaging (Figure 15). Using the tools “push,” “select,” “copy,” “paste as selection,” and “darker/lighter” (Figure 16), the original image was manipulated toward a possible treatment result, showing the changes possible and also the limitations in this particular case (Figure 17). Finally, the digital transparent molds were made and placed (“pasted”) on top of the original photograph as a layer with 50% transparency (Figure 18). The patient was impressed with the aesthetic possibilities. He took the photographs of the planned final result with him in order to discuss the proposed changes with his partner.
 |
 |
| Figure 17. The new look of the smile after the image manipulation. |
Figure 18. The manipulated image was made transparent (50%) and then projected over the original. |
The appointment for the composite mock-up was made after 4 weeks. The purpose of the composite mock-up was to improve the alterations in the mouth and to let the patient feel whether he can get used to possible changes. This mock-up will be discussed in part 2.
CONCLUSION
Thanks to the improved strength and superb optical properties of modern composites, aesthetic treatments with this class of restorative materials are becoming more and more popular compared to more invasive procedures. This material is an excellent medium for dynamic and reversible aesthetic alterations. It offers possibilities for phased treatment in more complex cases and finally, if necessary or desired in the future, orthodontics, surgery, and irreversible restorative techniques are still obtainable.
A totally noninvasive method for visualization of treatment planning is digital manipulation of dental images. A relatively inexpensive and simple to use digital imaging program (eg, Paint Shop Pro X) is available for such purposes. All patients (or family members and significant others) can see the proposed aesthetic corrections, take the time to think it through, and eventually give their opinion about it before the actual treatment has started. A patient can also get a good idea about the possible limitations of the treatment, which could enhance satisfaction with the final result.
References
- Roeters J, de Kloet H, Jeurissen A. Handboek Voor Esthetische Tandheelkunde. 2nd ed. Nijmegen, The Netherlands: STI; 2005.
- Atlas of PLVs. In: Gurel G. The Science and Art of Porcelain Laminate Veneers. Chicago, IL: Quintessence Publishing; 2003:231-344.
- Papasotiriou OS, Nathanson D, Goldstein RE. Computer imaging versus conventional esthetic consultation: a prospective clinical study. J Esthet Dent. 2000;12:72-77.
- Goldstein RE. Attitudes and problems faced by both patients and dentists in esthetic dentistry today: an AAED membership survey. J Esthet Restor Dent. 2007;19:164-170.
- Goldstein RE, Garber DA. Improving aesthetic dentistry through high technology. J Calif Dent Assoc. 1994;22:23-24, 26,28-29.
- Dozic A. Praktische werkwijzen om voorspelbaarheid van esthetische kleur- en vormuitkomst van composietrestauraties te vergroten. ACTA Quality Practice. 2008/2009;4:19-28.
- Vanini L, Mangani F, Klimovskaia O. Conservative Restoration of Anterior Teeth. Viterbo, Italy: ACME; 2005.
- Goldstein CE, Goldstein RE, Garber DA. Imaging in Esthetic Dentistry. Chicago, IL: Quintessence Publishing; 1998.
Dr. Dozic is assistant professor at Academic Centre for Dentistry in Amsterdam, the Netherlands, and guest professor at Faculty of Dentistry in Sarajevo, Bosnia, and Herzegovina. She also works in a private dental practice specializing in restorative dentistry in Amsterdam. She received her PhD in Dental Materials Sciences on theme “color of teeth” in 2005. She is lecturing in a master phase of dental curriculum and postacademically covering different aspects of aesthetic dentistry. She is also conducting research implying: electronic color determination, optical properties of dental materials, color change of teeth due to external factors, and the aesthetic outcome of different restorative methods in clinical dentistry. She has published more than 26 articles internationally and is the editor of the Annual Book About Dental Esthetics in the Netherlands. She maintains membership in many professional associations and academies. She can be reached at (0031) 617452560 or via e-mail at a.dozic@acta.nl.
Disclosure: Dr. Dozic reports no disclosures.
Dr. de Kloet studied dentistry at Free University in Amsterdam, the Netherlands. Since his graduation in 1974, he has been involved in research and clinical practice in the field of direct adhesive-aesthetic-composite dentistry, exploring the technical and aesthetic limits of composite materials. Currently, Dr. de Kloet works part-time at the Academic Centre for Dentistry in Amsterdam, where he organizes postgraduate courses in Holland and Belgium. He is co-author of more than 30 publications and 2 textbooks about aesthetic composite dentistry, in Dutch and German, with Joost Roeters of the Dental School of Radboud University, Nijmegen. He lectures internationally for 3M ESPE, Kerr, and Ivoclar Vivadent and for national and local associations of dentistry. He also is a renowned lecturer on digital dental photography. He can be reached via e-mail at h.dekloet@chello.nl.
Disclosure: Dr. de Kloet reports no disclosures.


