Conserve Tooth Structure, Grow Your Practice, and Increase ROI
INTRODUCTION
Would you want your dermatologist to just monitor a suspicious skin lesion or to conduct a definitive biopsy? Dentists face a similar challenge when diagnosing a suspicious occlusal lesion with no evidence of cavitation from radiographs or that is inconclusive from visual examination. Is it a stain, is the lesion confined to the enamel, or is it cavitated and progressing into the dentin? Do we watch and wait or proceed with a restoration?
Telling the patient “let’s watch this until the next visit” is inappropriate and does not instill patient confidence in the quality of our care. Our mission is to diagnose disease as early as possible using every tool available. I have used the Ortek-ECD (electronic caries detection) device (Ortek Therapeutics) on hundreds of patients.
I believe it significantly takes the guesswork out of detecting early cavitated occlusal lesions and helps us avoid unnecessary restorations.
Dental caries remains the most prevalent chronic disease in both children and adults. A primary goal of current caries management is to detect dental caries lesions as early as possible. This is particularly true for occlusal caries, where significant tooth damage, and even tooth loss, can occur due to late caries detection.1
Occlusal surfaces of posterior teeth are very prone to caries development because these surfaces possess a morphology (ie, pits and fissures) that favors retention of both fermentable carbohydrates and bacterial biofilms. Suspicious or questionable occlusal lesions are commonly encountered in general dental practice, with approximately one-third of patients exhibiting such a lesion at any given time.2
We know that radiographs and visual examinations have limitations in detecting early occlusal lesions accurately. It is now suggested that explorers should not be used for caries detection because they might spread bacteria from one area to another, present incomplete or inaccurate data, and/or may actually break an intact surface layer and disrupt remineralization.
Radiographic detection of interproximal decay is very effective. The usefulness of radiographs for detecting occlusal caries is limited. Experiments indicate that once an occlusal lesion is clearly visible on radiographs, demineralization has extended to or beyond the middle third of the dentin.3
Visual inspection of occlusal lesions remains an important diagnostic method, but we know that visual inspection is subjective. It would be helpful if we could confirm our diagnosis of early occlusal lesions with a “second opinion” from another diagnostic tool that has superior sensitivity and specificity and provides quantitative results.
In recent years, several caries detection devices have been developed and introduced to dental practitioners. These systems typically utilize light fluorescence or laser-based technologies. For more than one year, I have incorporated a new caries detection device into my practice called the Ortek-ECD (Figure 1).

Figure 1. The Ortek-ECD (Ortek Therapeutics) was tested and developed in the Department of Oral Biology and Pathology at the Stony Brook University School of Dental Medicine.
The ECD is an extremely affordable device that utilizes electronic conductance technology. It was tested and developed in the Department of Oral Biology and Pathology at the Stony Brook University School of Dental Medicine. The ECD demonstrated 100% sensitivity and 93% specificity in a peer-reviewed, published study conducted at Stony Brook.
If the dentin-enamel junction is breached by demineralization, hydrostatic pressure that exists within dentinal tubules will allow minuscule amounts of conductive dentinal fluid to enter the breached enamel site, allowing the ECD to complete an electrical circuit. The more fluid detected results in lower resistance, a higher current, and an increasing caries score that is digitally displayed from 01 to 100. Tooth enamel is a good insulator and is electrically nonconductive.
When the enamel at the bottom of a pit or fissure is intact, the circuit path is opened, and no current can flow. A zero score indicates a non-cavitated lesion or stain.
Using the ECD is fast and easy, and it operates on a 9-V battery. After placing the reference lip hook on the patient and isolating the teeth to be examined with cotton rolls, I take the conductive tip that has been attached to the handpiece and gently run the tip along the grooves of the tooth to ensure that the tooth is 100% clean.
I always do it twice and always check the probe for residual debris.
The occlusal surface must be completely dry, which is accomplished with a 5-second air blast. Then I place the conductive tip (Figure 2) into the bottom of a pit or fissure, and the ECD will provide a digital reading from 01 to 100 and an audible beep if caries are detected.

Figure 2. The ECD’s conductive tip.
CASE REPORTS
CASE 1
In this case, a 38-year-old female was examined during a routine dental exam: Teeth Nos. 20 and 21 displayed discoloration, possibly due to staining. Radiographs were taken, and there was no sign of cavitation (Figure 3). Prior to preparation, the ECD provided caries scores of zero for tooth No. 21 and 8 for tooth No. 20 (Figure 4).
After administration of local anesthesia, decay was detected and excavated (Figure 5).

Figure 3. The radiograph showed no sign of cavitation in tooth No. 21.

Figure 4. Prior to preparation, the ECD provided caries scores of zero for tooth No. 21 and 8 for tooth No. 20.

Figure 5. After administration of local anesthesia, decay was detected and excavated.
CASE 2
In this case, a 49-year-old male was examined during a routine dental exam. Teeth Nos. 28 and 29 displayed discoloration, possibly due to staining. Radiographs were taken, and there was no sign of cavitation (Figure 6). Prior to preparation, the ECD provided caries scores of 10 for tooth No. 28 and 11 for tooth No. 29 (Figure 7). After administration of local anesthesia, a 556 bur was used. Decay was detected, and the tooth was excavated and restored (Figure 8).

Figure 6. The radiographs of teeth Nos. 28 and 29 showed no sign of cavitation.

Figure 7. Prior to preparation, the ECD provided caries scores of of 10 for tooth No. 28 and 11 for tooth No. 29.

Figure 8. Decay was detected and excavated, and the tooth was restored.
CASE 3
In this case, a new 32-year-old female patient was given an initial routine exam. The patient indicated that her prior dentist had been watching the “stain” on tooth No. 2 for years. Radiographs were taken, and there was no sign of cavitation (Figure 9). Prior to preparation, the ECD gave a reading of 30 (Figure 10). After administration of local anesthesia, a 556 bur was used, and the decay was excavated (Figure 11). As can be seen, the decay was deep and wide.
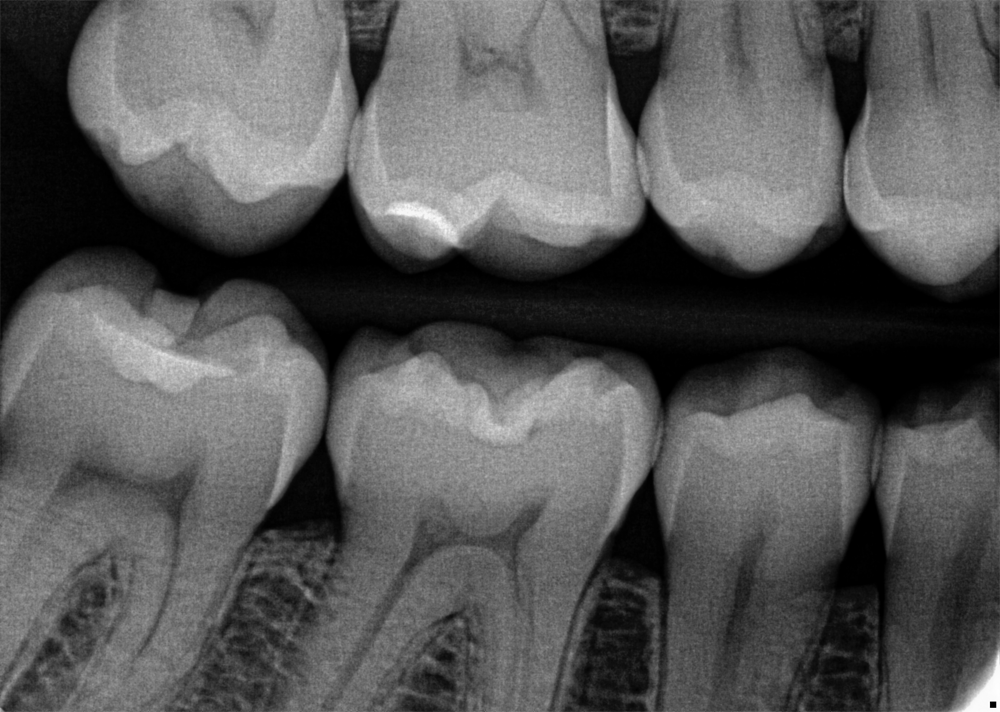
Figure 9. The radiograph of tooth No. 2 showed no sign of cavitation.

Figure 10. Prior to preparation, the ECD gave a reading of 30.

Figure 11. After administration of local anesthesia, a 556 bur was used, and the decay was excavated. As can be seen, the decay was deep and wide.
CONCLUSION
We are trusted with the responsibility to diagnose our patients’ health issues as early as possible. Until now, there had not been a way for me to feel entirely confident during the early diagnosis of occlusal carious lesions when radiographs showed no signs of cavitation and visual examinations were inconclusive.
The ECD allows me to save tooth structure by detecting an occlusal lesion that has extended into the dentin at a very early stage. Just as important, the ECD also helps me avoid unnecessary restorations. The feedback from my patients has been amazing. They are impressed when I compare the ECD’s digital readout to the before and after intraoral images.
They are also ecstatic when the ECD provides a zero reading and I can recommend noninvasive remineralizing treatments and follow-up examinations.
REFERENCES
1. Chatterjee R, Acevedo AM, Kleinberg I. Comparison of the detection of early occlusal caries in extracted human permanent molar teeth by electrical conductance and biopsy means. J Clin Dent. 2019;30(2):1-5. https://pubmed.ncbi.nlm.nih.gov/31310709/
2. Makhija SK, Gilbert GH, Funkhouser E, et al; National Dental Practice-Based Research Network Collaborative Group. The prevalence of questionable occlusal caries: findings from the Dental Practice-Based Research Network. J Am Dent Assoc. 2012;143(12):1343–50. doi:10.14219/jada.archive.2012.0097
3. Ricketts DN, Kidd EA, Smith BG, et al. Clinical and radiographic diagnosis of occlusal caries: a study in vitro. J Oral Rehabil. 1995;22(1):15-20. doi:10.1111/j.1365-2842.1995.tb00205.x
ABOUT THE AUTHOR
Dr. Rosen received his DDS degree from New York University Dental School. He maintains a general dentistry practice in Lynbrook, NY, with an emphasis on prevention and early diagnosis of dental lesions. He has lectured and is a published author. Dr. Rosen can be reached at rosendds@optonline.net.












