Researchers from the New York Institute of Technology have developed computer simulations showing how lasers set at different wavelengths can attack oral bacterial colonies, suggesting that the benefits of using lasers in oral debridement include killing bacteria buried in gum tissue and promoting better dental health.
“The paper verifies or validates the use of lasers to kill bacteria and contribute to better health following periodontal treatments,” said co-author Lou Reinisch, PhD, associate provost for academic affairs at New York Institute of Technology and an expert in laser surgery with a background in physics, optics, and calculus.
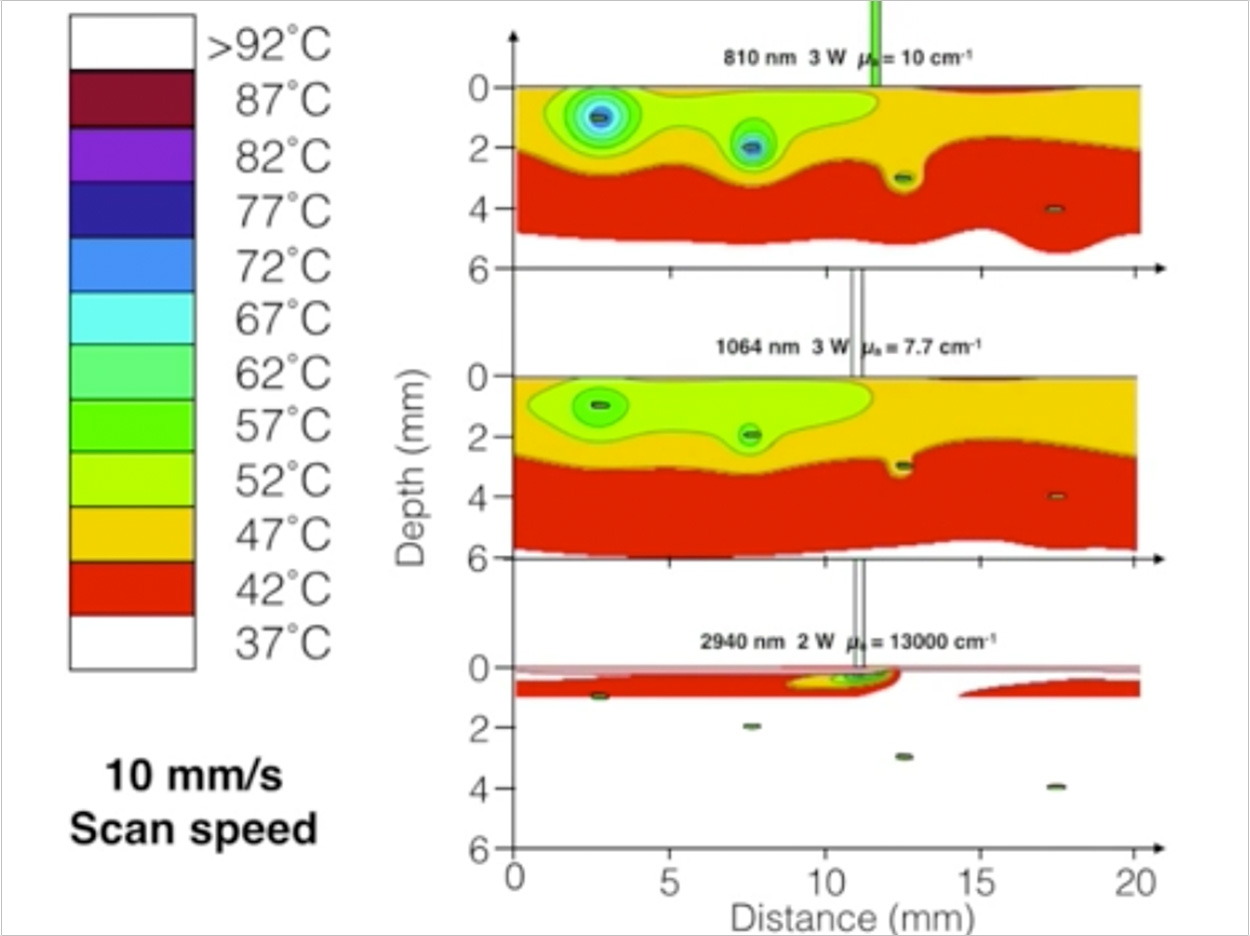
Reinisch created mathematical models based on the optical characteristics of gum tissues and bacteria. He then produced simulations of 3 different types of lasers commonly used in dentistry and their effects on 2 types of bacterial colonies of various sizes and depths within the gum models.
“One of the questions we asked is how deep could the bacteria be and still be affected by the laser light,” said Reinisch.
The simulations indicate that 810-nm diode lasers, set to short pulses and moderate energy levels, can kill bacteria buried 3 mm deep in the soft tissue of gums. The 1064-nm Nd:YAG laser also is effective with similar penetration. Both lasers spare healthy tissue with minimal heating of the surrounding tissue. Minimizing thermal damage accelerates healing, said Reinisch.
“The findings are important because they open up the possibility of tweaking the wavelength, power, and pulse duration to be the most effective for killing bacteria,” said Reinisch. “The doctors will look at this and say, ‘I see there is a possible benefit for my patients in using the laser.’”
“The study reveals what’s going on in the tissue, so I hope that we’re educating the medical professionals by demonstrating that you can do a good job of killing bacteria with certain lasers,” said co-author David Harris, PhD, director of Bio-Medical Consultants, which specializes in medical laser product development.
“When you do this treatment, you remove an infection and allow tissue to regenerate. Getting rid of the infection means the tissue can heal without interference,” said Harris.
Dental lasers can cost from $5,000 to more than $100,000, Reinisch said, and healthcare professionals require extra training to use them. These costs are passed on to the patient, so Reinisch said there must be a definite benefit to the patient to justify these costs.
At least 25% of dental offices in the United States have laser dental capability for periodontal treatment as outlined in the paper, Harris noted, along with other soft-tissue surgical procedures and hard-tissue procedures like the removal of tooth decay. Harris also said that the video simulations demonstrate what happens when lasers hit buried bacterial colonies.
“This is a great way to present to the doctor esoteric scientific findings in a clinically meaningful format,” Harris said. “The model is a great tool for making predictions of what can happen in the tissue. Our study confirms its use as a way to determine the most effective laser parameters to use clinically.”
The study’s methodology of simulating how laser light interacts with tissue has implications beyond dentistry. Physicians and surgeons user lasers in various treatments, including vocal cord procedures and dermatological treatments, including those for toenail fungus. Guided by the results in this study, Reinisch and Harris expect clinical trials will validate their findings.
The study, “Selective Photoantisepsis,” was published by Lasers in Surgery and Medicine.
Related Articles
Researcher Uses Lasers to Regenerate Dental Tissue
Laser Dentistry Requires Bright Practice Management
Use a Laser to Replace a Fractured Solid Zirconia Crown


