INTRODUCTION
Our nation, our world, is facing an epidemic of unhealthy, disturbed sleep. It is not just overweight, middle-aged adults. Sleep issues run through our society.
Three to 12% of children suffer from sleep-disordered breathing (SDB). This encompasses a spectrum of breathing abnormalities that occur during sleep in children. The condition ranges from primary snoring, characterized by noisy breathing without significant airflow obstruction, to more severe forms, such as obstructive sleep apnea (OSA) and central sleep apnea.
Prevalence and Risk Factors
Risk factors for pediatric SDB include obesity, adenotonsillar hypertrophy, craniofacial abnormalities, neuromuscular disorders, and a family history of SDB. It can affect infants and children of all ages. Age or gender does not seem to have any effect on its prevalence in children.
Clinical Presentation
Children with SBD present very differently than adults with sleep disturbances do. Their symptoms can vary depending on the severity of the SDB. Some of the common signs include:
- Snoring or loud, audible breathing
- Restless sleep, thrashing around in their sleep, changing positions, kicking off bed covers, and tangling the sheets.
- Displaying an open mouth posture (mouth breathing) during the day and while asleep
- Choking and gasping for breath during sleep
- Bed-wetting after having stayed dry previously
- ADHD symptoms—becoming hyperactive to help themselves stay awake and alert
- Losing or lacking emotional control, throwing tantrums, acting aggressively, or having frequent meltdowns
- Having night terrors and never growing out of them
- Poor school performance, trouble focusing at school, and difficulty learning as well as retaining new information.
- Behavioral issues and having trouble with social interactions with their peers
Screening and Diagnosis
Screening questionnaires, such as the QOL-18 and Epworth sleepiness scale for children, provide valuable insights into the symptoms the child presents with and the impact it has on his or her daily life as well as those around him or her.
Polysomnography (PSG) is the gold standard for diagnosing pediatric SDB. It monitors various parameters like airflow, respiratory effort, oxygen levels, and sleep stages, along with apneas and hypopneas and the presence of any central events.
Clinical evaluation and detailed medical history play a huge role in identifying potential risk factors and underlying conditions.
A comprehensive evaluation of the shape and size of the upper and lower arches, teeth spacing and alignment, tonsil size, tongue posture, frenum attachments, Mallampatti grade, and shape of the hard palate and soft palate all provide valuable information that can help connect the dots to help identify underlying causes.
This should also include evaluation for the presence of nasal breathing and signs of excessive mouth breathing, acid reflux, tooth grinding, or other disorders.
Impact on Health
Pediatric SDB can adversely affect the growth and development of a child, along with cognitive development and behavior.
Children who are not getting a full night’s sleep may have struggles with growth and development due to lack of adequate deep sleep, which can affect the release of growth hormone. They may struggle with obesity due to the impact on leptin and ghrelin levels, along with cortisol dysregulation. They may wet the bed because of a lack of deep sleep. Without healthy sleep, the body isn’t able to regulate the anti-diuretic hormone to help concentrate urine at night.
Long-term effects of SDB include cardiovascular complications, metabolic disturbances, and neurocognitive deficits. Chronic exposure to cortisol and stress hormones can lead to obesity, type II diabetes, high blood pressure, cardiac issues, chronic pain, and autoimmune problems.
The habitual open-mouthed posture and mouth breathing affect facial development, dental development, and health.
An integrated and multidisciplinary approach involving dentists, pediatricians, sleep specialists, ENTs, myofunctional therapists, and other healthcare professionals is essential for the comprehensive and successful management of these patients.
Early screening and accurate diagnosis, along with appropriate management through tailored treatment plans, are crucial to prevent complications and optimize healthy development and quality of life in affected children.
CASE REPORT
Patient Information
AG was a 6-year-old female who was seen during a routine hygiene exam (Figure 1). Past medical history included allergies, asthma, pneumonia, and tubes in her ears. A QOL-18 questionnaire was filled out by her mom, and it revealed numerous areas of concern related to sleep and behavioral problems. The patient was bottle-fed until age one and used a pacifier until 18 months of age. No thumb-sucking or other habits were reported.

Figure 1. AG was a 6-year-old female who was seen during a routine hygiene exam. Mom reported sleep and behavioral concerns.
Mom reported that AG was a tired child who struggled with morning wakeups. She frequently got into trouble at school for not paying attention and turning in her work on time. She was always tired and grumpy and disliked sports and activities. The patient reported she frequently fell asleep in class because she was tired, and it was hard to focus on what her teacher was saying. She got into frequent altercations with her siblings as well.
When questioned about AG’s sleep habits, Mom reported restless sleep, snoring, and mouth breathing during the day as well as at night. The patient and her mom stated bedtime was 7 pm to 6:30 am and that she usually fell asleep right away. No nightmares or bedwetting was reported.
Physical examination findings included long face (which is concomitant with enlarged adenoids and also known as adenoidal face), narrow nostrils, and chapped lips due to mouth breathing.
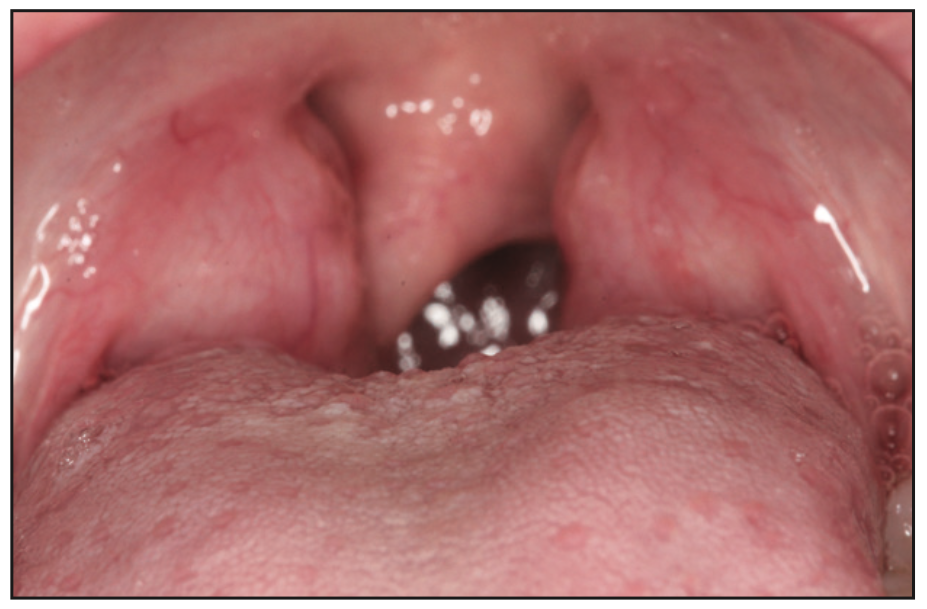
Figure 2. An intraoral exam revealed tonsils that were enlarged and inflamed and contributed to airway obstruction.
An intraoral exam revealed Grade 3 tonsils (Figure 2), narrow buccal corridors, constricted and crowded arches (Figure 3), and insufficient space for permanent teeth. She also had a Class 2 tongue tie along with low tongue posture and a scalloped tongue. The uvula was deviated and enlarged. TMJ examination was WNL.

Figure 3. The intraoral exam showed narrow buccal corridors and constricted and crowded upper and lower arches.
Diagnostic Investigations
The patient was referred to an ear, nose, and throat (ENT) doctor for tonsil evaluation. Diagnostic PSG was done, which resulted in a diagnosis of mild obstructive sleep apnea. Tonsillectomy and adenoidectomy were recommended by the ENT. Imaging studies included x-rays and CBCT scans (Figure 4).

Figure 4. A narrow airway and enlarged adenoids were seen in the preoperative workup.
Some improvement in sleep symptoms was noted, per Mom, after the tonsillectomy and adenoidectomy, but residual OSA was present in a follow-up sleep study that was performed. CPAP was prescribed by a Sleep MD to help manage the residual OSA.
Treatment options were discussed with parents to expand the arches and thus improve the airway. Lingual frenectomy in conjunction with myofunctional therapy was recommended, along with positional therapy and allergy management protocol with the ENT.
Her parents were very concerned about long-term compliance with the CPAP as well as its impact on her growth and development and agreed to proceed with the treatment recommended.
Myofunctional therapy was started, and lingual frenectomy was performed using a DEKA CO2 laser. The patient had 5 sessions of MFT prior to lingual release and 7 sessions following frenectomy.

Figure 5. Airway volume was monitored during the course of treatment.

Figure 6. (a) An upper fixed Schwarz expander with lap springs was used to expand the upper arch and direct growth. (b) A lower fixed Schwarz expander was used for the lower arch to help upright posterior molars and create space and help direct growth.

Figure 7. Upper-arch shape and form was improved once expansion was finished. A wider, U-shaped palate allowed for adequate space for eruption of permanent teeth.

Figure 8. Lower-arch form and shape was improved once expansion was completed. Mandibular molars were uprighted, and there was adequate space for the permanent teeth to erupt.

Figure 9. Increased airway volumes were noted on CBCT after expansion was completed.
Expansion of arches was done using upper and lower fixed Schwartz expanders. During the course of treatment, CBCT scans were done to monitor airway volume using Excelsior (PreXion) (Figures 5 and 6). The airway volume increase was noted as arches were expanded. The patient and her mom also reported improvement in symptoms (Figures 7 to 9).
CONCLUSION
An integrated approach involving pediatricians, sleep specialists, ENT surgeons, and other healthcare professionals is essential for comprehensive management. Early diagnosis and appropriate management are crucial to prevent complications and optimize a child’s health and quality of life.
In conclusion, pediatric SBD encompasses a range of breathing disturbances during sleep in children. Early recognition, accurate diagnosis, and tailored treatment plans can significantly improve outcomes and promote healthy development in affected children.
ABOUT THE AUTHOR
Dr. Dassani is an internationally educated dentist practicing in Houston. She received her initial dental training from the University of Mumbai in 1996. She operated a successful dental practice in Mumbai for 6 years before moving to the United States. She is a 2005 graduate of the Boston University Goldman School of Dental Medicine, where she was actively involved in research projects. She also enjoyed working in communities surrounding the dental school. She has been practicing in Houston for the last 18 years. She has a passion for providing patients with the highest quality of care that will benefit their overall health. Screening and treatment of obstructive sleep apnea in children as well as adults is an integral part of her practice. Her vision and goal for herself and her team is to help patients with sleep-disordered breathing get the treatment they need to live healthier, happier lives. She can be reached at dassanidentistry.com.
Disclosure: Dr. Dassani reports no disclosures.











