INTRODUCTION
This article will explore different approaches to the restoration of a Class II cavity preparation based on clinical parameters and discuss techniques and material choices that will help to maximize results and restoration longevity.
Clinical Parameters for Restorative Material Selection
For most general practitioners, direct composite restorations play a major role in their work every day. Many clinicians have a favorite material or technique that is universally applied to all clinical situations. Given the variety of patients and clinical issues that present, it is important that each clinician prescribes the restorative material that is best suited for each clinical situation!
When dental amalgam was the only direct restorative material being used, placement protocols were uncomplicated. Since the introduction of composite resin, these materials have been largely treated like amalgam as far as placement technique is concerned, “condensing” or “packing” the material into a cavity preparation like their metallic predecessors. Amalgam was described by some as “self-sealing” because of corrosive biproducts that developed over time at the marginal interface.1 However, composite depends upon acid etching and bonding (with adhesives) to seal the tooth-restorative interface. Because of this, there is a real clinical potential for failure because these 2 materials are so different. Amalgam is not very technique sensitive, and it condenses well into geometric cavity preparations. On the other hand, composite resin is very technique sensitive, requiring many steps that must be followed precisely to optimize results.
Clinical parameters that can impact the quality of placement of a bonded composite restoration include (1) moisture (saliva, blood, or crevicular fluid), (2) margin location (supragingival, equigingival, or subgingival), (3) availability of enamel at the cavosurface margins, (4) the ability to seal the gingival cavosurface margin with a matrix and wedge, and (5) the quality of the proximal contour and contact with the adjacent tooth.2
For the reasons stated above, the chance for clinical failures with composites is often regarded as being greater than with amalgam, with one study quoting the average life of a posterior composite at only 5.7 years.3
Bonding to Enamel and Dentin
Many consider the adhesive bond to etched enamel to be the strongest bond in dentistry. Since the concept of enamel etching and the use of resin adhesive technology have been introduced to dentistry, they have been widely considered to not only help in the retention of dental restorative materials to tooth structure but also to help act as a deterrent to micro-leakage and bacterial penetration. On the other hand, the bond to dentin is not always considered to be as strong or predictable. Many factors, such as those mentioned above, can significantly affect the ability to predictably bond to dentin.
One of the best and well-kept secrets currently in adhesive dentistry is the use of glass ionomer cements as a useful adjunct in the restorative process. Glass ionomers, since their discovery, have been one of the most widely researched of all dental materials. In many countries, they are the restorative material of choice due to their low cost and anticariogenic properties. According to Ngo et al,4,5 glass ionomer cement forms a “chemically fused seal to dentin” that many will argue is superior to dentin adhesive technology, especially when enamel is absent. It has been argued that the dentin bond hydrolyzes with time, allowing microleakage and recurrent caries to occur. In deeper excavated areas close to the dental pulp, Class V cervical areas, sclerotic dentin, and deep Class II proximal boxes without an “enamel rim,” glass ionomer technology can affect a better seal than bonded composite; this is especially true when dealing with the clinical challenges of the microenvironment. Also, it is important to note that the coefficient of thermal expansion (CTE) of glass ionomer cement is the same as dentin, so it expands and contracts at the same rate. Based on this discussion, after cavity preparation and isolation and prior to restoration, it is first important to determine (1) the ability to isolate the cavity preparation from moisture based on access and margin position; (2) the extent and depth of the preparation based on caries excavation; and (3) if a peripheral border of enamel exists completely around all margins of the cavity preparation, including the gingival margin of the proximal box(es). An important clinical distinction that needs clarification is that there is “good” dentin and “not-so-good” dentin to bond to. Dentin close to the dentinoenamel junction has fewer dentinal tubules per square millimeter and, therefore, more peritubular dentin to demineralize through the acid-etch process, yielding higher bond strengths.
Deeper, excavated areas close to the dental pulp, Class V cervical areas, sclerotic dentin, and deep Class II proximal boxes without an enamel rim are areas where the dentin bond does not perform well, leading to the possibility of recurrent decay and marginal failure of the restorative material. It is important as a clinician to differentiate between “good” and “bad” dentin when choosing a material to close this tooth-restorative interface. It is well accepted that glass ionomer cements seal bad dentin better than dentin bonding systems. In areas of good dentin, dentin adhesives perform very well.6
Until now, the delivery and manipulation of glass ionomer cements has been a clinical challenge. With the recent introduction of Fuji Automix LC (GC America), the routine use of glass ionomer materials in restorative dentistry has been made easier than ever before. Now these materials can be delivered into the cavity preparation without having to hand-mix or triturate them. Syringe delivery and precise placement make the use of this dentin replacement seamless with composite use.
CASE REPORTS
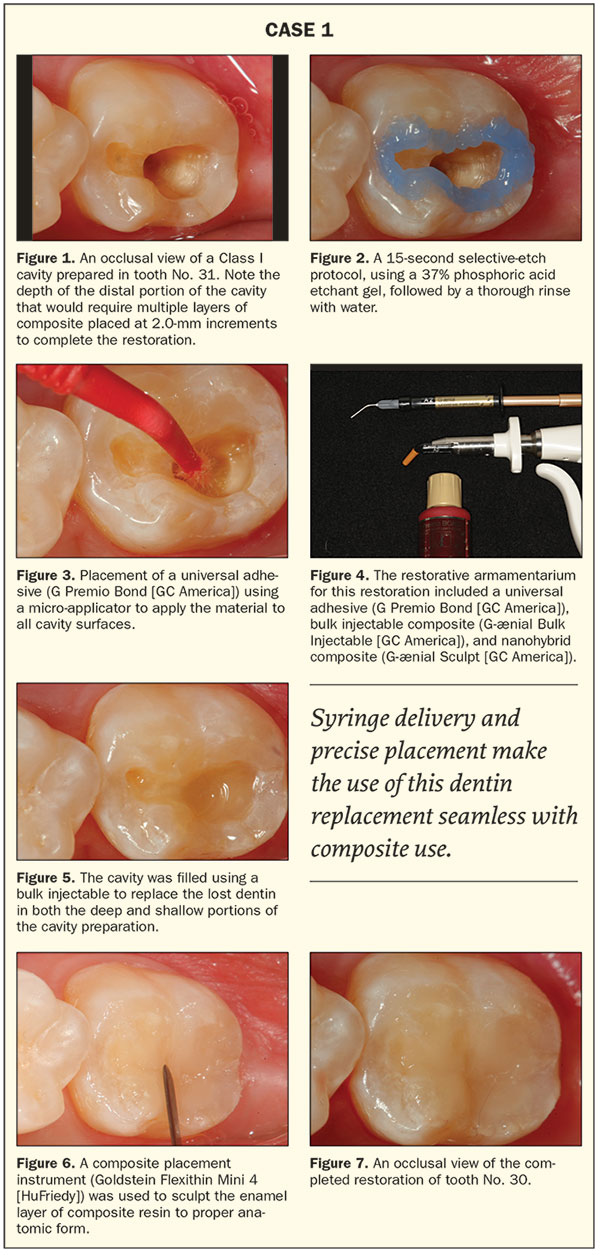
Case 1
Direct Composite Restoration/Shallow to Medium Depth/Enamel on All Cavosurface Margins
Figure 1 shows a Class I cavity preparation on tooth No. 30. The previous restoration and base had extended pulpally in the distal aspect of the preparation. Since the distance from the preparation floor in that area to the cavosurface margin is greater than 2.0 mm, it will take more than one increment of composite to restore it. One way to decrease the number of increments required and save placement time is to use a bulk-fill flowable composite (G-ænial Bulk Injectable [GC America]) as a “dentin” replacement. According to manufacturers, this type of flowable composite can be placed in 4.0-mm increments, cutting the number of increments of traditional composite required to fill a deeper cavity preparation in half. A selective-etch protocol was used. The enamel of the cavosurface margin was etched for 15 seconds using a 37% phosphoric acid etchant gel (Select Etch HV [BISCO Dental Products]) (Figure 2). After rinsing the etchant off thoroughly and then removing the excess moisture with a high-volume
suction, a universal adhesive (G Premio Bond [GC America]) was applied to all surfaces of the cavity preparation (Figure 3). Once the adhesive was light cured, the bulk injectable composite was placed to the depth approximating the dentinoenamel junction (Figures 4 and 5). Once the “dentin replacement” was light cured (VALO Grand [Ultradent Products) per the manufacturer’s instructions, a nanohybrid composite “enamel layer” (G-ænial Sculpt [GC America]) in the appropriate shade was placed, and the occlusal anatomy was then sculpted using a composite placement instrument (Goldstein Flexithin Mini 4 [HuFriedy]) (Figure 6). Figure 7 shows an occlusal view of the completed composite restoration in tooth No. 30 after the light curing and all the finishing/polishing steps were done.
 |
Case 2
Direct Composite Restoration/Deep Excavation/Enamel on All Cavosurface Margins (Closed Sandwich)
The patient shown in Figure 8 presented with an old Class I amalgam that had decay on the mesial proximal surface. A fracture line can also be seen radiating from the restorative material, across the mesial marginal ridge, and down the proximal surface near the palatal portion of the proximal contact. After removal of the restorative material and associated decay and preparation of the proximal cavity form, the operative area was isolated with a rubber dam (Figure 9) in preparation for the restorative process. Due to the depth of the preparation, a glass ionomer base (Fuji II LC Automix [GC America]) was placed (Figures 10 to 12). The potential for remineralization using glass ionomer cements in preparations close to the dental pulp is well documented by McLean et al7 and others.8-10 An appropriate sectional matrix band (Composi-Tight Gold [Garrison Dental Solutions]) was chosen that best corresponded anatomically to the tooth being restored and also to the width and height of the proximal surface. The height of the sectional matrix should be no higher than the adjacent marginal ridge when properly placed. Because of the concave anatomic shape, the proximal contact was located approximately 1.0 mm apical to the height of the marginal ridge. Next, the gingival portion of the band was stabilized and sealed against the cavosurface margin of the preparation using the appropriate-size flexible wedge (Garrison Dental Solutions).
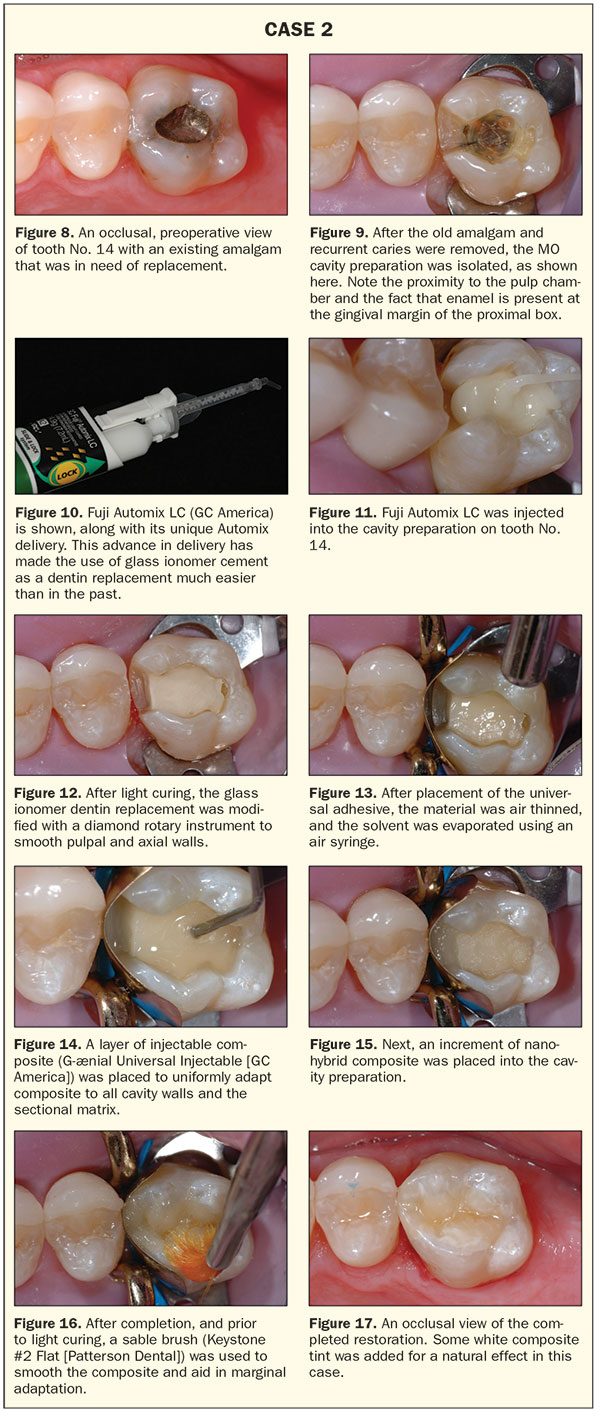 |
Since enamel surrounded the entire periphery of the preparation, including the gingival box preparation, a flowable composite (G-ænial Universal Bulk Injectable [GC America]) was used to fill that area of the cavity preparation. A 15-second etch was performed using a 37% phosphoric acid gel. The etchant was then rinsed off for a minimum of 15 to 20 seconds to ensure complete removal. Next, a universal bonding agent (G Premio Bond) was placed on all cavity surfaces (Figure 13) and light cured for 20 seconds. As mentioned, the first step was to fill the proximal box using a flowable composite (G-ænial Universal Injectable) to approximately the level of the pulpal floor (Figure 14). Because of its lower viscosity, the flowable composite uniformly adapted into all the intricate areas of the proximal box, thus ensuring precise marginal adaptation. After light curing for 20 seconds, the next step was to layer in the nanohybrid material (Figure 15). First, using a unidose delivery, the facial increment of nanohybrid composite (G-ænial Sculpt) was placed into the cavity preparation and sculpted to anatomic form. A palatal increment of nanohybrid composite was placed, sculpted (a soft sable brush was used to smooth the sculpted surfaces [Figure 16]), and then light cured in the same manner as previously described. After the light curing step was completed, the matrix band was removed, and the occlusion was checked with articulation paper and adjusted as needed using a carbide-finishing bur (FS3 [Komet USA]). When placing composite materials using this technique, very little finishing should be required, except at the marginal areas. Low-speed rubber polishing abrasives (A.S.A.P. polishers [CLINICIAN’S CHOICE Dental Products]) were used to further polish the surface of the restoration. Figure 17 shows an occlusal view of the completed Class II composite restoration.
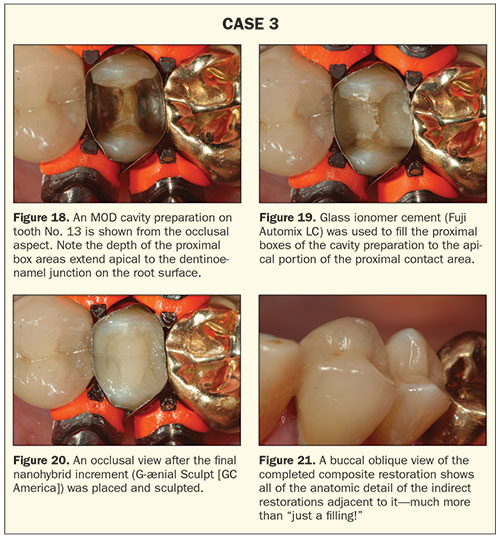
Case 3
Direct Composite Restoration/Any Depth/Little-to-No Enamel at the Cavosurface Margins of the Proximal Box (Open Sandwich)
Figure 18 shows an occlusal view of tooth No. 13 of a 73-year-old patient after the removal of an old amalgam and associated recurrent decay. The gingival floors of the previous restoration extended beyond the cementoenamel junction in the proximal box areas onto root surfaces. This is not a good place to rely on adhesives to seal the margin. As mentioned, glass ionomer cements, according to Ngo et al,4,5 forms a “chemically fused seal” to dentin; therefore, an open sandwich technique using glass ionomer cement (Fuji AutoMix LC) is a good choice to protect these vulnerable areas using a nanohybrid composite (G-ænial Sculpt) as the final “enamel” layer for strength and durability against the forces of occlusion. Also, glass ionomer cement at the marginal interface of a Class II restoration will provide protection from recurrent caries by virtue of fluoride release and remineralization.11 Figure 19 is an occlusal view of the cavity preparation after placement of glass ionomer cement into both proximal boxes of this MOD cavity preparation. The glass ionomer cement can be placed up to the gingival portion of the proximal contact area. The final nanohybrid composite increment restored the proximal contacts and occlusal surface of the restoration (Figure 20). A buccal oblique view (Figure 21) of the completed restoration shows the anatomic form of the adjacent ceramic and gold crowns as well as the completed composite restoration. (Note the attention that was paid to the replication of natural tooth anatomy in all 3 types of restorations.)
 |
CLOSING COMMENTS
Different approaches to restoring a Class II cavity preparation have been described. It should be remembered that every clinical situation is different regarding the amount of enamel and the quality of dentin present after decay removal. Each situation should be evaluated on its own merits, and then the appropriate protocol must be used to ensure the best long-term clinical result.
References
- Bharti R, Wadhwani KK, Tikku AP, et al. Dental amalgam: an update. J Conserv Dent. 2010;13:204-208.
- Kugel G, Ferrari M. The science of bonding: from first to sixth generation. J Am Dent Assoc. 2000(suppl 131):20S-25S.
- Tezvergil-Mutluay A, Agee KA, Hoshika T, et al. The inhibitory effect of polyvinylphosphonic acid on functional MMP activities in human demineralized dentin. Acta Biomater. 2010;6:4136-4142.
- Ngo HC, Fraser M, Mount G, et al. Remineralisation of artificial carious dentine exposed to two glass-ionomers. Presented at: 2002 IADR/AADR/CADR General Session; March 9, 2002; San Diego, CA. Abstract 3109.
- Ngo HC, Fraser M, Mount G, et al. Remineralization of carious dentin by glass ionomer, an in-vivo study. Presented at: 2001
IADR General Session; June 29, 2001; Chiba, Japan. Abstract 0919. - Munck J, Van Meerbeek B, Satoshi I, et al. Microtensile bond strengths of one- and two-step self-etching adhesives to bur-cut enamel and dentin. Am J Dent. 2003;16:414-420.
- McLean JW, Powis DR, Prosser HJ, et al. The use of glass-ionomer cements in bonding composite resins to dentin. Br Dent J. 1985;158:410-414.
- Mount GJ. Clinical placement of modern glass-ionomer cements. Quintessence Int. 1993;24:99-107.
- Christensen G. Glass-ionomer-resin restorations. Clin Res Assoc Newsletter. 1992;16:l-2.
- Mount GJ. Clinical requirements for a successful ‘sandwich’—dentine to glass ionomer cement to composite resin. Aust Dent J. 1989;34:259-265.
- Botelho MG. Inhibitory effects on selected oral bacteria of antibacterial agents incorporated in a glass ionomer cement. Caries Res. 2003;37:108-114.
Dr. Lowe received his DDS degree from the Loyola University School of Dentistry in 1982. He previously taught at the Loyola University School of Dentistry while building a private practice in Chicago. Dr. Lowe currently maintains a full-time practice in Charlotte, NC. He can be reached via email at boblowedds@aol.com.
Disclosure: Dr. Lowe receives an honorarium from GC America.
Related Articles
Complete Oral Rehabilitation: A Case Report: Using a Combined Surgical/Ceramic Approach
The Bulk-Fill Class II Composite Restoration
Focus On: Bioactive Dental Materials


