INTRODUCTION
Bone quality plays a factor with initial implant stability in immediate or delayed approaches. Implant placement in the maxilla frequently requires some site manipulation to accommodate the implant. Bone width deficit can be due to resorption in the buccal-lingual direction related to either periodontal issues with a tooth when immediate placement is planned or following healing of a prior extraction site. Bone quality due to lower density is typical of the maxilla and is usually D3 or D4 in nature.
Bone density on standard radiographs is an individual perception and equated with visual shades of gray in the planned site. Cone-beam computed technology (CBCT) offers a more accurate, repeatable evaluation of bone density and is measured by typical software in Hounsfield units (HU). An HU reading of less than 200 (Lekholm and Zarb classification) equates with type D4 bone, indicating poor-density bone, whereas type D3 bone is greater than 200 HU and less than 400 HU.1 The distribution in the maxilla, having less bone density then the mandible, typically presents with D3 bone in the premaxilla and D4 in the posterior maxilla.2 However, factors may lead to a decreased bone density in the premaxilla equaling the D4 bone found posteriorly.
CBCT evaluation can provide a more accurate assessment during planning stages so that site modification may be included during surgical placement of the implants to improve the density of the bone in contact with the implant, increase insertion torque, and yield better load distribution when the implant is brought into function with prosthetic placement.3
 |
 |
| Figure 1. The anterior VGO (Variable Geometry Osteotomes) osteotome kit (Helmut Zepf Medizintechnik GmbH, H&H Company) with threaded straight tips and accessories in a sterilizer cassette. | Figure 2. The anterior VGO threaded straight osteotome tips in increasing diameter. |
Implant stability, both at placement and during function, relates to the density of the surrounding bone. The accepted goal at placement is to have sufficient insertion torque, even when immediate loading is not planned, so that the implant can integrate without the potential for micromovement in the surrounding bone. Improvement in the bone quality (density) has been documented as a clinical advantage to primary stability, specifically in D3 and D4 bone found in the maxilla.4,5
The use of osteotomes to improve bone quality at implant sites has been reported over an extended time in the literature. Summers6 reported on it in 1994, as well as Hahn7 in 1999, Garg8 in 2002, and many others over the past several decades. The initial osteotomes were hand instruments that were placed at the site and force exerted with a surgical mallet to advance the instrument to the planned depth while laterally compressing the bone to improve the density and expand the ridge width when desired. Some negative issues, unfortunately, may occur when a mallet is used to drive the osteotome apically, both from a patient-comfort aspect and a potential-surgical-error standpoint. The malleting is amplified cranially from a sound and sensation standpoint, and, although patients are anesthetized, they often do not like those sensations. Additionally, there is the potential that the osteotome diverges from the intended path, disrupting the surrounding bone as it is impacted with the mallet. As the lingual (palatal) plate is denser bone than the buccal (facial), if loading of the osteotome diverges from the intended path, either by misdirection of the mallet or contact with the denser bone of the palate, fracture of the facial plate may occur. This frequently leads to aborting the planned implant placement, as little to no initial stability would be present, should the implant be inserted, and a lengthening of treatment time, allowing the site to heal before another attempt is made.
 |
 |
| Figure 3. (a) VGO handle and crossbar (b) with crossbar held magnetically (c) to allow rotational torque with the threaded tip in the handle’s chuck. | Figure 4. The offset, non-threaded VGO tips are available for posterior applications. |
 |
| Figure 5. A precision pilot tip (top) and an immediate implant placement marker tip (bottom) is utilized before site initiation to create a purchase point for the pilot drill. |
Rotary handpiece-driven osteotomes have been available for an extended period of time. These were introduced to eliminate the patient sensation with mallet-driven osteotomes and give the operator more tactile control at the site. They do offer improved side control but have the potential for heat generation where the rotating instrument contacts the bone at the site.9 Heat generation at the bone interface may potentially hamper or prevent osseointegration related to the destruction of osteogenic cells. This has greater potential in the denser bone of the mandible than in the maxilla but may occur if excessive pressure is placed on the drill to advance it. It is well accepted that heat generation has negative consequences in implant integration and should be minimized to prevent destruction of osteogenic cells at the bone-implant interface.10 Hand osteotomes have the benefit of no heat generation found during the use of rotary osteotomes, but, as discussed, they have other issues that are eliminated with rotary osteotomes.11
So, what is the solution?
The VGO Concept
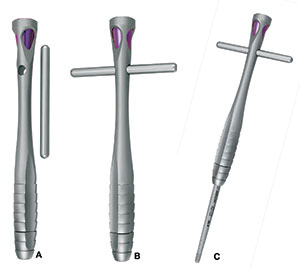
The VGO (Variable Geometry Osteotomes) instruments (manufactured by Helmut Zepf Medizintechnik GmbH in Germany and distributed by H&H Company) are designed for optimal heatless lateral condensation without the potential of crestal bone overloading when using the instruments while increasing practitioner tactile feedback. The system is provided as an anterior or posterior kit in a sterilizable cassette (Figure 1). The anterior tips are threaded to 8 mm and labeled from 0 to 6 mm with depth marks at 8, 10, 13, and 16 mm (Figure 2). Each kit contains 2 handles with a magnetic crossbar. VGO tips are interchangeable (Figure 3). The crossbar can increase torque in denser bone situations. The posterior VGO tips are sized from 1 to 8, non-threaded, and offset, with depth marks at 5, 8, 10, 13, and 16 mm
(Figure 4). These are designed for posterior use when straight line access is not possible with the anterior tips. Their intended purpose is for crestal sinus elevation and/or densification. They can be used in conjunction with rotary crestal sinus elevation kits and with light malleting action. They are also non-threaded. The anterior tips are advanced in a clockwise motion until reaching the planned depth, then counter rotated to remove. When the anterior tips are utilized and bone density is hampering full advancement, recalibration with a rotary device (pilot drill) may be suggested.
 |
 |
| Figure 6. The precision pilot tip (left) is used to create a purchase point for the initial VGO osteotome, and, when the implant placement angle requires correction from the angulation of the socket, the curved implant placement marker tip creates a purchase point on the socket wall to redirect the osteotomy with the VGO osteotome tips (right). | Figure 7. Comparison of the differences between the Delta-1 and Delta-2 VGO tips and where they actively create osseocompression on the tips’ shaft. |
 |
 |
| Figure 8. Radiograph of a fractured maxillary right premolar with a buccal and lingual root. | Figure 9. A radiograph was taken with the implant pilot drill to verify positioning in relation to the adjacent teeth and floor of the sinus. |
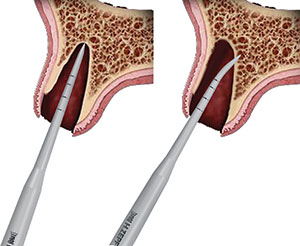
Precision pilot tips are provided in both kits and are available both straight and curved and with depth marks at 8, 10, 13, and 16 mm (Figure 5). These 2 tips are utilized to create a purchase point for the pilot drill when necessary. Lateral slippage of pilot drills often occurs due to the cortical bone that lines most sockets. The straight precision pilot tip is designed when the osteotomy will follow the extraction socket (Figure 6, left), and the curved precision pilot tip is utilized when redirection of the osteotomy is required from the path of the extraction socket (Figure 6, right).
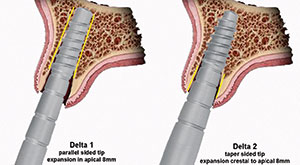
Traditional osteotomes that are used for the Summers-type approach feature a continuous taper and typically apply forces at the thin crest that can often cause overstress and fracture the crest, especially when using them to less than maximal depth of the tips. This can have the potential of overstressing the delicate buccal crestal bone, leading to fracturing or resorption during healing after implant placement. The VGO osteotomes utilize a different concept called passive wave dilation, using a stepped tip escalation formula (Figure 7). Both kits are composed of either Delta-1 tips or Delta-2 tips. They work at opposite poles of the osteotomy and become active at the 8-mm mark and where dilation begins. The Delta value indicates to the surgeon what portion of the osteotomy is being dilated. Delta-1 tips feature half the taper of their Delta-2 counterparts. Delta-1 tips progressively dilate the apical (deep bone), and Delta-2 dilates the crestal area from within. The result is a deep wave dilation from within, providing the benefit of decreased crestal stress.
The axis of rotation of the bony plates is moved deeper with the additional advantage of passive entrance into the osteotomy. The threaded tips of the anterior kit drive the tips in and additionally create micro-serrations, which increase bleeding. This, in effect, leads to more growth factors being present at the bone-to-implant interface due to the degranulation of platelets (activated state). Both kits feature the Delta Dot above or below the instrument to allow the clinician to know at a glance where exactly the tip will do work, namely at the deep apical bone or the surface crestal bone. Tip-0 from the anterior kit is uniquely marked with a dot above and below to indicate that it may be fully active, depending on the diameter of the generic pilot drill the surgeon has used.
To attain the best results, it is recommended that each case be initiated with a standard pilot osteotomy to intended full depth, followed by Tip-0, Tip-1, and so forth, until the desired osteotomy size is achieved, depending on the planned implant fixture. The sequence is continued, alternating between Delta-1 and Delta-2 tips until reaching a width that is less than the intended diameter of the implant being placed. The implant being placed completes the osseocompression as it is inserted to achieve a higher insertion torque.12 When the initial bone density is D4, undersizing the osteotomy by a minimum of 1.5 to 2.0 mm is suggested to improve the insertion torque. Achieving sufficient primary implant stability in poor-quality bone is difficult. Other than for conventional osteotomes, little is known about the effectiveness of screw-shaped spreaders in condensing bone and increasing primary stability. Therefore, implant stability quotient (ISQ) measurements of implants placed in bone-surrogate models were conducted. Bony microarchitecture had no effect on implant stability, but initial bone density, presence of a cortical layer, and the use of screw-shaped spreaders significantly increased ISQ levels.
CASE REPORT
A 64-year-old male patient with an unremarkable medical history presented with a maxillary first premolar that required extraction related to vertical root fracture (Figure 8). Informed consent was obtained following discussion of clinical findings and recommended treatment.
 |
 |
| Figure 10. The No. 1 anterior VGO osteotome was utilized in the lingual root space to expand the root geometry to accommodate implant placement. | Figure 11. Site preparation continued with the No. 3 anterior VGO osteotome following the No. 2 osteotome. |
 |
 |
| Figure 12. Site preparation was completed with the No. 4 anterior VGO osteotome. | Figure 13. The implant was placed into the osteotomy using a surgical handpiece, engaging the implant driver. |
Local anesthetic (4% Articaine with 1:100,000 epinephrine [Dentsply Pharmaceuticals]) was administered. A sulcular incision was made using a No. 15 scalpel blade, starting at the distal buccal of the second premolar and continuing to the distal papilla of the canine. A vertical releasing incision was made, sparing the canine papilla, an
d a full-thickness flap was elevated on the buccal. Short vertical releasing incisions were made on the palatal, sparing the papilla, and a sulcular incision was created. The tooth was atraumatically extracted, and a radiograph was taken to verify that no residual root fragments remained. As the premolar extraction socket had separate buccal and palatal root spaces, implant placement was planned for the palatal root space to center the implant under the prosthetic crown that would be placed for ideal loading vectors. This placement would also allow greater osseous thickness after healing on the buccal, thereby aiding in its long-term preservation under function.
 |
 |
| Figure 14. The implant was then placed into the lingual root space that had been expanded using the anterior VGO osteotomes to preserve bone and improve osseous density. | Figure 15. The buccal root space was filled with graft material, which was then condensed into any voids from the extraction. |
 |
 |
| Figure 16. As the site cannot be closed by primary closure, a piece of non-resorbable membrane was placed under minimally elevated flap margins to cover the implant and graft material. | Figure 17. Sutures were placed to secure the membrane. |
 |
| Figure 18. Radiographs show the implant (a) at placement; (b) 4 months later with the impression abutment in place; and, finally, (c) restored with a custom abutment and cemented crown. |
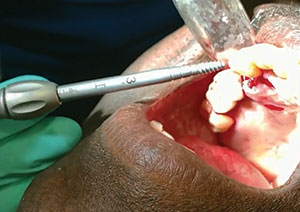
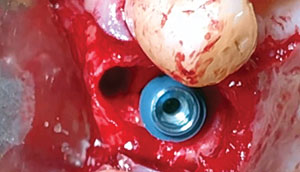
A pilot osteotomy was done with a generic pilot drill toward the palatal root space to a depth of the osteotomy. It corresponded to the previously selected implant length based on radiographic planning (Figure 9). The Tip-0 was then utilized into the pilot hole to the determined depth. Site preparation continued with the Tip-1 (Figure 10). The remainder of the osteotomy continued with sequential use of the remaining tips (Figure 11). Osteotome preparation of the site continues with larger VGO osteotomes until the site is narrower than the planned implant and the implant insertion will complete the lateral osseous condensation. In this case, VGO osteotome preparation was completed with the No. 4 tip (Figure 12). As planned, a 5.0- × 13-mm implant (AnyRidge [integrated dental systems]) was inserted into the osteotomy created with the VGO instruments to the correct depth using the surgical handpiece, followed by a manual wrench (Figure 13).
The implant was positioned into the palatal root socket, leaving a void in the buccal root socket (Figure 14). To aid in preservation of the easily resorbable buccal crestal bone, the socket void was filled with Irradiated Cancellous bone (Rocky Mountain Tissue Bank) to the crestal level (Figure 15). Since a large crestal gap was present due to an inability to get primary closure, a membrane was required to cover the osseous graft material just placed. A piece of Cytoplast TXT-200 nonresorbable membrane (Osteogenics Biomedical) was placed, tucking its edges under the previously elevated buccal and palatal soft-tissue flap margins (Figure 16). Also, 4-0 vicryl sutures (Ethicon) were placed in an interrupted pattern over the membrane to secure the flap margins in place and prevent disruption of the underlying graft and overlying membrane (Figure 17). A radiograph was taken to document the implant placement into the site, and the patient was dismissed to allow healing and osseointegration before the restorative phase began (Figure 18a).
Following 4 months of healing to allow integration of the implant and graft material, the restorative phase was initiated with uncovery of the implant and the taking of a closed-tray impression (Figure 18b). Restoration was completed with a custom abutment and a cemented crown (Figure 18c).
IN SUMMARY
The maxillary arch presents with less dense bone than found in the mandible and, thus, has less load-handling potential due to the density difference. Manipulation of the bone through osseous condensation with osteotomes improves that bone density to allow better load handling and long-term bone maintenance when compared to sites that have not had osseocompression performed. As discussed, the VGO osteotomes eliminate some of the issues with traditional osteotomes that require a mallet to advance the tip or have the potential for heat generation, as reported with rotary osteotomes. Furthermore, these instruments provide a better tactile feel for the practitioner, allowing for a better guided approach based on the site’s anatomy, along with improved safety.
References
- Sogo M, Ikebe K, Yang TC, et al. Assessment of bone density in the posterior maxilla based on Hounsfield units to enhance the initial stability of implants. Clin Implant Dent Relat Res. 2012;14(suppl 1):e183-e187.
- Truhlar RS, Orenstein IH, Morris HF, et al. Distribution of bone quality in patients receiving endosseous dental implants. J Oral Maxillofac Surg. 1997;55(12 suppl 5):38-45.
- Hao Y, Zhao W, Wang Y, et al. Assessments of jaw bone density at implant sites using 3D cone-beam computed tomography. Eur Rev Med Pharmacol Sci. 2014;18:1398-1403.
- De Vico G, Bonino M, Spinelli D, et al. Clinical indications, advantages and limits of the expansion-condensing osteotomes technique for the creation of implant bed. Oral Implantol (Rome). 2009;2:27-36.
- Petrov SD, Drew HJ, Sun S. Sequencing osteotomes to overcome challenges presented by deficient bone quantity and quality in potential implant sites. Quintessence Int. 2011;42:9-18.
- Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:152-162.
- Hahn J. Clinical uses of osteotomes. J Oral Implantol. 1999;25:23-29.
- Garg AK. The use of osteotomes: a viable alternative to traditional drilling. Dent Implantol Update. 2002;13:33-40.
- Mishra SK, Chowdhary R. Heat generated by dental implant drills during osteotomy—a review. J Indian Prosthodont Soc. 2014;14:131-143.
- Chauhan CJ, Shah DN, Sutaria FB. Various bio-mechanical factors affecting heat generation during osteotomy preparation: a systematic review. Indian J Dent Res. 2018;29:81-92.
- Baptist BA. Clinical applications of an atraumatic osteotome. Compend Contin Educ Dent. 2017;38:538-543.
- Kreissel P, Kölpin F, Graef F, et al. Effect of rotating osteotomes on primary implant stability—an in vitro investigation. J Oral Implantol. 2013;39:52-57.
Dr. Krastev graduated from New York University (NYU) in 1993 and was appointed as assistant professor in CAPPA. In 2004, after completing a 2-year implant training at NYU, he was invited to serve as a clinical assistant
professor and was on faculty until 2016, teaching in the implant training program. He has developed and patented multiple dental products and maintains a private practice in New Hyde Park, NY. He can be reached at pkrastev@aol.com.
Dr. Kurtzman is in private general practice in Silver Spring, Md. A former assistant clinical professor at the University of Maryland, he has earned Fellowships in the AGD, the American Academy of Implant Prosthodontics, the American College of Dentists, the International Congress of Oral Implantologists (ICOI), the Pierre Fauchard Academy, and the Association of Dental Implantology; Masterships in the AGD and ICOI; and Diplomate status in the ICOI and the American Dental Implant Association. He has lectured internationally, and his articles have been published worldwide. He has been listed as one of Dentistry Today’s Leaders in Continuing Education since 2006. He can be reached via email at dr_kurtzman@maryland-implants.com.
Dr. Garg is a nationally recognized dental educator and surgeon who, for more than 20 years, served as a full-time professor of surgery in the department of Oral and Maxillofacial Surgery and as director of residency training at the University of Miami Leonard M. Miller School of Medicine. Dr. Garg is considered the world’s preeminent authority on bone biology, bone harvesting, and bone grafting for dental implant surgery. He is a well-known lecturer and has authored 9 published textbooks and a dental implant marketing kit that have been translated into multiple languages and distributed worldwide. He can be reached at arun.implantseminars@gmail.com.
Dr. Radwan graduated from the Columbia University College of Dental Medicine in 1990 and was a clinical instructor there for more than 10 years. He maintains a private practice in New York City.
Dr. Frawley earned both his undergraduate and dental degrees from the University of California, Los Angeles (UCLA). He has been practicing dentistry in Beverly Hills, Calif, since 1981. He has been grafting and placing implants since 1982. He taught at UCLA for 15 years. Dr. Frawley started Surgical Esthetics, a regenerative company in 2011. He has been teaching grafting and implants both nationally and internationally for the past 8 years.
Disclosure: The authors report no disclosures.
Related Articles
Hard-Tissue Laser Applications: Optimizing Restorative Treatment
Management of Oral Viral Lesions With a Diode Laser
A Guidance System for the Partially Edentulous Arch



