INTRODUCTION
Replacement of incisors is a huge challenge for clinicians, technicians, and even patients, and although the advancements in dental implants and techniques made outcomes more predictable, proper management of the soft tissues and patients’ acceptance of results are still not guaranteed.1 Moreover, patients facing the loss of their teeth may experience apprehension toward losing their social image or daily function. Hence, patients often expect to have their implants restored with a fixed prosthesis similar to their natural dentition much earlier during the treatment phase.2 The preparation of aesthetically appealing and anatomically correct implant-supported provisional restorations facilitates the fabrication of the final implant-supported crown. The provisional restoration molds and manipulates the soft tissue while acting as a blueprint or template for the final crown.3 The emergence profile of the provisional restoration passes through stages of different forms. The first stage is concave to give space for the gingival tissues to grow in thickness.4 Later, resin material is added to exert some pressure on definite positions to move the gingival tissues to the desired levels. The soft-tissue form and position are stabilized, and the final provisional emergence profile form should be properly recorded. This is transferred to the dental laboratory for duplication to the final restoration.5 Immediately after removal of the provisional restoration, the peri-implant soft tissues begin to remodel into a flatter gingival architecture resembling that of an edentulous site. If no attempt is made to halt the soft-tissue remodeling when the provisional restoration is removed, the resulting cast will not accurately represent the soft-tissue contours around the provisional restoration,5 not to mention the challenges facing the ceramist in accurately reproducing hue, chroma, value, surface characterization, translucency, opacity, surface gloss, and internal as well as external characterizations.6
CASE REPORT
Chief Complaint and Addressing Challenges
A 28-year-old female patient presented to the Fixed Prosthodontics Department clinic in the Faculty of Dentistry at Ain Shams University in Cairo, Egypt, with missing tooth No. 9 that, due to a traumatic accident years ago, had been restored with an acrylic removable partial denture. She requested replacing the removable prosthesis with the most conservative fixed solution.
The clinical examination, radiographs, diagnostic casts, and photographs revealed a reduction in mesiodistal width of the edentulous space compared to tooth No. 8, a high lip-line, buccal hard- and soft-tissue defects, and challenging shades and textures of neighboring teeth (Figure 1). A CBCT scan confirmed the bone deficiency findings.

Figure 1. Preoperative photos. (a) The frontal and (b) occlusal view show the decreased mesiodistal width of the edentulous space of the missing upper left central incisor and the high lip-line of the patient.
Treatment Planning
After consultation with the surgeon, 3 options for restoration were presented. A dental implant, a resin-bonded bridge, and a fixed partial denture were clearly discussed, along with the pros and cons of each. She chose the grafting and implant solution as she didn’t want to sacrifice any sound tooth structure of the adjacent teeth. A diagnostic aesthetic wax-up for tooth No. 9 was created to be used later for prosthetic implant placement and provisionalization. An autogenous bone block graft from the patient’s mandible was used to increase the buccolingual dimension of the ridge (Figure 2). After 4 months, an implant (3.8 × 12 mm) (Maestro Dental Implant [BioHorizons]) was placed, aided by a surgical guide. Guided bone regeneration was done, and platelet-rich fibrin and connective tissue graft from the palatal mucosa were also transplanted to the donor’s site to augment the deficiency in soft-tissue structures. The patient returned after 10 days for suture removal and a provisional resin-bonded, fixed denture prosthesis construction. The tissue surface of the pontic was ensured not to exert any pressure on the healing site. In the second stage of surgery, the implant was exposed, and the provisional restoration was screwed onto the implant. Occlusion was adjusted on the crown so that it only shared the centric load and was free from all contacts in eccentric occlusion. The patient was scheduled for multiple visits 2 weeks apart to monitor the gingival shaping progress. Composite resin was added wherever needed and polished, and the provisional crown was screwed and tightened. Once the gingival level was considered satisfactory for both the clinician and the patient, it was time for a final impression (Figure 3).

Figure 2. An occlusal view showing the defect in the buccolingual dimension of the edentulous space.

Figure 3. Proper soft-tissue contour shaped by the emergence profile of the provisional restoration.
Final Restoration
The provisional restoration was used to construct a custom-made impression coping following the technique from Papadopoulos et al.7 First, the provisional was screwed to an implant analog (Figure 4a). An impression tray was fabricated for the analog using a piece of pink wax sheet rolled as a cylinder. A hard-consistency impression material was used to record the emergence profile of the provisional crown. The crown was removed and replaced with an impression coping (Figure 4b). The space previously occupied with the emergence profile of the provisional restoration was filled with Bisacryl temporary crown material (Figure 4c). After complete setting, the custom-made impression coping was unscrewed and finished (Figure 4d). The excess temporary material was removed, and the coping was tightened to the implant inside the patient’s mouth (Figure 5). The screw channel was blocked with Teflon, and a one-step impression technique was chosen. The impression coping was tightened to the analog, positioned in the impression, and sent to the dental laboratory with the diagnostic wax-up cast and a full set of photographs. A lithium disilicate (IPS e.max [Ivoclar]) hybrid abutment with a separate crown made by pressing technology and having the same emergence profile of the provisional and impression coping was fabricated for the case (Figure 6). The separate abutment and crown choice was made because of the frequent fracture of the provisional hybrid crown, indicating its exposure to high forces due to the palatal position of the implant. A medium-opacity ingot was selected for the abutment to block the titanium-base (Ti-base) metallic color, while a low-translucency ingot was chosen for the crown. After the try-in visit, the restorations were returned to the dental laboratory for glazing and hybrid abutment cementation to the titanium base. The Ti-base was sandblasted with 100-µm alumina particles. While fitting surfaces of the hybrid abutment, the screw channels were etched with a 9% hydrofluoric acid etchant (Porcelain Etch and Silane 9% buffered HF acid [Ultradent Products]) for 20 seconds, thoroughly rinsed, and dried before being treated with silane coupling agent (Porcelain Etch and Silane). Dual-cured adhesive resin cement (Multilink Automix [Ivoclar]) was used to bond the abutment and the Ti-base. The patient proceeded with the delivery visit, reinspected the crown, and approved it for final cementation.

Figure 4. (a) A temporary crown was mounted on analog and impression material and was used for recording the emergence profile. (b and c) The temporary crown was replaced with the impression coping, and flowable composite material was used to fill the space. (d) The custom implant impression coping.

Figure 5. Custom implant impression coping.
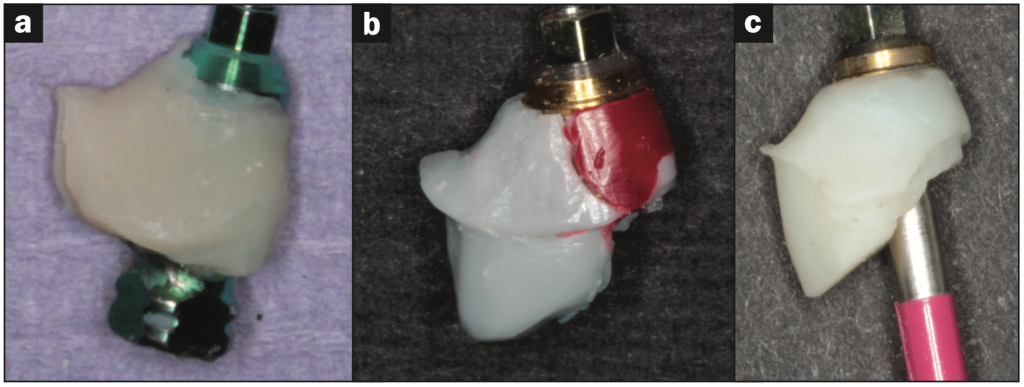
Figure 6. Copying the emergence profile from (a) the impression coping to (b) the wax pattern to (c) the final abutment.
Need for Modification
At this stage, the clinician and the patient noticed the more incisally aligned gingival margin of the ceramic crown that was overlooked in the temporary and try-in stages (Figure 7). Additional composite resin material was added to the labial emergence profile of the provisional crown to push the gingival tissues further apically. After 4 weeks, the new gingival level was stabilized, and a new impression was taken. After pouring the stone cast, the space around the abutment showed the amount of ceramic that needed to be added to adjust the gingival line, but as the abutment was cemented with resin cement to the Ti-base, the addition was impossible. The only solution seemed to be to remake the crown and the abutment!

Figure 7. The difference in gingival levels between the restored and the natural maxillary incisor.
The patient and clinician agreed upon keeping the crown, while the addition in the emergence profile of the abutment was built separately in wax, pressed, and luted to the ceramic abutment (Figures 8 and 9). Once the fit was confirmed, the piece was extraorally etched, silanated, and cemented to the hybrid abutment (Figures 10 and 11). The delivery process was completed by etching and silanizing the hybrid abutment and the fitting surface of the crown.

Figure 8. Spruing the wax piece intended to modify the emergence profile.
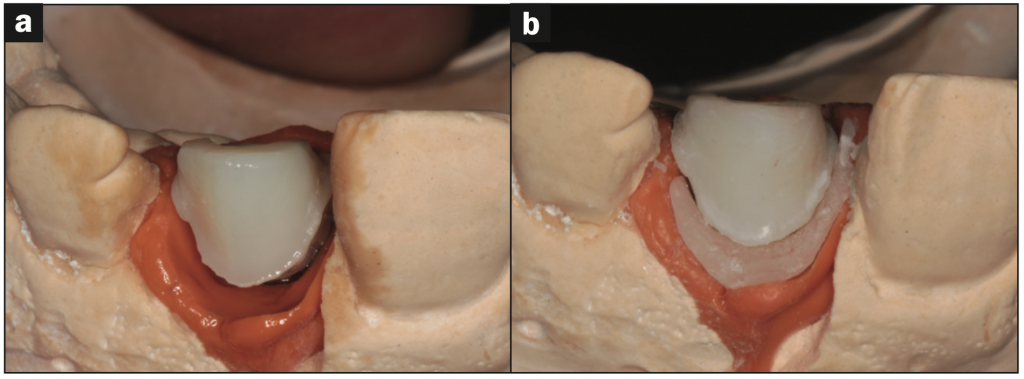
Figure 9. (a) The hybrid abutment on the cast showing the deficient emergence profile. (b) Here it is shown after pressing the added piece to the existing emergence profile and before cementation.
The abutment was screwed to the implant with 30 Ncm of force with a torque wrench, the screw channel was blocked with Teflon and light-cured composite resin, and the crown was finally cemented (Figure 12). The occlusion was adjusted so that, in light contact, the crown wouldn’t share in the centric occlusal load and would share only in the heavy biting. The eccentric contacts couldn’t be totally eliminated due to the protruded lower left central incisor, but the occlusion was adjusted so that it shared in heavy contact protrusive movements only. The patient was instructed to monitor the gingival condition and was given sufficient oral hygiene measures, scheduled for recall visits, and followed up for 36 months afterward (Figure 13).
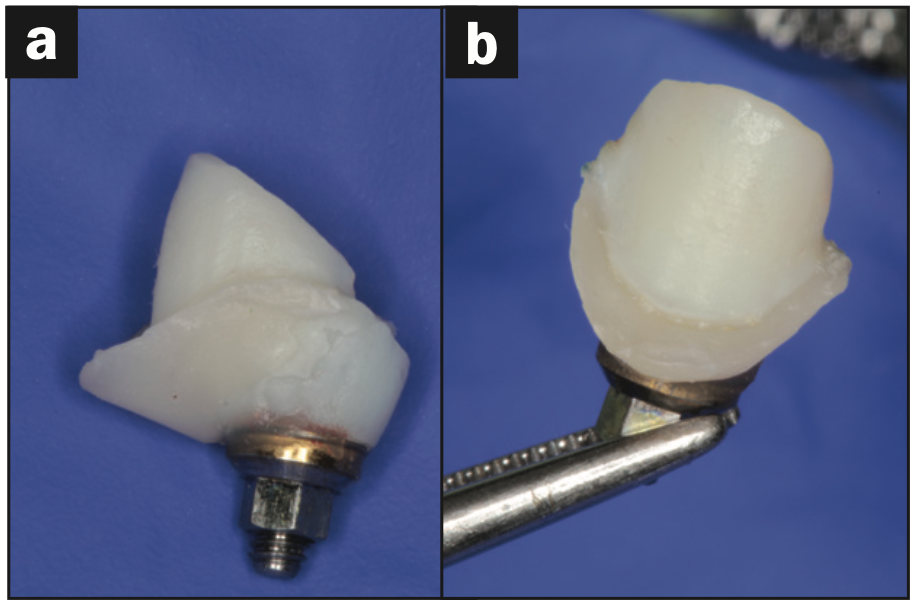
Figure 10. The hybrid abutment after modification.
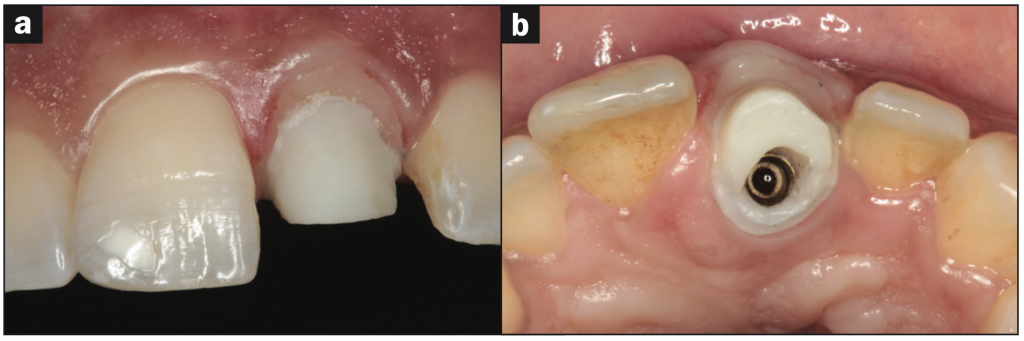
Figure 11. Intraoral photographs of the new gingival level exerted by the modified hybrid abutment: the (a) frontal and (b) occlusal view.

Figure 12. Immediate postoperative image.
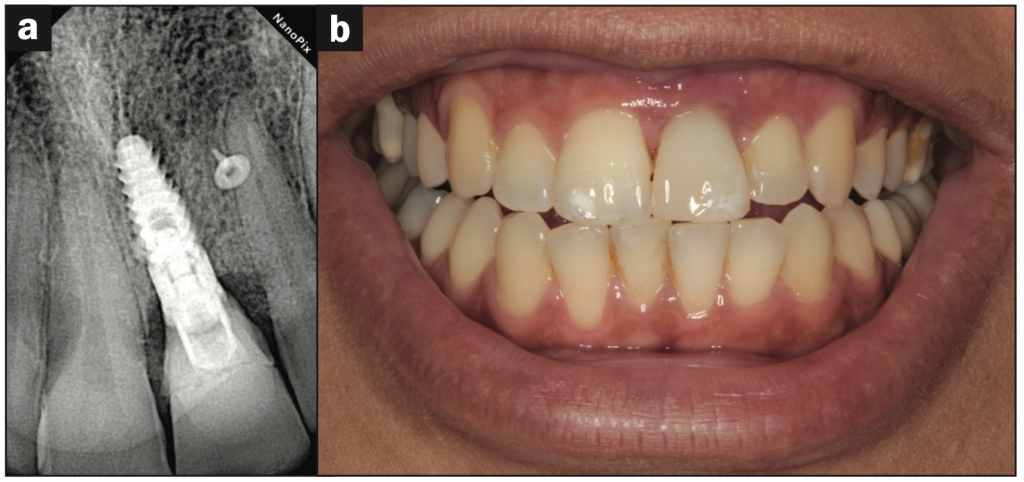
Figure 13. (a) Periapical radiograph and (b) intraoral retracted view after a 36-month follow-up appointment.
DISCUSSION
Because of their proximity to one another that facilitates critical evaluation, a missing single central incisor can be the most challenging case for the clinician and technician but also the most rewarding. A dental implant is considered the first line of treatment in the case of single missing teeth and has the greatest success rate. In the aesthetic zone, osseointegration and function of a single implant are no longer the only criteria for determining success in state-of-the-art of implant dentistry. There must not only be osseointegration of single implants but also harmonious soft- and hard-tissue architecture complementing natural-looking implant restorations.8 To achieve optimal aesthetics regarding soft tissues, several issues have been taken into consideration recently, including implant-loading protocol, provisional restorations, aesthetic and biocompatible properties of restorative materials, the proper 3D implant placement, and gingival biotype.9-14 An implant abutment emergence profile similar to that of a natural tooth is required to support and contour the peri-implant soft tissues. The circular, small-diameter implant, when compared to the root of a natural tooth, creates a dilemma of how to construct a restoration that imitates the natural tooth form.15 As implants have cylindrical form, it is impossible for restorations emerging from them to restore and maintain gingival margins to imitate those supported by anatomically correct, natural teeth.16 Soft-tissue management with provisional restorations utilizing the selective pressure method via provisional restorations is essential. As the soft tissues tend to slump and collapse in no time after provisional removal using a technique that ensures proper subgingival contours, recording is mandatory for fabricating a final restoration that supports the gingival tissues in the right position. One of these techniques involves indirectly replicating the subgingival contours of the provisional abutment in an impression material or autopolymerizing acrylic resin.17,18 Since the platform size of the abutment typically matches that of the implant replacing the missing root, the resulting emergence profile of the final restoration will never replicate that of the natural tooth, making customization inevitable.19 The hybrid abutment is a ceramic abutment, which is luted to a Ti-base with a crown cemented on it. The Ti-base provides space for the pressed restoration required to adjust the shape, emergence profile, and aesthetic properties of this abutment according to the clinical situation.20 With the preparation margin of the crown located on the gingival level, the geometry of the hybrid abutments allows for an easy integration of the restoration and excess cementation material is, therefore, easily removed.20 In this case report, a modification in the subgingival contours was required after the ceramic abutment cementation to the Ti-base. The clinician had to remake the whole restoration or depend on the reliable hydrofluoric acid and silane coupling agent surface treatment for glass ceramics. A strong and durable resin bond provides high retention, improves marginal adaptation, prevents microleakage, and increases the fracture resistance of the restored tooth and the restoration, yielding durable results when guidelines are followed.20
CONCLUSION
In cases with implant placement in the aesthetic zone, osseointegration alone cannot determine the success of a dental implant restoration. The challenges faced by the clinician and technician in each step to deliver a restoration that fulfils the patient’s needs aesthetically and functionally and maintains biological tissue health are innumerable. In this case, the maxillary central incisor was restored with a lithium disilicate hybrid abutment and crown. Surgical as well as prosthetic treatments were performed to restore white and pink aesthetics.
And after a 3-year followup, it was concluded that treatment using customized implant solutions with the modified emergence profile with bonded glass ceramics was satisfactory and stable.
ACKNOWLEDGMENT
The authors would like to express appreciation to Dr. Karim Abdelmohsen, assistant professor of oral and maxillofacial implants, faculty of dentistry, Ain Shams University, for performing the surgical procedures.
REFERENCES
1. van Brakel R, Noordmans HJ, Frenken J, et al. The effect of zirconia and titanium implant abutments on light reflection of the supporting soft tissues. Clin Oral Implants Res. 2011;22(10):1172–78. doi:10.1111/j.1600-0501.2010.02082.x
2. Santosa RE. Provisional restoration options in implant dentistry. Aust Dent J. 2007;52(3):234–42. doi:10.1111/j.1834-7819.2007.tb00494.x
3. David R. Provisional restoration for an osseointegrated single maxillary anterior implant. J Can Dent Assoc. 2008;74(7):609–12.
4. Rompen E, Raepsaet N, Domken O, et al. Soft tissue stability at the facial aspect of gingivally converging abutments in the esthetic zone: a pilot clinical study. J Prosthet Dent. 2007;97(6 Suppl):S119–25. doi:10.1016/S0022-3913(07)60015-8. Erratum in: J Prosthet Dent. 2008;99(3):167.
5. Schoenbaum TR, Han TJ. Direct custom implant impression copings for the preservation of the pontic receptor site architecture. J Prosthet Dent. 2012;107(3):203-6. doi:10.1016/s0022-3913(12)60059-6
6. Raigrodski A. Managing the challenge of crowning the single central maxillary incisor. J Esthet Restor Dent. 2008;20(5):337–42. doi:10.1111/j.1708-8240.2008.00206.x
7. Papadopoulos I, Pozidi G, Goussias H, et al. Transferring the emergence profile from the provisional to the final restoration. J Esthet Restor Dent. 2014;26(3):154–61. doi:10.1111/jerd.12068
8. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313–23.
9. Buser D, Chen ST, Weber HP, et al. Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures. Int J Periodontics Restorative Dent. 2008;28(5):441–51.
10. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113–9.
11. Grütter L, Belser UC. Implant loading protocols for the partially edentulous esthetic zone. Int J Oral Maxillofac Implants. 2009;24 Suppl:169–79.
12. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18(1):31-9.
13. Kan JY, Rungcharassaeng K, Morimoto T, et al. Facial gingival tissue stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: consecutive case report. J Oral Maxillofac Surg. 2009;67(11 Suppl):40–8. doi:10.1016/j.joms.2009.07.004
14. Kois JC, Kan JY. Predictable peri-implant gingival aesthetics: surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001;13(9):691–8.
15. Wu T, Liao W, Dai N, et al. Design of a custom angled abutment for dental implants using computer-aided design and nonlinear finite element analysis. J Biomech. 2010;43(10):1941–6. doi:10.1016/j.jbiomech.2010.03.017
16. Lazzara RJ. Managing the soft tissue margin: the key to implant aesthetics. Pract Periodontics Aesthet Dent. 1993;5(5):81–8.
17. Shor A, Schuler R, Goto Y. Indirect implant-supported fixed provisional restoration in the esthetic zone: fabrication technique and treatment workflow. J Esthet Restor Dent. 2008;20(2):82-95. doi:10.1111/j.1708-8240.2008.00156.x
18. den Hartog L, Raghoebar GM, Stellingsma K, et al. Immediate loading and customized restoration of a single implant in the maxillary esthetic zone: a clinical report. J Prosthet Dent. 2009;102(4):211–5. doi:10.1016/S0022-3913(09)60154-2
19. Shafie HR. Clinical and Laboratory Manual of Dental Implant Abutment. Wiley-Blackwell; 2014.
20. Kansu G, Gökdeniz B. Effects of different surface-treatment methods on the bond strengths of resin cements to full-ceramic systems. J Dent Sci. 2011;6(3):134–9. doi:10.1016/j.jds.2011.05.002
ABOUT THE AUTHORS
Dr. Emam attended Ain Shams University in Cairo, Egypt, where she received a bachelor’s degree in dentistry as well as an MSc degree and a PhD in fixed prosthodontics. In 2021, she was a postdoctoral visitor researcher at the University of Bonn in Germany. Later, she received a professional diploma in hospital infection control from the Faculty of Medicine, Ain Shams University. She is currently a lecturer in the department of fixed prosthodontics, Faculty of Dentistry, Ain Shams University, and has authored several publications in the field of prosthodontics. She is also a speaker at national and international dental conferences. She can be reached via email at marwaemam@asfd.asu.edu.eg.

Marwa Emam, MSc, PhD
Dr. Eldimeery attended Ain Shams University, where he received a bachelor’s degree in dentistry as well as an MSc degree and a PhD in fixed prosthodontics. He is the owner of Perfect Dental Clinic private practice and course coordinator of the postgraduate occlusion program, Faculty of Dentistry, Misr International University, in Cairo, Egypt. He is also a speaker at national and international dental conferences. He can be reached via email at aymangalal@asfd.asu.edu.eg.

Ayman Eldimeery, MSc, PhD
Disclosure: The authors report no disclosures.












