The purpose of this article is to summarize the newest dental x-ray guidelines from the National Council on Radiation Protection and Measurements (NCRP) report No. 145, which was released in December 2003, and alert dentists to the potential impact on their office radiographic procedures.1
The NCRP is a nonprofit corporation chartered by Congress in 1964 to perform the following tasks:
(1) Collect, analyze, develop, and disseminate in the public interest information and recommendations about (a) protection against radiation, and (b) radiation measurements, quantities and units, particularly those concerned with radiation protection.
(2) Provide a means by which organizations concerned with the scientific and related aspects of radiation protection and of radiation quantities, units and measurements may cooperate for effective utilization of their combined resources, and to stimulate the work of such organizations.
(3) Develop basic concepts about radiation quantities, units and measurements, about the application of these concepts, and about radiation protection.
(4)Cooperate with the International Commission on Radiological Protection Units and Measurements and other national and international organizations, governmental and private, concerned with radiation quantities, units, and measurements and with radiation protection.
In short, this agency periodically assesses new technology and radiation safety practices to make recommendations about radiological procedures based on available scientific data. In reality, the recommendations are usually adopted by educational institutions and government agencies first, then become part of the end-users clinical practice. The American Dental Associations Council on Scientific Affairs cited 4 NCRP reports in its 2001 report entitled. An Update on Radiographic Practices: Information and Recommendations.2
Definitions of shall and shall not and should and should not in the NCRP report are as follows:
(1) As used in the report, the terms shall or shall not mean that adherence to the recommendation is considered necessary to meet accepted standards of protection.
(2) The terms should or should not are used to indicate a prudent practice to which exceptions may occasionally be made in appropriate circumstances.
Our interpretation of the ways these new guidelines will affect you and your office staff follows. These new recommendations will do the following:
• Dramatically change the use of leaded aprons and thyroid collars.
• Mandate the use of rectangular collimation for x-ray generators.
• Mandate the use of selection criteria how a dentist must prescribe radiographs.
• Mandate the establishment of a radiation protection program for each dental office.
• Mandate radiation safety training of all office staff who perform dental x-rays in the office.
• Mandate collimation for cephalometric images to the precise clinical area.
• Mandate that dentists not use sight development for evaluating their films.
• Mandate employing a qualified expert to determine shielding requirements for new or remodeled dental facilities.
• Mandate use of radiation badges for some office staff and all pregnant office staff.
All practicing dentists are interested in minimizing the x-ray dose to patients in dental offices. The dental profession, including the commercial vendors of x-ray products, has made substantial improvements in keeping these patient doses to an absolute minimum; ie, to apply the ALARA principle (As Low As Reasonably Achievable).4 We have protected patients by using faster and faster image receptors, collimating x-ray beams to as small a skin surface area as possible (more on this later), protecting patients with lead aprons and thyroid collars, and now, switching to solid-state image detectors. X-ray machines are even examined and calibrated on a regular basis by a state radiation safety officer. Now, more is required.
Protective X-Ray Devices Leaded Aprons
The use of leaded aprons on patients shall not be required if all other recommendations in this report are rigorously followed. Leaded aprons have long been used in dental offices and institutions for both intraoral and extraoral radiographic procedures as a means of protecting patients. The changes outlined in this report will significantly alter our radiation hygiene procedures and our patients’ perception of the need for radiographs. It is hoped that specialized groups and legislative bodies such as the FDA, NCRP, American Dental Association, and all state dental associations will be prepared for the inevitable questions adult patients will ask when they learn that we will not be using a leaded apron when taking dental x-rays. Imagine the reaction(s) of patients who have already mentioned their concerns about being exposed to dental x-rays and who have been told for years that all the necessary precautions are being taken, including the use of the leaded apron. These patients are likely to react poorly to this new recommendation.
It is our hope that relevant agencies develop a comprehensive educational campaign for dentists, who will attempt to adhere to these new guidelines, and for the public, who might balk at the nonuse of aprons in offices.
Protective X-ray Devices Thyroid Collars
NEW X-RAY COLLIMATION CHANGES
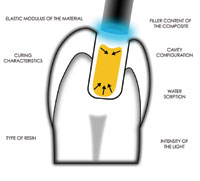
Collimating the x-ray beam to the precise size of the image receptor eliminates scatter radiation. When scatter radiation strikes the film, sensor, or phosphor plate, the result will be a dramatic reduction in image quality. Most vendors produce large, round cones with large x-ray beam patterns so the operator will be sure to expose the film or receptor. This not only adds scatter radiation, reducing image quality, but also adds significantly to the patients x-ray dose. Interpretation of this report suggests that dentists will have to use a rectangular collimator of the precise size of the image receptor. This will improve the images taken and reduce scatter radiation. This collimation also reduces the patients skin surface x-ray dose by almost 60% simply because the beam size is smaller.
The NCRP report No. 145 states the following: Rectangular collimation of the beam shall be used routinely for periapical radiography. Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimension of the image receptor by more than 2% of the source-to-image receptor distance. Similar collimation shall be used, when feasible, for interproximal (bitewing) radiography.
IMAGE RECEPTOR SPEED
Dentists who prefer intraoral ANSI speed D film will need to consider using the faster E- or F-speed film. Although the report cites E-speed film in its shall statement, in reality most dentists in the United States will probably have to adopt F-speed film, since the largest film manufacturer, Eastman Kodak, discontinued the manufacture of E-speed film in December 2001. To be more competitive with the faster phosphor plate and solid-state receptors, Kodak has aggressively marketed In-sight, its F-speed film.
Other film manufacturers still produce E-speed film. Since the committee authoring these guidelines ap-pears to want to require dentists to stop using D-speed film, it is unclear why they did not write their recommendation as a shall statement for the faster F-speed film. The re-port states the following: Image receptors of speeds slower than ANSI speed Group E films shall not be used for intraoral radiography. Faster receptors should be evaluated and adopted if found acceptable.
For extraoral radiography (ie, panoramic and cephalometric imaging), slow-speed, blue-flourescing calcium tungstate screens will no longer be recommended. Since these slower screen phosphors increase the patients skin and absorbed x-ray dose, the NCRP is attempt-ing to dissuade practitioners from continued use in favor of the lower-x-ray-dose-producing faster rare-earth systems.
The fastest imaging system consistent with the imaging task shall be used for all extraoral dental radiographic projections. High-speed (400 or greater) rare earth screen-film systems or digital-imaging systems of equivalent or greater speed shall be used.
Dentists can check the speed of their screens by noting the high-speed or high-plus speed labeling on the screen itself or the blue fluorescence when exposed by their intraoral x-ray machine in a darkened room. The clinician simply has to place the x-ray tube close to the screen material and press the exposure button. The screen will then fluoresce the appropriate color. This simple test will tell the dentist what type of screens he or she employs. Dentists can convert panoramic and cephalometric cassettes simply by removing the old screens and replacing them with new screens. Also, the new screens will need to be matched to a compatible film such as green-sensitive T-Mat G film. Although the above recommendation is not very specific regarding digital receptors, the mention of digital image receptors by the NCRP may prompt the practitioner to consider the purchase of a new factory-equipped digital panoramic or pan-ceph machine.
CEPHALOMETRIC IMAGING
Practitioners using cephalometric imaging should consider the following: Filters for imaging the soft tissues of the facial profile together with the facial skeleton shall be placed at the x-ray source rather than at the image receptor.
The report further states that the x-ray beam for cephalometric radiography shall be collimated to the area of clinical interest. This prevents unneeded exposures to the patient’s hard and soft tissues. However, this equipment modification may not be easy to achieve without purchasing new cephalometric or pan-ceph machines. Once again, this may prompt some practitioners to convert to factory-equipped digital equipment.
In the commentary portion of the text of the NCRP report, it states, Practitioners need to remember that all structures recorded on the image need to be interpreted for evidence of disease or injury as well as for cephalometric analysis.
This may prompt some practitioners to obtain a report from a board-certified oral and maxillofacial radiologist, the ADAs newest recognized dental specialty. Reporting services are available through dental schools, practicing oral and maxillofacial radiologists, and report services such as the Advanced Dental Board, an oral and maxillofacial radiology consultation group of head and neck radiologists located in Las Vegas. The group provides image interpretation services for implant, TMJ, and other radiological images on a fee-for-service basis. There are also several private practice oral and maxillofacial radiologists who perform these services.
SIGHT DEVELOPMENT OF X-RAY FILM
Dental practitioners who sight-develop film (reading wet x-ray films at the time of a procedure) in order to assess endodontic procedures or bite-wing radiographic interpretation should note the following: Dental radiographic films shall be developed according to the film manufacturers instructions, using the time-temperature method and recommended chemistry or its equivalent. Sight development shall not be used.
This may lead some practitioners to consider conversion to digital intraoral imaging systems using CMOS or CCD sensors, which can im-mediately display the image in the operatory.
SHIELDING, BARRIERS, AND DOSIMETERS
For practitioners designing new offices or remodeling existing locations, the shielding design will need to be provided by a qualified expert. However, construction materials other than lead are permitted, and the adequacy of the shielding must be determined. Regarding these issues, the Report states the following: Shielding design by a qualified expert shall be provided for all new or remodeled dental facilities. When a conventional building structure does not provide adequate shielding, the shielding shall be increased by providing greater thickness of building materials or by adding lead, gypsum, wallboard, concrete, steel or other suitable material. Adequacy of shielding shall be determined by calculation and checked by survey measurements.
The report further states that operators need to maintain visual contact with the patient during the x-ray exposure; ie, “Shielding design for new offices shall provide protective barriers for the operator. The barriers shall be constructed so operators can maintain visual contact and communication with patients throughout the procedures.”
This may require modification of some dental offices. Though some practitioners may wish to provide dosimeters for appropriate personnel, most states and institutions do not require this. The report, however, insists that exposed personnel who are pregnant now must be provided with dosimeters; ie, Provision of personal dosimeters for external exposure measurement shall be considered for workers who are likely to receive an annual effective dose in excess of 1 m Sv, and personal dosimeters shall be provided for known pregnant occupationally exposed personnel.
Selection Criteria
Dentists must examine their patients before ordering or prescribing x-ray images, regardless of whether they utilize film, phosphor plate, or solid-state images. Actually, this is not a new guideline. Guidelines on this matter were published several times, several years earlier by the FDA and others and were adopted by the American Dental Association.5-7
The report states, Radiographic examination shall be performed only when indicated by patient history, physical examination by the dentist, or laboratory findings.
The report goes on to define the difference between a symptomatic patient and an asymptomatic patient; ie, For symptomatic patients, radiographic examination shall be limited to those images required for diagnosis and planned treatment (local or comprehensive) of current disease, and For asymptomatic patients, the extent of radiographic examination of new patients, and the frequency and extent for return patients, shall adhere to published selection criteria. These selection criteria have been published.8-10
There is also a section on administrative radiographs related to institutions such as dental schools and state board examinations, which says none shall be taken if they do not relate to a patients health. Additional recommendations relate to eliminating pointed cones and using only open-ended cones as well as restricting the source-to-image distance to a minimum of 20 cm (approximately 8 inches).
Office Radiation Protection Program, Including Radiation Safety Training of Staff
This section will have a significant impact on the way radiographic procedures are performed, including image processing. If conventional x-ray film image processing is used, it is wise to consider switching to digital imaging because of all the steps necessary to meet these new recommendations. The shall statements/recommendations include (1) having a written quality assurance protocol (manual), (2) having your equipment inspected by a qualified expert, (3) evaluating your chemistry daily, (4) evaluating each type of film used monthly for fog or artifacts, (5) inspecting screen-film cassettes after any accident for integrity and performance, (6) repairing any defect found, (7) evaluating your darkroom monthly for leaks or after any changes are made to filters, lamps, etc, (8) visually inspecting leaded aprons monthly, and (9) providing training to all x-ray personnel in radiation protection that is sufficient to ensure they understand the recommendations made in the Lippincott NCRP report.
CONCLUSION
There is little doubt that the report will stir debate within the profession, but it is clear that the recommendations will have a considerable impact on the radiographic practices in all oral healthcare settings. Every dentist must now re-examine his or her radiographic services, protective equipment, and receptor selections to ensure they are practicing within the accepted standards. In addition, it appears many dentists will have to change the way they obtain x-ray information for each patient, including prior examination of each patient to determine his or her precise radiographic needs as based on selection criteria. Finally, this report appears to make a strong case for dentists to adopt digital imaging systems and receptors, especially if they wish to avoid some fairly dramatic changes to the radiation protection program, receptor speeds, filtration, and chemical processing.
References
1. National Council on Radiation Protection and Measurements (NCRP). Radiation Protection in Dentistry. Bethesda, Md: NCRP; 2003. NCRP Report No. 145.
2. ADA Council on Scientific Affairs. An update on radiographic practices: information and recommendations. J Am Dent Assoc. 2001;132(2):234-238.
3. National Council on Radiation Protection and Measurements. Dental X-Ray Protection. Bethesda, Md: NCRP; 1970. NCRP Report No. 35.
4. National Council on Radiation Protection and Measurements. The Application of ALARA for Occupational Exposures. Bethesda, Md: NCRP; June 8, 1999. NCRP Statement No. 8.
5. Joseph LP. The selection of patients for X-ray examinations: dental radiographic examinations. Rockville, Md: The Dental Radiographic Patient Selection Criteria Panel, DHHS, Center for Devices and Radiological Health; 1987. HHS Publication No. FDA 88-8273.
6. Matteson SR, Joseph LP, Bottomley W, et al. The report of the panel to develop radiographic selection criteria for dental patients. Gen Dent. 1991;39:264-270.
7. Council on Dental Materials, Instruments, and Equipment. Recommendations in radiographic practices: an update, 1988. J Am Dent Assoc. 1989;118:115-117.
8. Miles DA, Van Dis ML, Jensen CW, et al. Radiographic Imaging for Dental Auxiliaries. 3rd ed. Philadelphia, Pa: WB Saunders; 1999.
9. Langland OE, Langlais RP. Principles of Dental Imaging. 2nd ed. Philadelphia, Pa: Lippincott Williams and Wilkins; 2002.
10. Miles DA, Parks ET. Radiographic Techniques in Dentistry for the Child and Adolescent. 8th ed. St Louis, Mo: Mosby; 2004.
Dr. Miles is professor of oral and maxillofacial radiology and associate dean for clinic affairs and faculty development at the Arizona School of Dentistry and Oral Health in Mesa, Ariz. He is a diplomate of the American Board of Oral and Maxillofacial Radiology (ABOMR) and secretary to the Board of the International Association of Dentomaxillofacial Radiology. A diplomate of the American Board of Oral Medicine (ABOM) and a past president, Dr. Miles has been a test construction consultant for the National Dental Examining Board for the ADA, and on occasion, serves as consultant to the FDA on radiological devices. He has authored more than 120 scientific articles and 4 radiology textbooks, and he has given more than 300 invited presentations, nationally and internationally. He has been an invited consultant in digital imaging for companies such as Eastman Kodak, Dentrix, Dentsply, Eaglesoft, Suni Imaging, LightYear, and PracticeWorks. He can be reached at damilesrad@cox.net.
Dr. Langlais is professor of oral and maxillofacial radiology at the University of Texas Health Science Center at San Antonio, where he directs the graduate program in the specialty. He has given more than 400 courses and lectures nationally and internationally. He has written 11 textbooks, many of which have been translated into Italian, Spanish, German, Polish, and Japanese. He has published some 150 scientific papers, book chapters, and abstracts. Dr. Langlais is a charter honorary member of the South African Association of Dento-Maxillofacial Radiology; a fellow of the American College of Dentists, International College of Dentists, Royal College of Dentists of Canada, and the American Academy of Oral and Maxillofacial Radiology; an honorary fellow of the Australian Academy of Dento-Maxillofacial Radiology; and diplomate of the American Board of Oral Medicine and American Board of Oral and Maxillofacial Radiology. He can be reached at (210) 567-3341.