INTRODUCTION
The dental literature reports that implants achieve a 95% success rate after 10 years.1 However, the term “successful” could be misleading, at least as far as the lifetime of the implant is concerned. While the definition of implant success includes many critical factors (eg, the implant is non-mobile, integrated, cleansable, functional, and asymptomatic for the patient), it also allows for ongoing marginal bone loss (MBL) of 1.0 mm in the first year, and up to 0.2 mm in each successive year.2 While this standard for MBL is still widely held as the acceptable level, these criteria are inaccurate for a wide variety of implant systems.3 The Sixth European Workshop on Periodontology estimated 50% of implants have peri-implant mucositis and 12% to 40% of implants will develop peri-implantitis.4 With the number of implants placed and the prevalence of periodontal diseases that lead to peri-implant disease and bone loss, many of the implants placed today will fail long-term.
The literature suggests that patients who suffer from periodontal disease will also have a higher risk of complications with their implants4-6 and are at increased risk of peri-implant disease and eventual implant loss.7 Studies have shown that the implant takes on the bacteria present in the patient’s mouth; bacterial biofilm is a major concern and a risk factor for development of implant complications.5 If the patient has gum disease, the tissue surrounding the implant will also contain pathogens for periodontal disease.6 Furthermore, patients with a history of implant failure, as measured by implant removal, are 1.3 times more likely to have a second implant,8 and the greater the number of implants within one subject, the greater likelihood the subject will experience MBL greater than 3 mm.9
For these reasons, it is these authors’ opinion that placing implants before the periodontium is stable and healthy does patients a disservice and contributes to the failure of the implants. Moreover, achieving the proper health requires a definitive treatment modality for periodontal oral health. Probing depths must be less than 5.0 mm whenever possible and with no bleeding on probing. Patients should have excellent oral hygiene; stable occlusion; and, after implant placement, an occlusal guard. Also, patients should participate in frequent periodontal maintenance at regular 12-week intervals as management of periodontal disease is ongoing.10
 |
 |
| Figure 1a. Preoperative radiograph, showing probing depths of 6, 6, 7 | 6, 6, 6, around site No. 8 and 6, 5, 6 | 6, 6, 6 around site No. 9. |
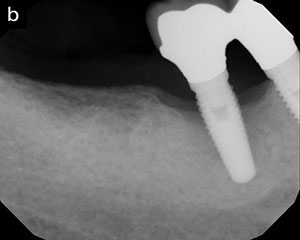
Figure 1b. Three-year postoperative radiograph showing bone fill. Probing depths were 3 circumferentially for both Nos. 8 and 9. |
After treating the oral health of the patient and placing the implant, if complications occur, both peri-implant mucositis and peri-implantitis should be identified and treated early to give the patient the best possible outcome.11 Both require aggressive treatment protocols because the areas around implants experience more rapid bone loss than do teeth. Also, evidence suggests that peri-implant mucositis is reversible if caught early.12,13
Existing literature and clinical experience point to the need for a reliable and predictable way to treat failing implants as there is no standard protocol for treating peri-implant disease.13 The 4 treatments for failing dental implants are mechanical debridement, pharmacological therapy, surgical procedures, and laser therapy.13
The following 2 mini case reports describe the successful treatment of peri-implantitis using laser-assisted regeneration (LAR) with the LAPIP protocol (Millennium Dental Technologies). In both cases, the peri-implantitis was due to periodontitis throughout much of the dentition.
Treatment Protocol
The LAPIP protocol is a multistep protocol that includes the following:
- Probing under local anesthesia to determine the full depth of bony defects
- Using a variable-pulsed 1,064-nm Nd:YAG laser (PerioLase MVP-7 Nd:YAG laser [Millennium Dental Technologies]), as the energy selectively vaporizes bacteria and endotoxins and denatures pathological proteins, ablates diseased epithelial lining and granulomatous tissue, and reduces bacteria (pocket depth, combined with tissue type, determines total energy used)
- Using an ultrasonic scaler (MiniMaster [EMS]) to remove calculus and cement, when present, from the implant surface
- Modifying bone and initiating bleeding
- Using laser energy in hemostasis mode to create a stable fibrin clot containing growth factors from the bone, acting as a natural membrane
- Approximating coronal soft tissue against the implant to achieve adhesion
- Adjusting and monitoring occlusal trauma throughout the healing process
CASE REPORTS
Case 1
A 69-year-old female presented with peri-implantitis surrounding implants placed in the No. 8 and 9 central incisors 18 months previously. In addition, she had 2 draining fistulas on the buccal of each implant, as well as circumferential bone loss around the fixtures. Probing depths around tooth No. 8 measured 6, 6, 7 from DF to MF and 6, 6, 6 from DL to ML; probing depths on tooth No. 9 measured 6, 5, 6 and 6, 6, 6. Bleeding on probing and purulence were noted. The patient had thyroid deficiency and hypercholesterolemia but no other significant medical conditions. Early periodontitis was present in the second molars on the maxilla (Figures 1 to 3).
 |
 |
| Figure 2a. Pre-op photo. | Figure 2b. Three-month post-op view showing reduction in tissue inflammation while maintaining the gingival margin. |
 |
 |
| Figure 3a. One-week post-op view of the subepithelial connective tissue grafts (SCTGs). | Figure 3b. Six-week post-op view of the SCTGs. The SCTGs were done to increase attachment and close fistulas. |
 |
 |
| Figure 4a. Pre-op radiograph, showing probing depths of 8, 8, 8 | 8, 7, 7 around site No. 29 and over 10 circumferentially around site No. 30. | Figure 4b. One-year post-op radiograph showing bone regeneration, with probing depths of 3 circumferentially around site No. 29 and 4, 4, 5 | 4, 5, 5 around site No. 30. |
Treatment Protocol and Results
LAR via the LAPIP protocol was performed using the PerioLase MVP-7 Nd:YAG laser, per the patient’s choice. Three months later, we performed subepithelial connective tissue grafts underneath the existing tissues to close the fistulas and increase the zone of keratinized tissue. After both procedures, the patient was prescribed a combination of acetaminophen and ibuprofen as an analgesic/anti-inflammatory and amoxicillin as an antibiotic. No prescription opioids were necessary. An occlusal adjustment was performed as per the protocol. Healing was uneventful; at the 6-month postoperative visit, the same laser was used again around fenestrations for disinfection. Radiographs were taken at 3 years post-LAPIP treatment. Probing depths were 3 circumferentially for both teeth Nos. 8 and 9, with no bleeding on probing or purulence.
Case 2
A 70-year-old male presented with 2 implants exhibiting signs of peri-implantitis: a compromised implant in site No. 29 and a non-integrated implant in site No. 30. His medical history included heart disease and hypertension; he was currently prescribed and taking rivaroxaban (Xarelto). He also had a history of periodontal disease in the mandible/molar with moderate-to-severe bone loss. Bleeding on probing and purulence were noted. Probing depths around implant No. 29 were 8, 8, 8 | 8, 7, 7 and implant No. 30 was over 10 circumferentially (Figure 4).
Implant No. 30 would be deemed hopeless in the eyes of most clinicians. Despite 40% bone loss on the lingual and 50% bone loss on the facial, the principles of LAR indicate that if the circumferential defect is present, there is still the potential to regenerate bone to the lid of the osseous defect. If traditional surgery and GTR were treatment planned, it would be highly difficult to predictably detoxify the implant in a hemorrhagic site.
Treatment Protocol and Results
The patient was presented with options and chose LAR via LAPIP treatment. No other regenerative materials or biologics were used during the procedure. Periodontal disease in adjacent areas was also treated with the full-mouth LANAP protocol (Millennium Dental Technologies). The patient was prescribed amoxicillin. An occlusal adjustment was performed. One-year post-op probing depths around tooth No. 29 were 3, 3, 3 | 3, 3, 3 and 4, 4, 5 | 4, 5, 5 around tooth No. 30. The patient was thrilled that the implant was re-integrated.
DISCUSSION
These 2 mini case reports demonstrate how LAR via the LAPIP protocol can resolve inflammation as well as restore some of the bone lost due to infection. These cases reflect typical results in our office, where more than 1,000 cases have been treated. Based on our experience, the LAPIP protocol is the standard of care utilized in our office for regenerative procedures around implants. As mentioned before, however, current literature does not endorse any one treatment strategy over another as the best practice for the treatment of peri-implantitis.13 However, it does recommend a re-examination of how much bone loss is acceptable in the long-term survival of a given implant.3
Ending bone loss is essential to the long-term survival of an implant; regeneration of lost bone is ideal. When more bony walls are available at the site, they provide more blood supply to promote bone regeneration regardless of which treatment option for a failing implant is chosen. The most predictable regeneration occurs in a circumferential defect.
Eradicating inflammation from peri-implant disease and improving soft-tissue health is the first step for preventing the loss of bone around the implant. Some research suggests that neither ultrasonic nor mechanical debridement were efficacious for reducing pocket-probing depths in patients suffering from peri-implantitis in their failing implants.14 Furthermore, while pharmacological efforts led to lower levels of bacteria in the short term, they only produced a statistically significant reduction in the proportions of bacteria present immediately after therapy.15 Let us then compare the latter 2 treatment options, guided tissue regeneration (GTR) vs LAR, using a specific treatment method, the LAPIP protocol.
In our experience, GTR is unpredictable and often results in soft- and hard-tissue loss. In the presence of a large defect, GTR surgery necessitates extensive flap reflection and removal of diseased tissue and bone. It is impossible to know if all the affected tissue has been removed, and it is very difficult to detoxify the diseased implant surface using chemical or mechanical cleaning. Additionally, GTR requires a stable blood clot to provide regeneration, relying on a membrane to exclude epithelial downgrowth and a recurrence of the pocket. Often this type of surgical approach results in soft-tissue recession or additional attachment loss, which affects patient satisfaction. Furthermore, bone regeneration around implants is often unpredictable with this method.
LAPIP treatment can eradicate infection and facilitate bone regrowth; research has indicated that all examined cases of the failing implants treated with the LAPIP protocol have reintegrated in the pocket and stabilized with bone growth of 3 to 8 threads upon radiographic examination.16 With the LAPIP protocol, the laser detoxifies the implant immediately. Then the laser biostimulation encourages the regenerative cells. The stable blood flow helps regenerate the lost bone. LAPIP also has an advantage over GTR as it does not necessitate a foreign membrane. With LAPIP, the blood clot is filled with regenerative cells and is sticky and stable, making it difficult to dislodge and creating a natural barrier. LAPIP provides biostimulation to the bone, and that biostimulation activates regenerative cells needed to regrow the hard tissue that was previously lost to infection. Also, because no reflection of a vertically oriented flap is needed, the patient retains the integrity of the structural tissue, allowing for all other future treatment options, if needed. Moreover, the LAPIP protocol maintains soft-tissue height, which sustains aesthetics and improves patient satisfaction with the outcome. The patients in our practice also report significantly less post-op discomfort with the LAPIP protocol compared to GTR, without the need for prescription opioids.
CLOSING COMMENTS
With limited success in mechanical debridement and pharmacological treatments, the 2 remaining treatments for implant failure are GTR and LAR. LAR using the LAPIP protocol and the PerioLase MVP-7 over traditional GTR can yield more predictable results with failing implants resulting from peri-implantitis; allow for definitive eradication of bacteria; maintain soft-tissue height; retain the integrity of structural tissue for any future treatment, if needed; and sustain aesthetics to improve patient satisfaction with the outcome.
References
- Brånemark P-I, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995;6:227-231.
- Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25.
- Schwartz-Arad D, Herzberg R, Levin L. Evaluation of long-term implant success. J Periodontol. 2005;76:1623-1628.
- Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(suppl 8):282-285.
- Armellini D, Reynolds MA, Harro JM, et al. Biofilm formation on natural teeth and dental implants: What is the difference? In: Shirtliff M, Leid JG, eds. The Role of Biofilms in Device-Related Infections. Berlin, Germany: Springer; 2009:109-122.
- Mombelli A. Microbiology and antimicrobial therapy of peri-implantitis. Periodontol 2000. 2002;28:177-189.
- Valente NA, Andreana S. Peri-implant disease: what we know and what we need to know. J Periodontal Implant Sci. 2016;46:136-151.
- Weyant RJ, Burt BA. An assessment of survival rates and within-patient clustering of failures for endosseous oral implants. J Dent Res. 1993;72:2-8.
- Fransson C, Lekholm U, Jemt T, et al. Prevalence of subjects with progressive bone loss at implants. Clin Oral Implants Res. 2005;16:440-446.
- Nagelberg RH. It’s all about perio maintenance. Dent Econ. 2010;100:44.
- Levin L. Dealing with dental implant failures. J Appl Oral Sci. 2008;16:171-175.
- Mombelli A, Lang NP. Clinical parameters for the evaluation of dental implants. Periodontol 2000. 1994;4:81-86.
- Murray CM, Knight ET, Russell AA, et al. Peri-implant disease: current understanding and future direction. N Z Dent J. 2013;109:55-62.
- Karring ES, Stavropoulos A, Ellegaard B, et al. Treatment of peri-implantitis by the Vector system. A pilot study. Clin Oral Implants Res. 2005;16:288-293.
- Mombelli A, Lang NP. Antimicrobial treatment of peri-implant infections. Clin Oral Implants Res. 1992;3:162-168.
- Nicholson D, Blodgett K, Braga C, et al. Pulsed Nd:YAG laser treatment for failing dental implants due to peri-implantitis. In: Rechmann P, Fried D, eds. Lasers in Dentistry XX. Bellingham, WA: Society of Photo-Optical Instrumentation Engineers; 2014:89290H.
Dr. Saltz attended Case Western Reserve University’s advanced 6-year dental program before attending the University of Kentucky postdoctoral program in periodontics and dental implants. He specializes in periodontics, microsurgery, laser and implant dentistry, and oral medicine, with an emphasis on comprehensive full-mouth oral rehabilitation. Dr. Saltz has lectured nationally on topics such as osseous grafts, crown lengthening and root reshaping, soft-tissue plastic surgery, aesthetic enhancement, sinus and ridge augmentation, dental implants, and CT scans and 3-D imaging. He can be reached at docjsaltz@yahoo.com.
Dr. Wilson attended Tufts University School of Dental Medicine, where she was a recipient of the US Army Health Professional’s Scholarship Program and served for 4 years in the US Army as a general dentist. Dr. Wilson attended the periodontal residency program at the University of Colorado School of Dental Medicine, where she was awarded the Robert G. Schallhorn Award for Periodontal Excellence. She can be reached at kdwilson76@gmail.com.
Disclosure: The authors report no disclosures.
Related Articles
Peri-Implantitis: Traditional Versus Laser Treatment
Treating Peri-Implantitis: An Alternative Approach











