There is a broad consensus that adding value to oral healthcare is desirable. The question is how we transition from a dental payment ecosphere dominated by fee for service (FFS) to value-based care (VBC).
The one thing we know is that, however we get to VBC, it will require an acknowledgement and acceptance that sustainable value is a long-term proposition. Alternative payment models (APMs) are integral to any VBC program. They can be implemented quickly, reduce costs, and help improve health, but they cannot do all three.
To underscore the importance of maintaining a long-term perspective, it’s worth revisiting the basic concept of how VBC will work in dentistry. The fundamental goal is to improve the oral health of a provider’s patient panel by increasing preventive services and reducing the number of more costly restorative services. Healthier patients require fewer restorations.
In the initial phase of moving to VBC, a dentist may encounter a backlog of patients with untreated caries or periodontal disease. The process of treating these patients could likely increase costs in the short term. However, in the long term, the oral health needs of those patients treated early will subsequently be met by preventive services.
As noted previously, preventive services are intrinsically less costly and do not need to be delivered by a dentist. As such, dentists can practice at the top of their license delivering surgical procedures.
Adjusting to Different, Coexisting Payment Methods
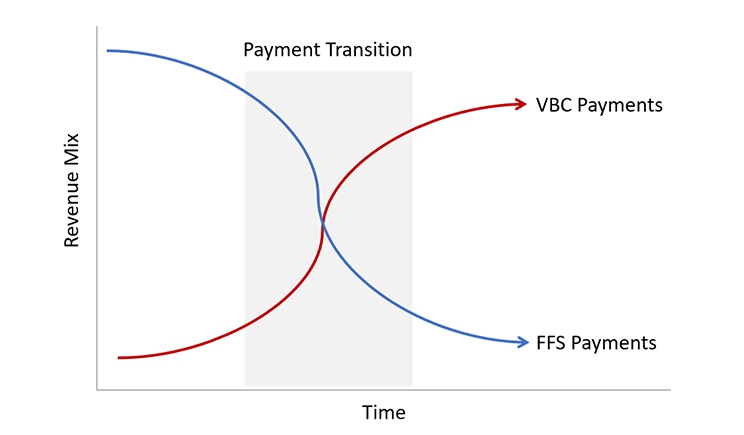
Conceptually, that scenario may make sense. But in practice, the payment mix encountered during the transition from FFS to VBC may offer challenges for dentists and payers (see the figure).
As has been seen in the adoption of new technologies, it is probable that some payers will be innovators in developing VBC plans, while other payers will be what Geoffrey Moore termed laggards.1 The same will be true for dentists. Some will embrace VBC and be early adopters, and others will follow later.
What we expect to see in dentistry may be analogous to what has been seen in care management where programs initially increase patients’ access to care and increase their adherence to recommended medical regimens, which increases the costs of care in the short term.2
Will It Be Worth It?
Sacrificing short-term goals in pursuit of achieving impactful long-term objectives is never easy. But in the case of transforming oral health with VBC, the effort will be rewarded. Reassuringly, there is precedent in the literature for the benefits of adopting a long-term view.
An April 2021 article in the Journal of Dental Research examining health outcomes in the New York State Medicaid Program concluded that “accessing preventive dental care by a large cohort of publicly insured individuals in New York State was associated with better health care outcomes, most notably for the rates and costs of inpatient admissions.”3
In other words, prevention pays.
Another recent study found that compared to FFS payments, APMs in Medicaid were associated with higher access and lower costs.4 Other studies can be found that provide persuasive arguments that VBC can be effective at increasing preventive services, lowering costs, and improving health outcomes.
Setting Expectations for Time to Success
Context for the time to achieve those benefits is reflected by Andrew Cohen, vice president of Kaufman Hall, a management consulting service.
“The transition to a value-based model will be gradual over a period of time, with ‘break even’ occurring in three to five years or possibly in five to 10 years in some organizations. I look at provider organizations that have been at it for 15 years and are still fine-tuning their model,” Cohen said.5
“You don’t sign a contract in August and expect your first bonus check in January the following year. It’s about changing physician, patient and employer behavior,” he continued.
“And, although it will likely take more than a decade for the market to shift, the time to start investing in these skills and capabilities is now. There will always be fee for service on some level. The challenge will be how can we manage a variety of different models as reimbursement fragments,” he said.
Lessons from Medical VBC
It’s fortunate for dentistry that the medical world has extensive experience with VBC and APMs. One of the more important lessons we can learn from their experience is patience. Whether it’s a payer developing an APM or a dentist considering whether to participate in a VBC program, the best strategy is one that prioritizes the long-term benefits. Successes will be measured in years, not months.
References
- Moore, G. A. (1991). Crossing the chasm: Marketing and selling technology products to mainstream customers. New York, N.Y.: HarperBusiness.
- Is Your Care Management Program Working: A Guide to ROI Challenges and Solutions; Flaster, A, Clary, K. (2017) https://www.healthcatalyst.com/care-management-roi-is-your-program-working.
- Dental Services and Health Outcomes in the New York State Medicaid Program – I.B. Lamster, K.P. Malloy, P.M. DiMura, B. Cheng, V.L. Wagner, J. Matson, A. Proj, Y. Xi, S.N. Abel, M.C. Alfano, 2021 https://journals.sagepub.com/doi/10.1177/00220345211007448.
- Matthews, R. (2020, October 13). Use Value-Based Care to Improve Outcomes and Reduce Costs. https://www.dentistrytoday.com/news/todays-dental-news/item/7192-use-value-based-care-to-improve-outcomes-and-reduce-costs.
- Strategies for Success In a Value-Based World Chapman, S. (2014). https://www.fortherecordmag.com/archives/0914p18.shtml#:~:text=Cohen%20believes%20the%20transition%20to,10%20years%20in%20some%20organizations.
Dr. Barefoot has clinical experience delivering patient care in private practice, as part of an HMO dental clinic, via mobile dentistry serving mostly Medicaid schoolchildren, and with other volunteers caring for rural communities in Honduras. His 30-year career in dentistry is complemented by a series of other non-dental endeavors that include medical research at Methodist Hospital of Indiana and business development, analysis, and analytics in a range of areas. He joined DentaQuest in 2016 as dental director for Indiana. In his current role, he provides clinical input to develop new care programs, to manage the design of quality measures, and to respond to questions from providers participating in value-based programs.
Related Articles
Use Value-Based Care to Improve Outcomes and Reduce Costs
How Does Value-Based Care Really Work in a Dental Office?
Partnership Launches Three-Domain Framework for Oral Healthcare











