INTRODUCTION
Applying digital technologies in dental practices today can be confusing, especially for removable prosthodontics. Until recently, complete denture technologies and procedures had remained practically unchanged for the better part of a century. The invention of the intraoral scanner, printable biocompatible resins, and the desktop 3D printer has essentially revolutionized complete denture techniques for the modern dentist. However, acquiring these technologies alone does not necessarily lead to better outcomes. Digital hardware and software must be utilized with sound principles practically and efficiently to benefit dentists in clinical practice meaningfully.
The topic of digital dentures is popular today and encompasses many techniques and workflows that must be understood and combined for successful outcomes. Arguably, the limitations of digital techniques are as important to consider as the possibilities. Today, dentists have more choices available to them for digital denture fabrication than ever before. This case report will follow a specific treatment pathway of a patient receiving complete denture therapy where both digital and analog processes were utilized.
CASE REPORT
A 65-year-old female presented with her chief concern being an ill-fitting and worn upper complete denture (Figure 1). The existing prosthesis was more than 15 years old and no longer stable or retentive. The patient reported she became edentulous in her early thirties, and the current prosthesis was her third complete denture.

Figure 1. Preoperative presentation.
She also reported her previous long-time dentist recently attempted to replace the denture unsuccessfully. The fit, retention, stability, and tooth arrangement were not to the patient’s satisfaction, and she sought to have it remade by a different clinician.
After a review of the medical and dental history, the patient was evaluated clinically and radiographically with a panoramic radiograph. A soft-tissue exam was completed with no significant findings. The patient was fully edentulous in the maxilla and partially edentulous in the mandible. The remaining lower anterior teeth were worn, and there was significant resorption in the posterior mandible as well as the maxilla. The palatal arch form was somewhat flat, and the residual ridge was thin and knife-edged anteriorly. The patient reported having a mandibular removable partial denture that was never comfortable and that she was unable to wear it. She reported being able to function adequately with her remaining dentition. The upper denture was found to be worn with an uneven occlusal plane and curve of Spee. The denture tooth arrangement had a midline discrepancy of approximately 8 mm toward the patient’s right side.
The patient was referred for a surgical consultation to assess the remaining bone volume and evaluate for possible implant support. There was minimal bone remaining, and implant therapy would require significant augmentation procedures the patient was not interested in pursuing. All findings and options were presented and discussed with the patient, including no treatment, as well as risks and benefits. The treatment plan was finalized to replace the complete upper denture and have no treatment in the mandibular arch at the current time.
The patient expressed a desire to have the new denture resemble her existing denture as closely as possible with respect to tooth size, contour, arrangement, and display. It was mutually agreed upon that the midline would be corrected by shifting it to the patient’s left and bisecting the philtrum of her upper lip. She requested the shade to be similar to but slightly brighter than her existing denture.
The “reference denture” technique was utilized to accomplish treatment using the patient’s existing denture and to combine analog and digital workflows. The first step in clinical treatment consisted of making full-face digital portraits with the patient wearing the existing denture in both smiling and retracted poses. These 2 portraits were aligned over each other in digital smile design software (TRIOS Smile Design [3Shape]) that allows the tooth positions to be designed and visualized and toggled accurately between the views.
The proportions and positions of the proposed denture teeth can be customized as the clinician deems appropriate for the particular situation at a level not possible with premanufactured denture teeth. Special care was taken to ensure the patient’s head did not move significantly between the photographs. If the patient’s head moves between the poses, it’s not possible to accurately toggle between the views when designing the tooth positions.
The existing denture was cleaned, and approximately 1 to 2 mm of intaglio acrylic was removed to create space for polyvinyl siloxane. The denture (not coated with adhesive) was loaded with VPS impression material and placed into the mouth in the usual fashion, making sure to record and maintain proper peripheral border molding. The impression was made in 2 phases, with the second phase recording the posterior border palatal seal (Figure 2).
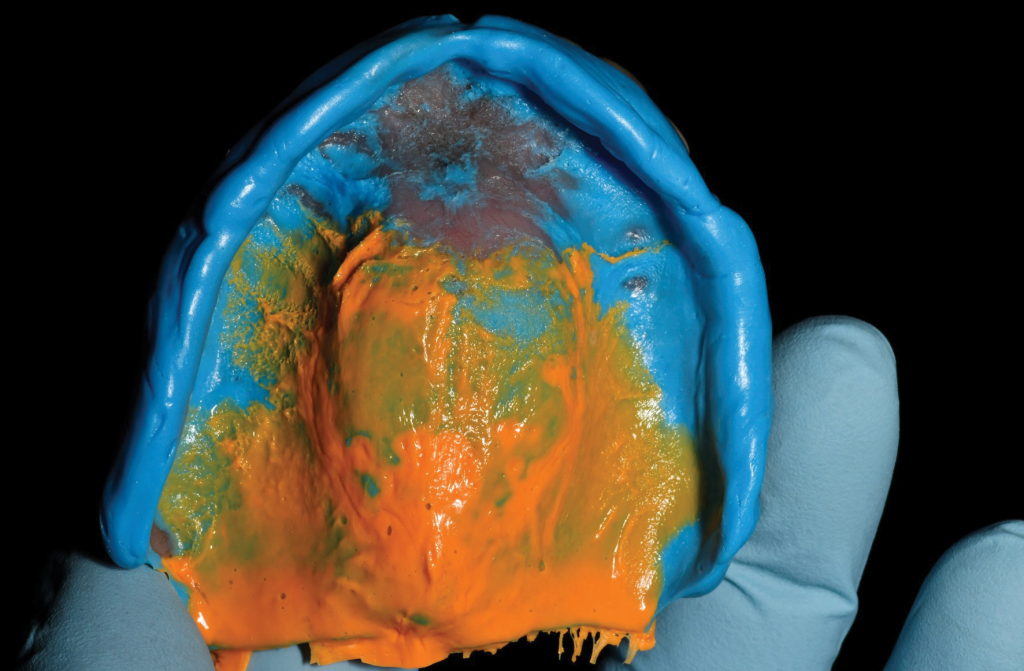
Figure 9. Final prosthesis.
Upon removal of the denture after proper manufacturer setting time, the impression was evaluated and inspected for any significant voids, pulls, or artifacts. The prosthesis was then digitized using a handheld intraoral scanner (TRIOS 4 [3Shape]), beginning on the intaglio surface, then continuing to the peripheral border and, finally, to the labial and occlusal aspects of the denture teeth. The denture was then placed back into the mouth to record the bite relationships. The opposing arch dentition was also recorded with the intraoral scanner in the usual fashion. The denture and all necessary information to design a new denture were now digitized and ready to be utilized (Figure 3).

Figure 3. Data was captured and aligned digitally.
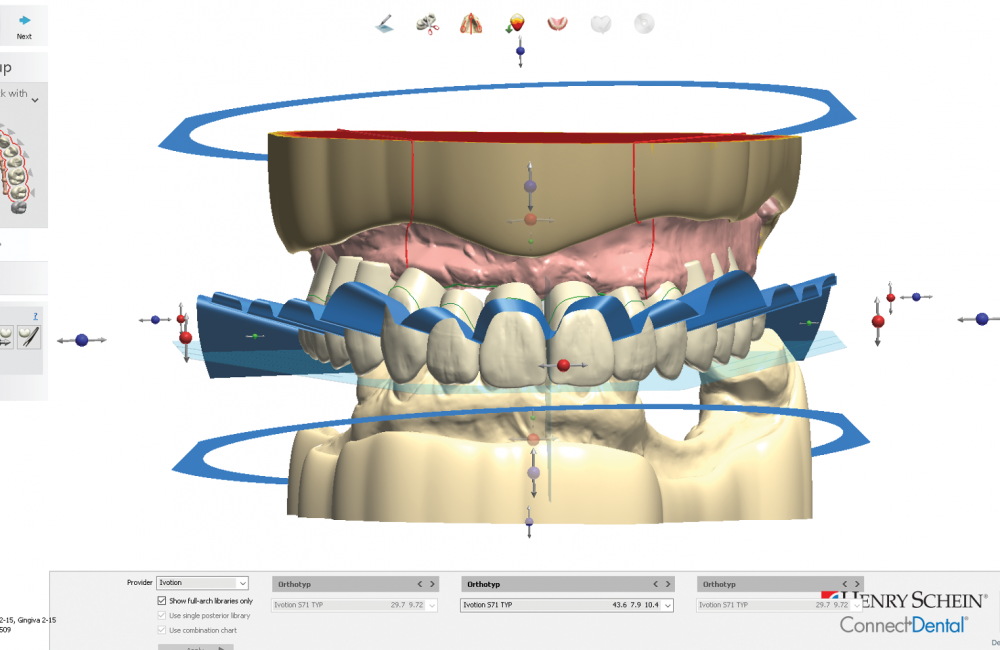
The digital files were exported from the scanning software and imported into the laboratory computer-aided design (CAD) software denture module (Dental System [3Shape]). The denture was virtually designed, and careful attention was paid to the pretreatment goal of maintaining the overall tooth setup and correcting the midline discrepancy (Figure 4).
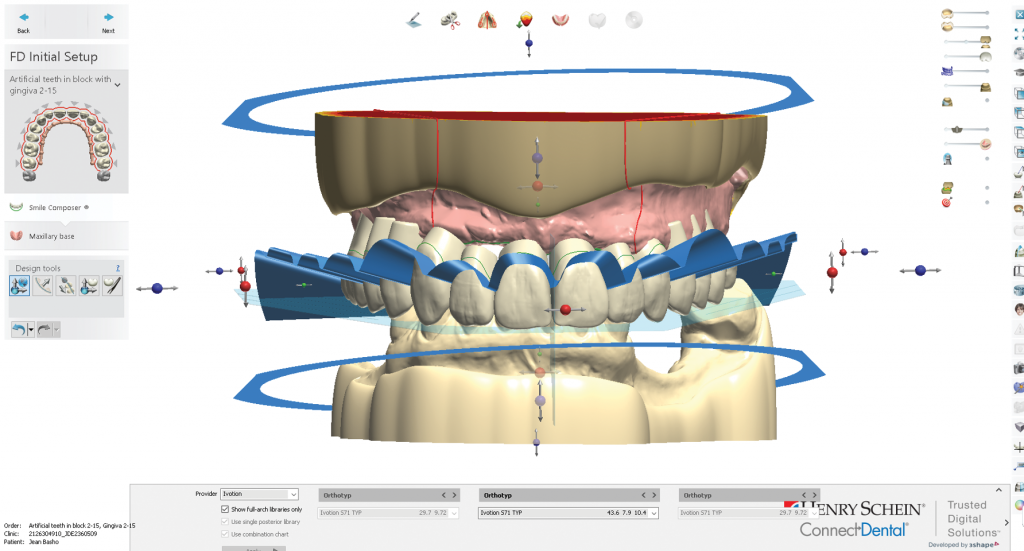
Figure 4. Virtual denture setup and design.
The digital full-face portraits were aligned with the intraoral scan using common landmark points to allow visualization of the denture in relation to the patient’s smile (Figure 5). The desired midline correction could also be visualized within the reference of the patient’s smile to further refine the digital tooth setup (Figure 6).

Figure 5. Digitized impression scan aligned to the facial portrait.

Figure 6. Digital design of the denture setup with a facial reference.
This denture was designed to be milled from a monolithic acrylic puck containing both the gingival base and tooth layer (Ivotion Denture System [Ivoclar Vivadent]). When the design was completed, it was exported from the CAD design software in an STL file format (Figure 7).
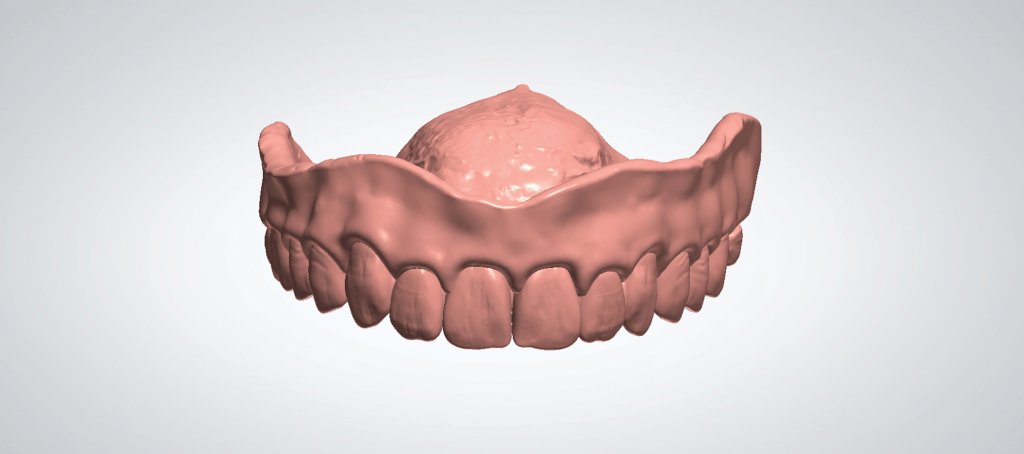
Figure 7. Prototype STL file.
This file was imported into the onsite desktop 3D printing computer-aided manufacturing (CAM) software (Form 3B [Formlabs]) and printed as a denture prototype using biocompatible denture tooth resin (Denture Tooth Resin [Formlabs]). The prototype was tried in the patient and evaluated for aesthetics, occlusion, and phonetics (Figure 8).

Figure 8. Prototype try-in.
Photographs were retaken and analyzed by both the doctor and patient. Following the evaluation, the file was sent to a digital denture laboratory (The Denture Center, Windsor, Ont, Canada) for manufacturing and delivered to the patient in normal fashion. Final photographs were obtained at the one-week postoperative visit (Figure 9).

Figure 9. Final prosthesis.
DISCUSSION
Rates of edentulism in the United States have been on a steady decline since the middle of the 20th century.1 In the 1950s, up to 19% of the general population was edentulous. By 2012, that figure declined to about 5%. This decline constituted a 78% relative decline. Dental schools followed this trend and generally allocated less time and emphasis to teaching complete dentures than in previous periods. In recent years, as dental schools began adopting digital techniques, some institutions even considered the notion of eliminating analog denture content from their curriculums. The topic of how to handle complete denture education in the modern era can be somewhat controversial and variable, depending on the institution.
Since the 20th century, dentistry itself as a profession has undergone marked changes with the development of new technologies, techniques, equipment, and services. Aesthetic, implant, and prosthodontics have developed and enjoyed robust innovations in materials, techniques, and armamentaria. However, proficiency in complete denture techniques still helps one master many of the critical skills required to assess aesthetics, smile design, occlusion, phonetics, and more. The development of digital denture techniques in recent years can complement and enhance the basic skills and concepts learned with analog processes.
Digital denture techniques have developed and grown over the last 2 decades.2 However, there can be confusion about just what a “digital” denture is. The term “digital denture” can be divided between digital information capture and digital manufacturing. There are many decisions that are necessary for each unique clinical situation on how best to use or not use digital technology. The advent of advanced intraoral scanners has allowed dentists to capture edentulous data digitally for the first time. The advancement of milling and printing technologies over the past 20 or so years has allowed the dental technician freedom to manufacture dentures using various techniques, workflows, and materials.
The clinical case presented above utilized multiple techniques and technologies to produce the outcome. The impression was made analog and then immediately digitized. The digital file was used to perform a virtual denture setup and then additively manufactured into a denture prototype rather than a traditional wax setup. Denture prototypes differ from wax try-ins in that a prototype will have a fit identical to the final prosthesis because it is produced from the master impression itself rather than a baseplate hand-formed over the master cast. This allows the clinician an opportunity to evaluate and assess retention and stability prior to finalizing the prosthesis. A significant advantage of this technique is the try-in step with the printed prototype. If retention and stability are not ideal, the prototype can itself be used as a custom impression tray to obtain an updated impression before the final prosthesis is manufactured. With analog-style techniques, cases with a lack of adequate retention and stability were often only discovered at the final prosthesis delivery appointment. This could be potentially upsetting to both doctor and patient when the intention is to finalize treatment during the appointment.
Today, some dentists are adding digital design and manufacturing equipment to their private offices to produce dentures and other final restorations on-site rather than outsource them.3 While certainly possible, producing final restorations on-site may not align with all clinicians looking to leverage technology without also adding cost, complexity, and responsibility. Dentists producing prostheses on-site are essentially starting in-house laboratories in their clinics. Taking control and responsibility for final prostheses ideally requires a trained team, laboratory equipment, and various denture materials.4 If a practice is not performing large numbers of cases, the return on investment may not deliver as intended.
However, utilizing the workflow outlined in this case report allows the clinician to leverage digital technology while still outsourcing final manufacturing. By combining an intraoral scanner, CAD design software, and a desktop 3D printer, the modern clinician can control the data capture, virtual design, and manufacturing of the denture prototype with relatively minimal capital investment. The responsibility and investments required to produce the final restoration can still be outsourced.
The development of digital denture design software allows any clinician to accomplish denture tooth setups accurately and efficiently without the learning curve of traditional manual waxing. These software products have essentially leveled the playing field with respect to the design process such that any clinician can easily learn and apply the workflows. Whereas final outcomes with analog workflows are highly dependent on the technician’s specific experience and hand skills, digital design allows even a novice operator to produce denture setups comparable to those from expert technicians.
Today, many clinicians are interested in using intraoral scanners to record edentulous tissues and eliminating physical impression procedures from complete denture workflows. The proof of concept has been well-documented by groups in the United States and internationally.5 While it is most certainly possible to record edentulous tissues with today’s generation of intraoral scanners, it often remains one of the more technique-sensitive and situation-specific procedures in digital dentistry with some inherent limitations. Variables including limited oral access, strong muscle tone, lack of keratinized tissue, hypermobile tissues, and poor patient cooperation must be considered before scanning tissues directly. Understanding the limitations of digital technology is as essential as understanding its capabilities. In the author’s experience, immediately digitizing an impression offers a consistent method of capturing the necessary information without the variables mentioned above. Combining analog impression techniques with sound prosthodontic principles and digital design/manufacturing processes may offer the best of all worlds in treating complete denture patients today. The patient presented here was immediately satisfied with her new prosthesis, and it required minimal post-op adjustments. Implementing digital workflows in complete denture patients can empower the clinician to provide a more predictable and efficient rendering of complete denture services.
CONCLUSION
Digital techniques in dentistry and removable prosthodontics are rapidly changing the capabilities and workflows available to the contemporary dental clinician. Leveraging digital technologies with sound prosthodontic principles and time-tested analog techniques results in a hybridization of techniques to improve patient outcomes and treatment efficiency.
Dentists taking responsibility for data capture, design, and prototyping while outsourcing final manufacturing offer a pragmatic and practical utilization of digital technologies for complete denture prosthodontics.
REFERENCES
1. Slade GD, Akinkugbe AA, Sanders AE. Projections of U.S. edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93(10):959–65. doi:10.1177/0022034514546165
2. Bonnet G, Batisse C, Bessadet M, et al. A new digital denture procedure: a first practitioners appraisal. BMC Oral Health. 2017;17(1):155. doi:10.1186/s12903-017-0440-z
3. Dusmukhamedov S, Lee C-N, Jeong S-M, et al. Digital denture fabrication: a technical note. Appl Sci. 2021;11(17):8093. doi.org/10.3390/app11178093
4. Andreescu CF, Ghergic DL, Botoaca D, et al. Evaluation of different materials used for fabrication of complete digital denture. Materiale Plastice. 2018;55(1):124–8.
5. Lo Russo L, Caradonna G, Salamini A, et al. Intraoral scans of edentulous arches for denture design in a single procedure. J Prosthet Dent. 2020;123(2):215–9. doi:10.1016/j.prosdent.2019.03.022
ABOUT THE AUTHOR
Dr. Rajan brings more than 18 years of experience to a full-time general practice in Mendham, NJ, focused on restorative, implant, and aesthetic dentistry. Dr. Rajan has been involved with digital techniques in dentistry since 2007. His focus is on optimizing intraoral scanning and digital workflows in restorative practices.
He has lectured extensively nationally and internationally as a key opinion leader for 3Shape, Straumann, and Henry Schein as well as for the Seattle Study Club. Dr. Rajan has obtained Fellowship in the AGD and trained at both Spear Education and the Pankey Institute. He is actively involved in dental education as the assistant director of digital dentistry at the Touro College of Dental Medicine and a founding member at CADpro Academy, a center for education in digital dentistry.
He can be reached at naren@cadproacademy.com.
Disclosure: Dr. Rajan has been a key opinion leader for 3Shape.