
The cystadenocarcinoma is a rare malignant neoplasm (less than 0.5% of all salivary gland tumors) that was first described by the World Health Organization (WHO) in 1991.1,2 It is considered a low-grade malignant neoplasm characterized by cysts and papillaryendo-cystic projections that often exhibits intraluminal papillary growth, but lacks any additional specific pathological features that characterize the other types of salivary gland carcinomas.3
The incidence of cystadenocarcinoma papillary is more common in the major salivary glands (65%) and in the parotid in most cases. In the minor salivary glands (35%), the preference of site is the palate, lip, buccal mucosa, and tongue, respectively.4 The adeno-papillary carcinomas producing mucus are less aggressive than other types of adenocarcinoma in the oral cavity.5
This report demonstrates a rare diagnosis and the surgical technique for a mucinous papillary cystadenocarcinoma in the tongue, its characteristics, and the patient’s follow-up after five years.
Case Background
The procedures employed followed the ethical standards of the 1975 Declaration of Helsinki revised in 2013.6 The patient signed a free and informed consent form, including the release of image rights and scientific publications. To ensure the quality of the present case report, the authors followed the CARE statement.7
An 82-year-old female patient female with leukoderma with controlled hypertension and without other medical histories presented herself at the Universidade Federal Fluminense of Niterói School of Dentistry Department of Oral and Maxillofacial Surgery in Rio de Janeiro with a primary complaint of a tongue lesion in March of 2015.
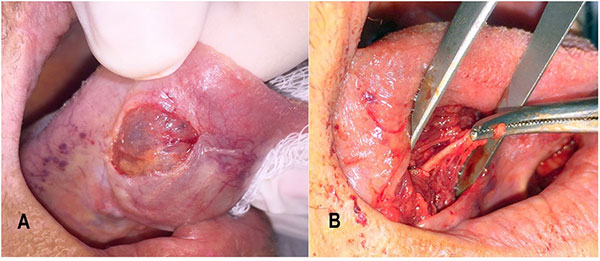 |
| Figure 2. (A) Transoperative picture after the first incision; (B) the hemostatic clamp holding the deep lingual artery, after tumor removal. |
The patient’s chief complaint was difficulty in chewing and swallowing, with a sensation of a “golf ball” in her tongue and without any pain (Figure 1A and 1B). The patient was previously diagnosed with tongue’s mucocele, with failed attempt to drain the lesion, and without prior biopsy.
The Surgical Procedure
The surgical procedure was performed in the operation room under conscious sedation using 15 mg of Dormonid Midazolam (Roche, Rio de Janeiro) and local anesthesia of lidocaine 2% with epinephrine 1:100,000 (DFL, Rio de Janeiro).
 |
| Figure 3. (A) Transoperative picture showing the lesion; (B) macroscopic image immediately after the surgical procedure. |
At the first moment, the patient was prepared for an incisional biopsy. No radiological images were required before the procedure. But during the procedure, after the lesion’s aspiration (mucinous fluid), the surgeons decided to remove the full lesion because they observed an excellent plan of cleavage between the “healthy” tissue and the lesion.
Thus, followed by a superficial incision on the ventral tongue area using a no. 15 blade (Swann-Morton, Sheffield, England) (Figure 2A), the divulsion using a hemostatic curve clamp (Quinelato, São Paulo, Brazil) by anatomical planes was performed. The deep lingual artery was ligated as well (Figure 2B).
The lesion was medial to the trunk of the lingual nerve and the duct of the sub-mandibular gland and lateral to the genius-hyoid muscle.
After the lesion’s removal, the tissue was sutured by planes with Vicryl 4.0 (Johnson & Johnson, Rio de Janeiro). The lesion was excised. It presented a well-circumscribed nodular shape (Figure 3A), measuring approximately 30 by 30 by 30 mm (Figure 3B).
Histopathological Analysis
The slides were obtained from the paraffin blocks and colored with Hematoxylin and Eosin (HE). They were observed in the microscope with a bright-field light (Olympus BX43, Tokyo). The images were captured using 4X, 10X, and 20X magnification (Olympus SC100, Tokyo). Macroscopic evaluation comprised a single nodule measuring 3.0 by 3.0 cm (Figure 3B). Two diverse microscopic patterns were present.
The first pattern revealed a cystic and solid pattern of epithelial and clear cells. Despite the low-grade malignancy aspect, with well differentiated cells, occasional mitotic figures were seen within the solid component presenting abundant small cystic spaces (Figure 4), which arises in multiple locations from the surrounding cystic epithelium of the whole mass (Figure 5). The whole solid components are lined externally by a single layer of epithelial cells in a palisading pattern, such as the epithelial lining of the microcystic component (Figure 4).
 |
 |
| Figure 4. Photomicrograph of the lesion showing an occasional mitotic figure (blue arrow) within the solid growth presenting multiple microcysts (green arrow) within the mass. The solid components and microcystic lining, which is a single layer of epithelial cubic cells in a palisading pattern, can be easily seen at this magnification. Magnification: 20X; stain: hematoxylin and eosin. | Figure 5. Photomicrograph of the lesion with a well differentiated tumor arising in multiple locations (green asterisks) from the surrounding cystic epithelium of the whole mass. The tumor is clearly well circumscribed. Magnification: 4X; stain: hematoxylin and eosin. |
 |
 |
| Figure 6. Photomicrograph of the papillary endocystic projections with widespread mucinous secretion surrounded by a thick layer of connective tissue with occasional calcification with no evidence of necrosis (black arrow). Magnification: 4X; stain: hematoxylin and eosin. |
Figure 7. Neoplastic cells presented sometimes with mild atypic features such as hyperchromatism and nuclear and cellular pleomorphism reinforcing the low-grade pattern of the tumor. The thick connective tissue capsule can be seen in detail at this magnification (white arrow). Magn |
The second pattern was characterized by papillary endocystic projections with widespread mucinous secretion (compatible with the transoperatory surgical findings) surrounded by a thick layer of connective tissue (Figure 6). Occasional calcification could be seen, although no evidence of necrosis could be found. Besides the encapsulation, neoplastic cells presented sometimes with mild atypic features such as hyperchromatism and nuclear and cellular pleomorphism (Figure 7), compatible with the indolent biological behavior usually seen in such rare tumors.
Thirty days after the surgical procedure and the diagnosis of the papillary mucinous cystadenocarcinoma, the patient was forwarded to the Oncological Service of the National Cancer Institute (INCA) in Rio de Janeiro. After a full evaluation of the patient’s body by scintigraphy, there was no evidence of malignant neoplasm elsewhere.
Thus, the tongue tumor was classified as a primary tumor. The patient’s oncologist classified the tumor according to the TNM Classification of Malignant Tumors8 as T2 M0 N0. The head and neck surgeon and the oncologist decided to proceed with 2Gy radiotherapy for five days a week for five weeks. The patient had not required chemotherapy in the present case.
Follow-Up and Outcomes
The patient was observed every six months by the Department of Oral and Maxillofacial Surgery and the Oncology Service. After the first year, the patient presented excellent healing and tongue movements without sequelae (Figure 8A and 8B). The patient was checked for both groups for five years without tumor recurrence (Figure 8C and 8D).
 |
| Figure 8. (A) The dorsal area with one-year follow-up; (B) ventral area with one-year follow-up; (C) dorsal area with five-years follow-up; (D) ventral area with five-years follow-up. |
Discussion
Given the case presented and the surgeons who performed the procedure, it was impossible to include as a differential diagnosis a rare lesion such as the papillary mucinous cystadenocarcinoma. During the clinical examination, the mucocele was one of the differential diagnostics, due to the history presented by the patient and the time. The other hypothesis was pleomorphic adenoma. However, it was not compatible with the main area of involvement, the time of evolution, the age of the patient, or what was observed clinically.
During the operative procedure, high adherence to the surrounding tissues was observed. The nutrition through the deep lingual artery (or ranine artery) stood out among these observations. Thus, the main idea changed to the possibility of a malignant tumor because of the adherence and the irrigation of the tumor observed during the surgical procedure.9
The tumor had a size that caused discomfort for the patient. The treatment for this condition was delayed, as the patient had a previous history of three years. Within this period, some professionals removed the mucous fluid present inside the tumor, causing temporary comfort, but without achieving the definitive treatment.
Even with the long period of evolution, the papillary mucinous cystadenocarcinoma presented in a non-invasive and well-defined manner without causing metastases. These features reinforce a similar prognosis when compared with other tumors of the same type in different locations, such as the ovaries.10,11
Nevertheless, both regional neck lymph node metastasis12,13 and distant lung metastasis14 have already been reported. These findings reinforce the need for a careful clinical examination, and long-term follow-up is essential in patients that present a history of such tumors.
Patient Perspective
The patient shared her experience with our multidisciplinary team and was grateful for the treatment in both services. After those five years, she can now talk, eat, and taste. Also, she has an excellent social life with her relatives.
Conclusion
Although it is a malignant tumor, papillary mucinous cystadenocarcinoma, in the present case, exhibited the behavior of a benign tumor. It can be removed without the need for extensive resection surgery, allowing the patient to obtain an excellent result after treatment by a simple enucleation, followed by radiotherapy.
However, the scarcity of reports of this type of tumor in the literature does not allow us to state that the same will occur in all cases. Further studies are needed on the behavior of this tumor and the survival rate of patients.
References
- Seifert G. Histological Typing of Salivary Gland Tumours. 2nd ed. Springer Verlag; 1991.
- Seethala RR, Stenman G. Update from the 4th edition of the World Health Organization classification of head and neck tumours: tumors of the salivary gland. Head Neck Pathol. 2017;11(1):55-67. doi:10.1007/s12105-017-0795-0
- Barnes L, Eveson JW, Sidransky D, Reichart P, eds. World Health Organization classification of tumors. Pathology and genetics of head and neck tumours. IARC Press; 2005.
- Foss RD, Ellis GL, Auclair PL. Salivary gland cystadenocarcinomas: a clinicopathologic study of 57 cases. American J Surg Pathol. 1996;20(12):1440–7. doi:10.1097/00000478-199612000-00002
- Nakagawa T, Hattori K, Iwata N, Tsujimura T. Papillary cystadenocarcinoma arising from minor salivary glands in the anterior portion of the tongue: a case report. Auris Nasus Larynx. 2002;29(1):87-90. doi:10.1016/s0385-8146(01)00121-3
- Ndebele P. The Declaration of Helsinki, 50 years later. JAMA. 2013;310(20):2145–6. doi:10.1001/jama.2013.281316
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. doi:10.1016/j.jclinepi.2017.04.026
- Sobin LH, Fleming ID. TNM Classification of Malignant Tumors, fifth edition (1997). Union Internationale Contre le Cancer and the American Joint Committee on Cancer. Cancer. 1997;80(9):1803–4. doi:10.1002/(sici)1097-0142(19971101)80:9<1803::aid-cncr16>3.0.co;2-9
- He H, Huang JQ, Ping FY, Chen GF, Zhang SZ. Deep lingual arterial chemoembolization of tongue carcinoma with microcapsuled anticancer drug. J Zhejiang Univ Sci B. 2007;8(10):704-8. doi:10.1631/jzus.2007.B0704
- Akhter N, Habib A. Successful pregnancy outcome with coexisting primary epithelial ovarian carcinoma. Mymensingh Med J. 2013;22(3):599-602.
- Husz V, Bus D, Vajda G. Extremely large epithelial ovarian cancer associated with pregnancy: A case report. Mol Clin Oncol. 2018;8(1):103–6. doi:10.3892/mco.2017.1501
- Etit D, Ekinci N, Evcim G, Onal K. Papillary cystadenocarcinoma originating from a minor salivary gland with lymph node metastases. Ear Nose Throat J. 2011;90(3):E6-7. doi:10.1177/014556131109000314
- Wang KY, Kim DH, Xu Y, Rad MG, Lincoln CM. High-grade features of papillary cystadenocarcinoma of the parotid gland. Oman Med J. 2019;34(2):164–8. doi:10.5001/omj.2019.30
- Nishimaki F, Gibo T, Tsukada K, et al. A rare distant metastasis of papillary cystadenocarcinoma arising from maxillary gingiva. Case Rep Oncol. 2020;13(2):683–8. doi:10.1159/000507956
Carlos Fernando de Almeida Barros Mourão is a member of the Biotechnology Department and the Department of Oral Surgery at the School of Dentistry at the Universidade Federal Fluminense of Niterói in Rio de Janeiro. Correspondence may be sent to mouraocf@gmail.com.
Luiz Antonio Tato is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Rafael Coutinho de Mello-Machado is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Kayvon Javid is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Pietro Montemezzi is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Daniel Cohen Goldemberg is a member of the Department of Oral Pathology at the National Cancer Institute of Brazil (INCA) of Rio de Janeiro
Madelaine Torres da Silva is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Monica Diuana Calasans-Maia is a member of the Department of Oral Surgery at the School of Dentistry at the Universidade Federal Fluminense of Niterói.
Related Articles
Know the Risks Before Adding Phlebotomy to Your Dental Practice
Management of Oral Viral Lesions With a Diode Laser
Dentistry: Do It for More Than the Money



