INTRODUCTION
In the current era of aesthetic dentistry, implant placement poses a serious challenge for the surgeon when attempting to restore severely atrophic alveolar ridges, especially in the maxillary aesthetic area. Within the realm of horizontal ridge augmentation, ridge-split procedures have long been used and modified since the 1970s. There are many new instruments and innovative techniques to maximize their success and provide predictable outcomes. This paper will review current methods that are reported in the literature and provide a new approach for “ridge expansion osteotomy” via a combination of techniques involving both full- and partial-thickness flaps, which may improve long-term success and predictability of the procedure.
The anterior edentulous maxillary ridge remains one of the most challenging areas for implant placement. After extraction, bone volume can be reduced by 40% to 60% in the first 6 months without the use of grafting materials,1 which translates to a resorption of 1.5 mm in height and 3 to 4 mm in width.2,3 Different methods are available to augment the atrophied maxillary ridge, such as guided bone regeneration, a block graft, distraction and expansion, a ridge split, or a combination of said techniques. The main advantage of the split ridge technique is that implants can be placed simultaneously, saving the patient and clinician time and additional surgical procedures. Implant placement, in conjunction with the split ridge technique, will also maintain and prevent collapse of the cortical plates. The ridge expansion/split ridge technique dates back to 1986, when Tatum4 introduced D-shaped osteotomes for ridge expansion. In 1990, Scipioni et al5 introduced a greenstick fracture technique with immediate ceramic root form implants, which was later modified in 1992 by Simion et al6 to incorporate the use of a chisel to split the ridge and the use of e-PTFE membrane to cover the site. In 1994, Summers7 introduced the “ridge expansion osteotomy (REO)” technique with the use of tapered osteotomes. In 2000, Vercellotti8 introduced the use of piezosurgery for ridge expansion, allowing for a more controlled expansion in more mineralized bone. Since then, many other instruments and modifications of the techniques have been introduced, all reporting success rates, improvements in surgical results, and shortened treatment times.
In recent years, few systematic reviews trying to provide clinicians with proper evidence of available ridge-split procedures have been published. Unfortunately, concrete conclusions are hard to develop when there is so much heterogeneity between the techniques published. For example, a systematic review by Mestas et al9 in 2016 reported survival rates of implants placed in expanded ridges using split crest techniques to be 96.8%, yet the included studies were of low to medium quality. In addition, there was great variability in the techniques and materials used in each of the included publications. Another systematic review by Elnayef et al1 in 2015 had cited 17 articles that reported survival rates of 97% for patients treated with alveolar ridge splits with full-thickness flaps and a 95.7% survival rate for patients treated with partial-thickness flaps. Their review of the characteristics of the studies analyzed showed that no study was the same. Variabilities between studies differed in the type of study; the location of the defect (mandible/maxilla); the flap design; the use of bone grafts, materials, membranes, and growth factors; and the type of implant system used.
Overall, considerable variability exists in the literature regarding all aspects of the procedure, such as the flap design, the instruments used for splitting and ridge expanding, the addition of bone grafts, and the use of membranes. Thus, a systematic review of available articles would guide you in terms of which technique will provide the best results. Nevertheless, it can tell you that the concept of ridge splitting can achieve acceptable results when reconstructing the deficient anterior and premolar maxillary areas via the use of implants.
A study by Nguyen et al10 in 2016 evaluated the efficacy and safety of ridge splitting and expansion using the piezoelectric device together with implant placement. The results are in accordance with the other studies demonstrating that the technique is safe and acceptable. However, it is worth noting that the authors pointed out a major drawback that was observed regarding the low amounts of bone and soft tissue that remained after healing. As a result, additional grafting may be necessary for long-term stability, especially in the aesthetic zone. The risk of lacking sufficient amounts of hard and soft tissue was also noted in a systematic review by Bassetti et al11 in 2016 when a full-thickness flap was elevated during the ridge-split procedure.
Through the use of schematics and a case report, this article will introduce a new combination of known techniques for REO that is aimed to enhance clinical outcomes in the anterior and premolar area—an area that is very demanding aesthetically. It is important to mention that this is a very dynamic technique, whereby each step can be modified according to each individual case since no case presents itself equally.
MATERIALS AND METHODS
Patient Selection
Patient selection for the procedures was done after periodontal and prosthetic evaluation. CBCT was used to evaluate the patients for case selection. All patients were healthy and without any major systemic diseases.
Surgical Procedure
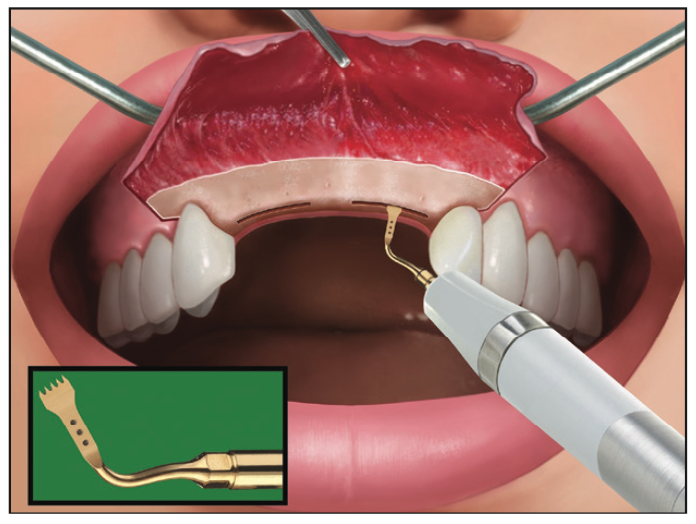
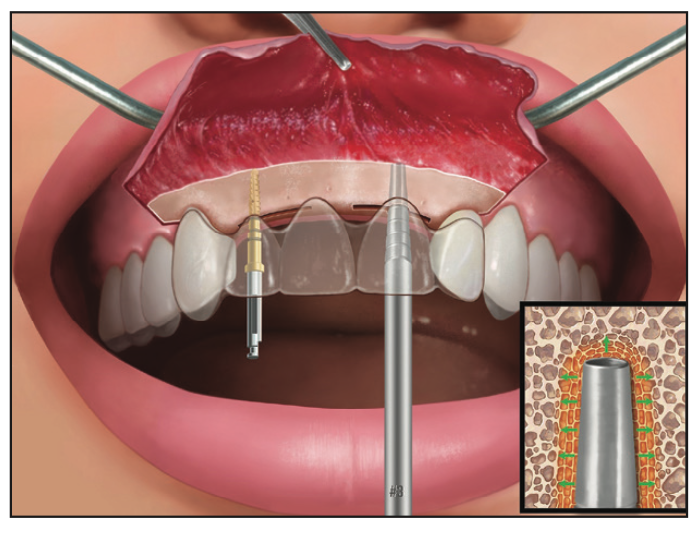
After local anesthesia administration, a palatal crestal incision was made over the edentulous ridge, along with intrasulcular or submarginal incisions that were made at least one tooth away from the edentulous area (Figure 1). Subsequently, a full-thickness flap was then elevated up to the level that does not require augmentation, followed by a split-thickness flap that was then made further apically (Figure 2). For example, in the case of triangular-shaped ridges, the base may be wide enough (7 to 8 mm), and only the coronal portion of the ridge may need to be augmented via the use of a full-thickness flap while the base is raised via a split-thickness flap.
A piezosurgery instrument with an OT7 tip (Mectron) was used to split the ridge at the edentulous area apical to the level of the base where there is sufficient bone, which coincides with the same level, or 1 to 2 mm apical to the start of the full-thickness flap, while also being at least 1 to 2 mm beyond the implant site mesiodistally (Figure 3). To prevent slipping of the osteotomes, a round bur or pilot drill was used to mark the implant site on the bone with the use of a surgical guide (Figure 4).
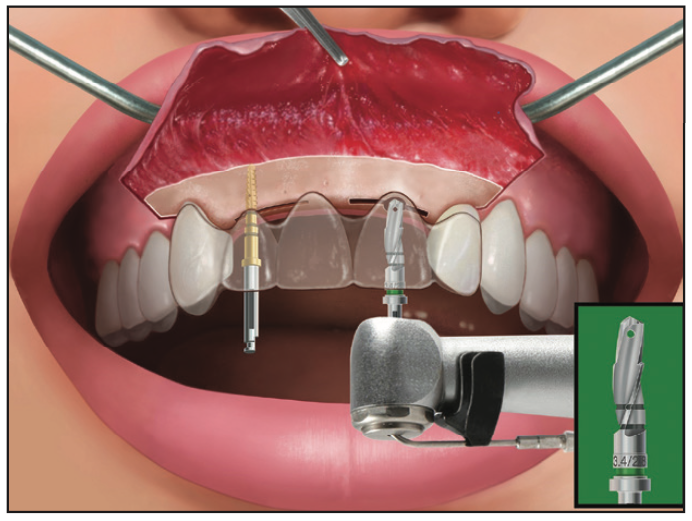
Sequential Tapered Implant Osteotomes (Salvin Dental Specialties) were used to expand and condense the bone up to the implant size expected to be placed (Figures 5 to 8).






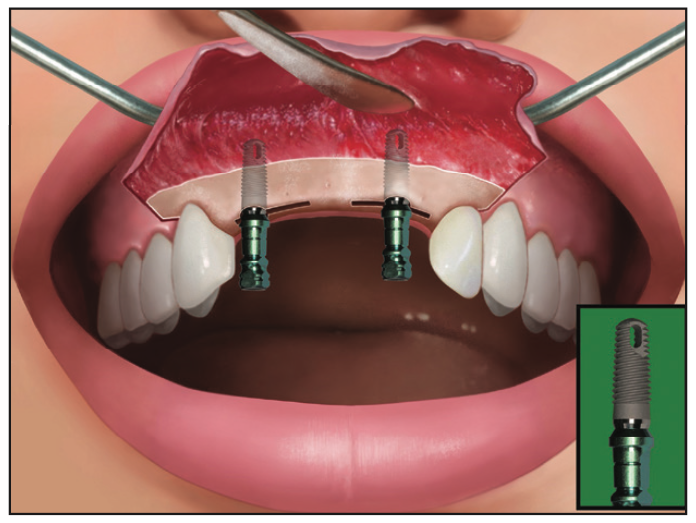
If bone quality is very good, an undersized tapered shaping drill can be used to shape the osteotomy (Figure 9). After implant placement (Figures 10 and 11), the buccal plate at the area of the augmentation was decorticated (Figure 12) and particulate allograft or xenograft was placed either with or without growth factors such as platelet-derived growth factor (PDGF) or platelet-rich fibrin (Figure 13).





Next, a resorbable membrane was placed and stabilized with either tacks or periosteal sutures (Figure 14). Finally, the flap was repositioned and sutured with primary closure (Figure 15).
CASE REPORT
A 45-year-old female presented to the graduate periodontics clinic for the replacement of teeth Nos. 4 and 5. Her medical history was non-contributory for surgery. During consultation, a clinical and radiographic exam was performed and a CBCT scan was ordered (Figures 16 and 17). The maxillary CBCT analysis showed an atrophic ridge around sites Nos. 4 and 5 (Figure 18) with a buccal-palatal dimension of approximately 4 mm. Thus, the patient was planned for a split ridge implant placement procedure.



During the procedure, 2 carpules of 2% lidocaine with epinephrine 1:100,000 were administered via buccal and palatal infiltrations. A papilla-sparing incision from the mesial of tooth No. 3 to the distal of tooth No. 6 was performed along the palatal aspect of the crest of the ridge. A full-thickness mucoperiosteal flap was then reflected to the extent of the anticipated buccal augmentation. A partial-thickness flap was continued apically to maximize blood supply to the alveolar ridge.
Using the OT7 piezoelectric instrument tip, a 10-mm-deep crestal trough was performed, extending mesially and distally to implant sites Nos. 4 and 5 (Figure 19). Using the surgical stent, sites were marked, and the pilot drill was used for the initial osteotomy. Tapered Implant Osteotomes were utilized sequentially for crestal expansion. Ridge expansion was deemed complete when the buccal-palatal dimension was adequate to accept a 3.25-mm-diameter implant (6 mm), which corresponded to a 2-mm increase in buccal-palatal ridge width.



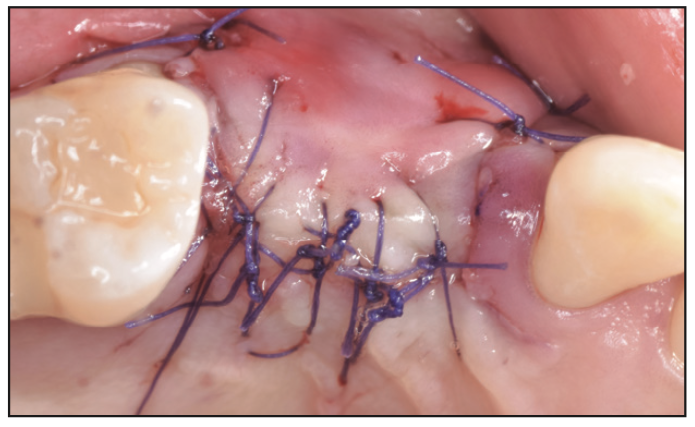
Two Biomet 3i 3.25- × 13-mm implants were then placed with insertion torque values of 35 Ncm (Figure 20). Buccal decortication was completed with a half-round bur. Puros Cortical Allograft (Zimmer Biomet) was placed on the buccal portion of the ridge, and a Bio-Gide (Geistlich) membrane was placed extending from the palatal to the buccal surface, covering the allograft (Figure 21). Tension-free primary closure was achieved using 5-0 vicryl sutures (Figure 22). The patient was seen for a series of postoperative appointments, whereby healing was uneventful at each visit.
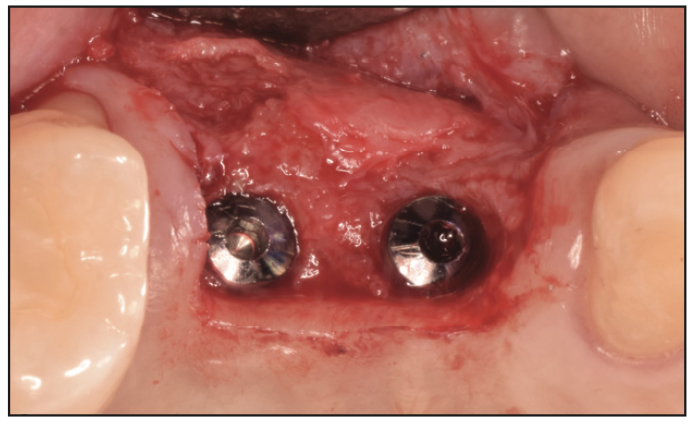


At 3 months, a second-stage procedure was performed. A full-thickness flap was reflected, and a significant gain in buccal bone width was observed with the implant being fully encased in bone (Figure 23). The keratinized gingiva on the ridge was transferred to the buccal aspect of the healing abutments (Figure 24). Next, implant crowns were fabricated for sites Nos. 4 and 5 (Figure 25).
DISCUSSION
The individual steps used for the combination technique were selected for their ease of use and predictability, as reported by the literature. When deciding on flap design, it is important to understand that the literature is not conclusive as to whether a partial- or full-thickness flap should be utilized. Bassetti et al11 found that there is a risk of an unpredictable buccal plate if a full-thickness flap is elevated when treating patients with 3 mm of ridge width. After healing, the ridge-split technique leaves less than 1.5 mm width of buccal plate, which is an insufficient amount of bone for long-term success of anterior maxillary implants. Our technique of full thickness, in combination with split thickness, allows for the additional grafting of the deficient ridge in the more severe cases. The extent of the full-thickness flap should be designed after the evaluation of CBCT and the clinical assessment. In many cases, the maxillary ridge widens toward the base, so the base does not require additional grafting. The split-thickness flap would maintain the blood supply to the ridge, thereby preventing unwanted resorption.
The use of PIEZOSURGERY (Mectron) has been reported to be advantageous compared to other splitting techniques. Its benefits include precise cutting and safety, a bleeding-free surgery site, selective cutting of hard tissue without damage to soft tissue, faster bone regeneration, a faster healing process, a decrease in post-op pain, and reduced traumatic stress to the patient because of its quiet operation.
Different expansion techniques and instruments are available today. Osteotomes have been documented to provide expansion in a controlled manner without the removal of bone and with increased bone density for better primary stability of implants. An additional benefit of osteotomes is that the projection from the surgical site helps in visualizing the implant’s emergence in all directions. The systematic review by Jha et al12 in 2017 showed that osteotomes are widely used and documented in ridge-split procedures.
The type of bone grafts and membranes used in the literature vary widely. While there is no preference for one product over another, we do recommend using a cortical allograft or xenograft on the buccal to achieve a longer replacement time and maintenance of ridge width for the future.
Membrane stabilization techniques utilizing tacks or stabilizing sutures have been shown to improve containment and immobilization of the bone graft, a very critical aspect of ensuring predictable and successful GBR. Periosteal sutures are beneficial in ridge-split cases since they do not require a second procedure for their removal while, at the same time, providing great membrane stabilization and graft containment.
The use of growth factors may enhance the healing and maturation of the bone in split-ridge procedures. Using allograft in combination with recombinant human platelet-derived growth factor BB (rhPDGF-BB) has been documented by Chiang et al13 in 2014 to provide these enhanced results.
Overall, all these combination techniques will enhance surgical outcomes and long-term success for ridge-split procedures.
CONCLUSION
The schematics and case report present a technique to maximize success for horizontal ridge splitting in the maxilla. Research has clearly demonstrated that guided bone regeneration is necessary to ensure buccal thickness in the area of expansion. These case reports highlight how a combination of techniques needs to be incorporated to achieve optimal results with ridge-split expansions. Decisions need to be made, starting with the flap design. A combination full-thickness flap/split-thickness flap is recommended to prevent ridge resorption as well as to aid in coronal grafting and stabilization of the membrane to the periosteum for successful GBR. The use of a piezo surgical unit provides safety as well as a better healing response. Tapered osteotomes allow for maintaining parallelism as well as providing osseodensification to the osseous ridge. Bone grafting with or without growth factors will aid in maintaining or increasing ridge width. The combination technique described can aid the clinician in treating areas of the mouth with narrow ridge anatomy and to achieve predictable results. Additional long-range follow-up studies are needed.
REFERENCES
1. Elnayef B, Monje A, Lin GH, et al. Alveolar ridge split on horizontal bone augmentation: a systematic review. Int J Oral Maxillofac Implants. 2015;30(3):596-606. doi:10.11607/jomi.4051
2. Tan WL, Wong TL, Wong MC, et al. A systematic review of post‐extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23:1-21. doi:10.1111/j.1600-0501.2011.02375.x
3. Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post‐extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048–58. doi:10.1111/j.1600-051X.2009.01482.x
4. Tatum Jr H. Maxillary and sinus implant reconstructions. Dent Clin N Am. 1986;30(2):207–29.
5. Scipioni A, Bruschi GB, Calesini G. The edentulous ridge expansion technique: a five-year study. Int J Periodontics Restorative Dent. 1994; 14(5):451–9.
6. Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associate with a split crest technique and guide tissue regeneration. Int J Periodontics Restorative Dent. 1992;12(6):462–73.
7. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium (Newtown, Pa.). 1994;15(2):152–4.
8. Vercellotti T. Piezoelectric surgery in implantology: a case report—a new piezoelectric ridge expansion technique. Int J Periodontics. 2000;20(4):358–65
9. Mestas G, AlarcoÂn M, Chambrone L. Long-term survival rates of titanium implants placed in expanded alveolar ridges using split crest procedures: a systematic review. Int J Oral Maxillofac Implants. 2016;31(3):591–9. doi:10.11607/jomi.4453
10. Nguyen V, von Krockow N, Weigl P, et al. Lateral alveolar ridge expansion in the anterior maxilla using piezoelectric surgery for immediate implant placement. Int J Oral Maxillofac Implants. 2016;31:687–99. doi:10.11607/jomi.4214
11. Bassetti MA, Bassetti RG, Bosshardt DD. The alveolar ridge splitting/expansion technique: a systematic review. Clin Oral Implants Res. 2016;27(3):310–24. doi:10.1111/clr.12537
12. Jha N, Choi EH, Kaushik NK, et al. Types of devices used in ridge split procedure for alveolar bone expansion: a systematic review. PLoS One. 2017;12(7):e0180342. doi:10.1371/journal.pone.0180342
13. Chiang T, Roca AL, Rostkowski S, et al. Reconstruction of the narrow ridge using combined ridge split and guided bone regeneration with rhPDGF-BB growth factor-enhanced allograft. Int J Periodontics Restorative Dent. 2014;34(1):123–30. doi:10.11607/prd.1633
ABOUT THE AUTHORS
Dr. Kim is an adjunct clinical assistant professor and former chief resident in the department of periodontics at the Rutgers School of Dental Medicine (RSDM) in Newark, NJ. He is in private practice in Flushing, NY. He can be reached at jasonkimdds@gmail.com.
Dr. Lerer is a former resident in the department of periodontics at RSDM. He is a periodontist with the US Navy in North Carolina. He can be reached at chananlerer@gmail.com.
Dr. Murawski is a former resident in the department of periodontics at RSDM. He is in private practice in New Jersey. He can be reached at murawskidmd@gmail.com.
Dr. Drew is vice chairman and a professor in the department of periodontics at RSDM. He can be reached at drewhj@sdm.rutgers.edu.
Dr. Cappetta is PG director and an assistant clinical professor in the department of periodontics at RSDM. He can be reached at cappeteg@sdm.rutgers.edu.
Disclosure: The authors report no disclosures.



