Atrophic ridges present some unique challenges to the surgical placement of dental implants. Patients today often request fixed prostheses to replace their failing or missing teeth. Conventional options exist, including fabrication of conventional, removable complete dentures or more advanced therapy, such as palateless implant-retained overdentures. When attempting a design so that the patient can function without removal, the amount of available hard tissue becomes paramount. Height, width, and density of available hard tissue must clearly be evaluated, as well as the position of vital anatomic landmarks. There can be no assumption that every patient can receive fixed implant prostheses without some invasive treatment to build or maintain bone to allow for proper dental implant integration and to support the final prosthesis.
Oral and maxillofacial complications often arise when there is inadequate hard tissue to perform routine implant surgery. Autogenous bone grafting is one procedure that provides width and potentially height to an edentulous situation but requires that the patient place no pressure on the invasive surgical and donor sites. This often means that the patient must remain edentulous during the initial healing time.1 Even in the age of COVID-19 and the requirement for mask use, this can be difficult for any patient to tolerate during the extensive integration period.
Here we will describe a positive treatment modality that actually expands the alveolar ridge when there is a significant horizontal bone defect. This alveolar ridge-split technique is completed using a piezotome (Piezotome CUBE [ACTEON]). The facial plate of the maxilla tends to resorb more than the palatal plate. This results in a sagittal disharmony. By ridge splitting the available arch form, the available hard tissue is expanded rather than removed.2-4 This provides access for dental implants to be precisely positioned, maintaining an appropriate amount of facial and palatal bone. The implant placement could not be achieved without this process unless significant bone grafting was completed, either prior to implant insertion or as an immediate implant protocol, to protect the facial aspect of the implant threads. The goal with the piezotome is to bend the facial plate, avoiding any fracture. The tips used with this particular piezotome are specifically designed with a square-like shape with a sharpened tip. This provides for the accurate creation of a trough. Progressively larger tips are used to widen and expand the bone.5,6
A clean full-thickness mucoperiosteal incision is made to the atrophic ridge with a releasing vertical incision made at the midline. This exposes the entire atrophic ridge. Two vertical oblique osteotomies are made mesial and distal to the desired implant position. This acts similarly to a dishwasher door. The tips of the piezotome are clearly marked in 2-mm increments, which is helpful in determining the depth we wish to achieve. The instrument provides a greenstick-like movement of the facial plate of bone as the implant is torqued to depth. The implants are placed, and the trough that was created is filled in with allograft material (Newport Biologics, Glidewell Lab) that is wetted with sterile saline. The material was covered here with a platelet-rich fibrin (PRF) membrane and a resorbable membrane (Newport Biologics). The implants were initially stabilized with adequate facial and palatal bone support. The piezotome here provided accuracy, safety, and comfort in achieving the desired result—more so than when using a chisel and hammer or a high-speed bur to create the trough for implant placement.
Ridge splitting is indicated where there is compromised hard-tissue width for appropriate dental implant placement. Both the facial and palatal cortical plates are visible through CBCT analysis (Green CT [Vatech America]). No significant undercuts are present. The facial bone is repositioned to provide better stability of the implant and improved aesthetics of the final prosthesis. It is necessary to have 3 mm or more of horizontal width to do this technique.7 When possible, the piezotome makes surgical osteotomies simpler for the practitioners and provides comfort to the patient due to the creation of fewer force stresses.
The piezotome’s frequency ranges between 28 and 36 kHz. The tips are active only on hard tissue, which limits the risk of any soft-tissue injury. The ultrasonic vibrations are said to allow tissue relaxation and optimal cell repair for a clean incision and improved healing.6 Thus, the cut created is free of friction and vibration. Studies have indicated an absence of necrosis as osteocytes remain viable.
The protocol used with the Piezotome CUBE is simple and precise. As the soft tissue is reflected to visualize the available bone, the first CS1 ultrasonic tip is used to a depth of approximately 8 mm. There are clear 2-mm markings on each tip. Lateral expansion is continued using the next size ultrasonic tip (CS2). A third tip (CS3) is then used to create the facial relief on the mesial and distal aspects of the surgical site.8,9 Bone expansion can be continued depending on the amount of available width of hard tissue. Next, create a site for the immediate torqueing of dental implants. The gaps created between the implants are filled with allograft material.
This graft material is protected from invagination of epithelium by using PRF membranes. These membranes are created by simply drawing blood from the patient and spinning it under a specific protocol using a centrifuge (Salvin Dental). This PRF material is helpful in bone preservation and new bone turnover. It accelerates the biological processes, resulting in bone regeneration in the defect areas. It is an excellent tool in helping to create adequate bone height and width in this atrophic area. Healing is presumed to be faster, which increases bone attachment around our dental implants and reduces infection.10-12
Following ridge splitting and dental implant placement, an inflammatory response occurs, which results in vasodilation, plasma and leucocyte seepage, and cell addition that helps in the phagocytosis of cellular and tissue macrophages. Angiogenesis and the formation of blood clots containing platelets are noted. The revascularization gives nutrients to the cells, which results in their proliferation.9 As trauma to the site is reduced, the site has a better chance to integrate, and the prognosis increases.
When available bone in an arch is limited, proper, predictable placement of dental implants is challenged. Grafting procedures may allow regeneration of hard tissue where deficiencies exist. Autogenous bone, taken from the patient’s own body, is often considered to give the most predictable results. However, this material must be taken from a donor site, which makes the technique more invasive. Allograft materials, which are harvested from human donors, have become popular. No secondary surgical site is required. Cortico/cancellous mixed allograft is fabricated as bone is ground down to cortical and cancellous particulate and then processed to eliminate disease transmission and antigenic responses. This material is osteoconductive, providing a matrix for eventual regeneration. As demineralization occurs, the organic collagen matrix remains, which exposes bone morphogenic proteins. These growth factors are what controls the differentiation of progenitor cells to osteoprogenitor cells and eventual bone and cartilage creation.4 Cortical particles maintain space during the regeneration process, and the cancellous particles remodel quicker. Epithelium grows significantly faster than bone, so any graft material must be protected to allow for increased bone replacement.1
A popular treatment modality that many patients request today involves “All-on” screws or cement on fixed dental implant prostheses. This is often referred to as the best mode of treatment, which best mimics natural tooth function. Dentures and implant-retained overdentures provide an important role in our dental tool chest, but when patients intend to invest in non-removable appliances, anatomic considerations need to be addressed.
CBCT analysis using the PaX-i3D Green (Vatech America) can initially determine the amount of available hard tissue and vital anatomy we are dealing with.13,14 Then 3D Diagnostix (3DDX) software is used to determine the actual amount of available bone and precisely aids in virtually placing the appropriate dental implants. The final prosthesis can also be designed. Implant position is determined prior to any surgical intervention. Undercuts, nerves, and the height and width of the residual ridge are all considered. To ensure ideal implant positioning prior to any surgical intervention, CBCT analysis of the patient’s properly seating conventional denture is done. The intaglio surface must rest completely on the palatal tissue. The patient’s denture is scanned separately with radiopaque markers and again within the patient’s mouth. This protocol will allow for approximation of final tooth position and any access hole positioning or purposeful draw of custom-milled abutments. From the virtual CBCT diagnosis, a surgical guide is fabricated to aid in the eventual positioning of the implants in the available hard tissue. Osteotomy angulation, depth, and width are predetermined using this accurate surgical guide. After integration of the implants, an initial impression is made with implant-level impression copings. Here, a polyvinyl siloxane material (Kettenbach LP) is used. There are several methods to retain the final implant-retained prosthesis. Multiunit abutments are chosen by the dental laboratory to allow for access holes to be formed on the palatal aspect of a screw-retained maxillary prosthesis. A second protocol involves fabricating custom titanium abutments to support a cement-on implant bridge. Regardless, accuracy and a passive fit are paramount to the longevity of the underlying implants and prosthesis. Aesthetics is determined using a standard denture teeth setup over a screw-retained, stable record base. Once form and function are established, the laboratory can create what is referred to as a “smile composer,” or PMMA.15,16 This transitional appliance is used to check proper occlusion, speech, and aesthetics. Once this transitional appliance is accepted, the dental laboratory will mill the final BruxZir zirconia (Glidewell) implant-retained prosthesis. This material is fracture- and wear-resistant. Interarch distance is always considered and should be evaluated carefully prior to promising the patient this mode of therapy.17
Realizing the advantages and disadvantages of certain dental implant protocols is a critical part of the success of our treatment and is truly the “art of dentistry” today. When implant integration is complete, and they are properly positioned, prosthetic construction is maximized.
CASE REPORT
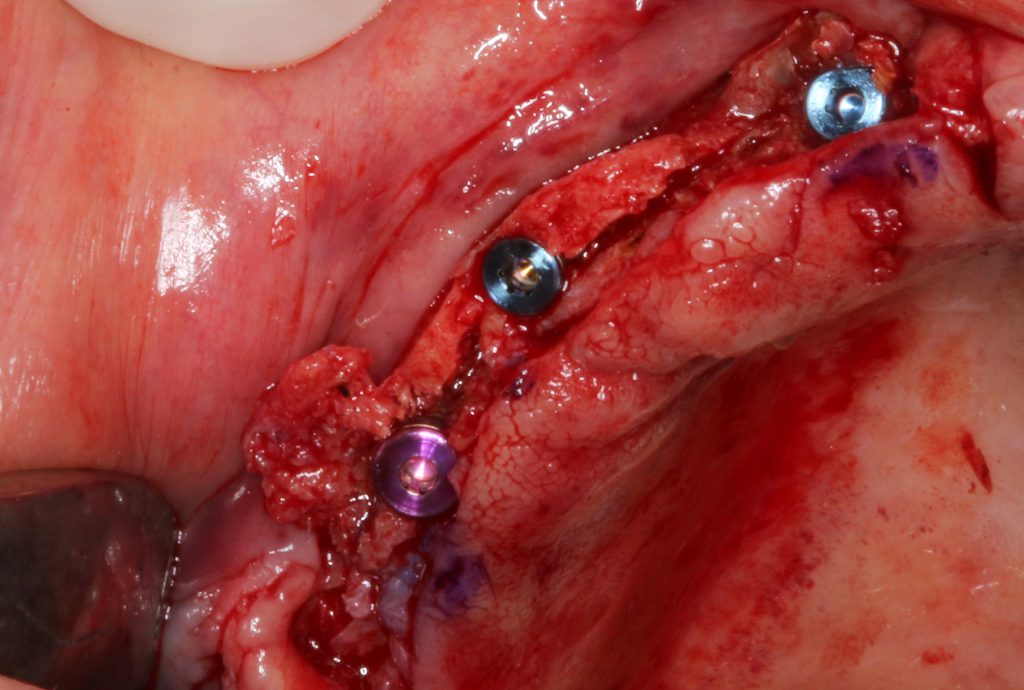
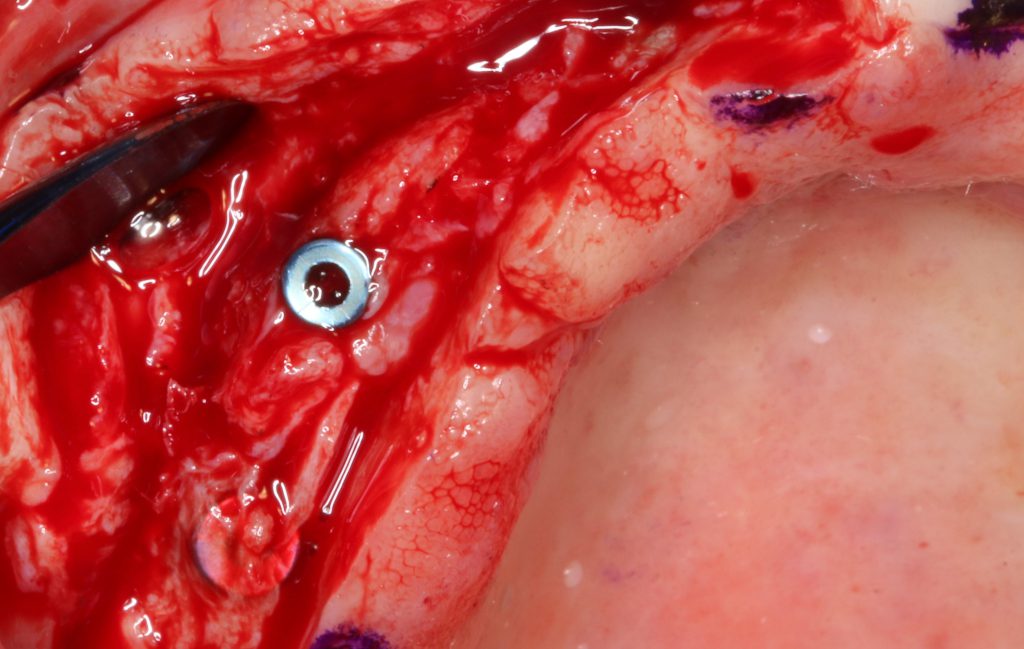
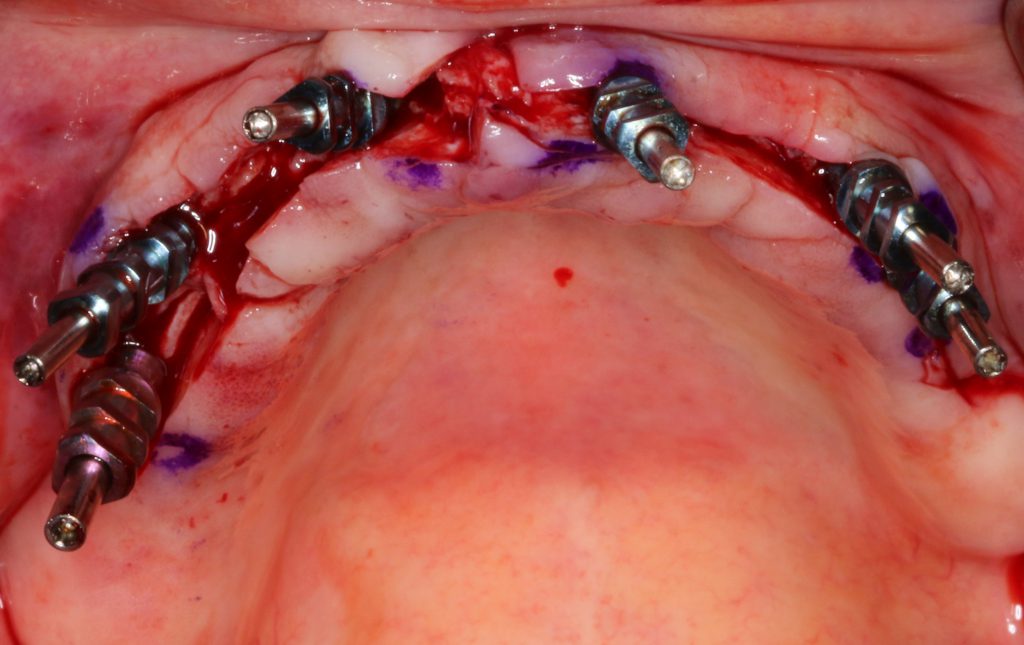
Our patient was a 67-year-old female who had worn a conventional maxillary complete denture for many years. Although the denture served some function, the patient elected to consider a fixed bridge (Figure 1). Figure 2 illustrates what appeared not only to be adequate vertical height of bone to accept dental implants in proper position but significant horizontal bone shrinkage as well. In diagnosing this case, CBCT analysis was used to determine the amount of horizontal bone. Her existing denture, which fit well on the intaglio surface, was used with radiographic markers to determine final implant angulation, depth, and position within the arch (Figure 3). Using this CBCT system as a diagnostic tool, it was apparent that there was only minimal bone available. Using the 3DDX software, it was determined that 6 dental implants could be precisely placed in the edentulous maxilla (Figure 4). Venous blood was drawn and spun to create PRF membranes. The attached gingiva was reflected to expose the available hard tissue, which was thin. The coronal portion of bone was flattened (Figure 5). To expand the facial and palatal bone, a Piezotome CUBE was used to trough the tissue precisely to a depth of 8 mm (Figures 6 and 7). Following the Hahn Dental Implant System (Glidewell) surgical placement protocol, a 2.4-mm-diameter pilot bur created the proper depth for implant placement. The implants were then torqued into the prepared osteotomies and formed using the trough created by the Piezotome CUBE (Figure 8). Allograft (Newport Biologics) was wetted with sterile saline and carried to the facial aspect of the surgical site, filling the trough created by the Piezotome CUBE (Figure 9). The graft repair was protected by using the PRF membrane created (Figure 10). The surgical site was sutured using Vicryl (Newport Biologics). A postoperative CBCT analysis showed the implant in place with the facial and cortical bone intact (Figure 11). The surgical guide used to aid in the surgical angulation and depth of the implants was used to determine their buried positions under the healed maxillary arch using an indelible marker (Figure 12). I elected to reflect the soft tissue here to illustrate the adequacy of the facial plate of bone integrated around the surgically placed implants (Figure 13). Impressions were made using an open tray concept (Figure 14), and radiographs were made to ensure proper seating of the impression copings (Figure 15). The dental laboratory (Glidewell) created custom titanium abutments to support a fixed, cement-on implant-retained zirconia bridge (BruxZir) (Figures 16 and 17). The patient was restored to function and was pleased with the final aesthetic result (Figures 18 and 19).















CONCLUSION
Full-arch, implant-retained prostheses are a popular method of transitioning the patient from the frustrations of edentulism and the need for removable appliances. Being able to predictably create a stable and integrated means to support a fixed or fixed/detachable prosthesis can be challenging for the dental surgeon. Understanding vital anatomy and available hard tissue, as well as the density of the bone, can be done using reliable CBCT analysis and CAD/CAM design. This modern technology allows the practitioner to visualize the finished case prior to any surgical intervention. Most importantly, it allows us to choose cases that are possible and those that may require more invasive surgical treatment. Autogenous block grafting to establish viable height and width of bone is one method. Here, we discussed the use of ridge-splitting techniques to maintain facial and palatal cortical bone while immediately placing dental implants. These implants integrate well and are restored using prepared custom titanium abutments, which allow the final implant-retained prosthesis to rest passively with stability. The increased function and aesthetics are appreciated by our patients.
REFERENCES
1. AlGhamdi AS, Shibly O, Ciancio SG. Osseous grafting part I: autografts and allografts for periodontal regeneration–a literature review. J Int Acad Periodontol. 2010;12(2):34-8.
2. Moro A, Gasparini G, Foresta E, et al. Alveolar ridge split technique using piezosurgery with specially designed tips. Biomed Res Int. 2017;2017:4530378. doi:10.1155/2017/4530378
3. Bassetti MA, Bassetti RG, Bosshardt DD. The alveolar ridge splitting/expansion technique: a systematic review. Clin Oral Implants Res. 2016;27(3):310-24. doi:10.1111/clr.12537
4. Bassetti R, Bassetti M, Mericske-Stern R, et al. Piezoelectric alveolar ridge-splitting technique with simultaneous implant placement: a cohort study with 2-year radiographic results. Int J Oral Maxillofac Implants. 2013;28(6):1570-80. doi:10.11607/jomi.3174
5. Vercellotti T, Stacchi C, Russo C, et al. Ultrasonic implant site preparation using piezosurgery: a multicenter case series study analyzing 3,579 implants with a 1- to 3-year follow-up. Int J Periodontics Restorative Dent. 2014;34(1):11-8. doi:10.11607/prd.1860
6. Stübinger S, Stricker A, Berg BI. Piezosurgery in implant dentistry. Clin Cosmet Investig Dent. 2015;7:115-24. doi:10.2147/CCIDE.S63466
7. da Silva Neto UT, Joly JC, Gehrke SA. Clinical analysis of the stability of dental implants after preparation of the site by conventional drilling or piezosurgery. Br J Oral Maxillofac Surg. 2014;52(2):149-53. doi:10.1016/j.bjoms.2013.10.008
8. Majewski P. Autogenous bone grafts in the esthetic zone: optimizing the procedure using piezosurgery. Int J Periodontics Restorative Dent. 2012;32(6):e210-7.
9. Magrin GL, Sigua-Rodriguez EA, Goulart DR, et al. Piezosurgery in bone augmentation procedures previous to dental implant surgery: a review of the literature. Open Dent J. 2015;9:426-30. doi:10.2174/1874210601509010426
10. Borie E, Oliví DG, Orsi IA, et al. Platelet-rich fibrin application in dentistry: a literature review. Int J Clin Exp Med. 2015;8(5):7922-9.
11. Miron RJ, Xu H, Chai J, et al. Comparison of platelet-rich fibrin (PRF) produced using 3 commercially available centrifuges at both high (~700 g) and low (~200 g) relative centrifugation forces. Clin Oral Investig. 2020;24(3):1171-1182. doi:10.1007/s00784-019-02981-2
12. Miron RJ, Zucchelli G, Pikos MA, et al. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig. 2017;21(6):1913-1927. doi:10.1007/s00784-017-2133-z
13. Misch, CE. Dental Implant Prosthetics. 2nd ed. Mosby Inc; 2015.
14. Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol. 2012;38(3):298-307. doi:10.1563/AAID-JOI-D-10-00146
15. Kosinski TF. Implant-retained, solid zirconia full arch reconstruction: what our patients are asking for. Inside Prosthodontics. May 2019. 42-52.
16. Kosinski TF. Dental implant hybrids for maximum esthetics. Inside Dentistry. May 2015. 74-80.
17. Kosinski TF. Creation of the bruxzir hybrid to increase form and function. The Profitable Dentist. Summer 2019. 56-59.
ABOUT THE AUTHORS
Dr. Kosinski received his DDS degree from the University of Detroit Mercy School of Dentistry (Detroit Mercy Dental) and his Mastership in Biochemistry from the Wayne State University School of Medicine. He is an affiliated adjunct clinical professor at Detroit Mercy Dental; serves on the editorial review board of REALITY, the information source for aesthetic dentistry; and is the past editor of the Michigan Academy of General Dentistry Update. He is currently the editor of the AGD journals General Dentistry and AGD Impact and is the editor of Implants Today in Dentistry Today. He is a past president of the Michigan AGD. He is a Diplomate of the American Board of Oral Implantology/Implant Dentistry, the International Congress of Oral Implantologists (ICOI), and the American Society of Osseointegration. He is a Fellow of the American Academy of Implant Dentistry and received his Mastership in the AGD. He can be reached at drkosin@aol.com.
Dr. Tilley received her DMD degree at the University of Alabama School of Dentistry. She is a native of Pensacola, Fla, and has been practicing dentistry in her hometown since 1998. She keeps up with the latest in dentistry by attending continuing education seminars on topics such as oral surgery, implants, veneers, periodontal disease, cosmetic procedures, and much more. Dr. Tilley has also done extensive training at the Las Vegas Institute for Advanced Dental Studies and the Engel Institute with Drs. Timothy Kosinski and Todd Engel, respectively. She is a Fellow of the International College of Dentists (ICD) and is a member of the AGD, the ADA, the Florida Dental Association, the Alabama Dental Association, the Academy of Laser Dentistry, and the Academy of American Facial Esthetics. Dr. Tilley has received Fellowships with the ICOI and the ICD. Most recently, Dr. Tilley was inducted into Fellowship in the Academy of Dentistry International and the American College of Dentists. She can be reached via email at stephflynntilley@cox.net.
Disclosure: The authors report no disclosures.


