A Complete Digital Workflow in Two to Three Patient Visits
INTRODUCTION
A very large population exists in the United States with at least one edentulous dental arch. More than 36 million Americans are completely edentulous.1 In addition to that, a significant segment of the population has failing complete dentitions. These patients, when seeking care, are most commonly found in the general dentist’s office. The fixed, implant-supported, full-arch restoration has been found to provide a measurable improvement in quality of life for the edentulous patient2 as well as having long-term survival rates.3,4 As dental professionals and dental care providers to the general public, it is our responsibility to provide appropriate care to this patient population. However, the restorative procedures required to complete a full-arch, implant-supported restoration can be complex, require expertise in the procedure, and have workflows with 5 or more appointments. Any of these conditions may be an obstacle to an implant-supported, full-arch restoration being recommended or performed.5
The digital age in dentistry has introduced technology that offers the possibility of simplified and shortened workflows for the full-arch, implant-supported restoration.6,7 There have been limitations to the possibility of a complete digital workflow for full-arch, implant-supported restorations due to the design of scan bodies, utilization of correct scan paths, and machining tolerances, resulting in inaccurate positioning of implants or abutments in virtual models.8-13
A technology called Nexus iOS was introduced to the North American dental community in April of 2022 by the Keystone Dental Group. The solution was developed and is currently supported by the Osteon Medical Corporation, a subsidiary company of the Keystone Dental Group. It offers a simple, predictable solution for the full-arch implant patient. Created to simplify the restorative, full-arch, implant-supported restoration procedure, it eliminates complex technical steps and the need for expensive equipment, and reduces the number of appointments required to complete an implant-supported, full-arch, fixed restoration—all while increasing the level of accuracy and predictability of the restoration.14-16 The Nexus workflow completes the restorative procedure for a full-arch, implant-supported restoration in as little as 2 to 3 appointments and is an open solution available for most implant systems.17,18
The solution was carefully developed, examining the technology of existing intraoral scanners; the way the current algorithms capture scan body data; the way the current CAD software analyzes and uses that data; the mechanical and aesthetic requirements of a full-arch, implant-supported restoration; the mechanical properties of the materials used in these restorations; and clinical and laboratory workflows currently used to complete this type of restoration. Analyzing all this data, a full-arch, implant-supported solution was developed and tested and has already been used to restore more than 60,000 implants. The solution includes intraoral scanning, the rethinking and redesigning of scan bodies, and control of the scan path. Artificial intelligence algorithms are infused throughout many of the processes. It includes applications that validate impression accuracy in real time, before the patient leaves the operatory, and the digital transfer of all data. There are also laboratory artificial intelligence algorithms that validate and improve the accuracy of collected scan data, artificial intelligence-empowered design of the supporting structure of the restoration, and ultra-precision machining and validated complex protocols that ensure delivery of predictable, precise restorations.
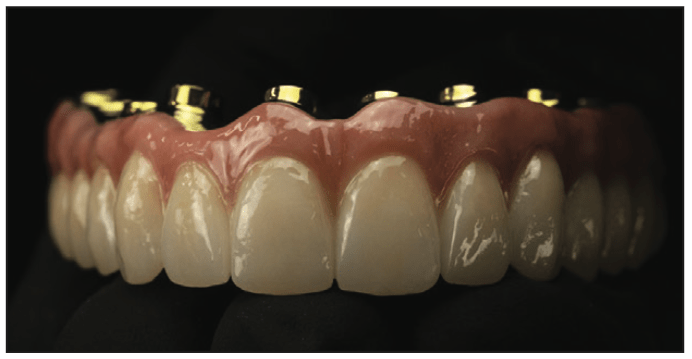
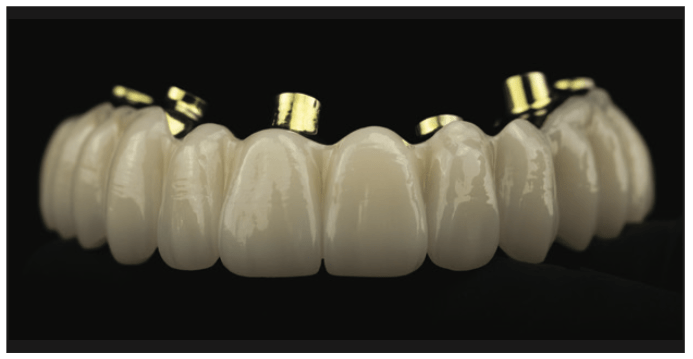
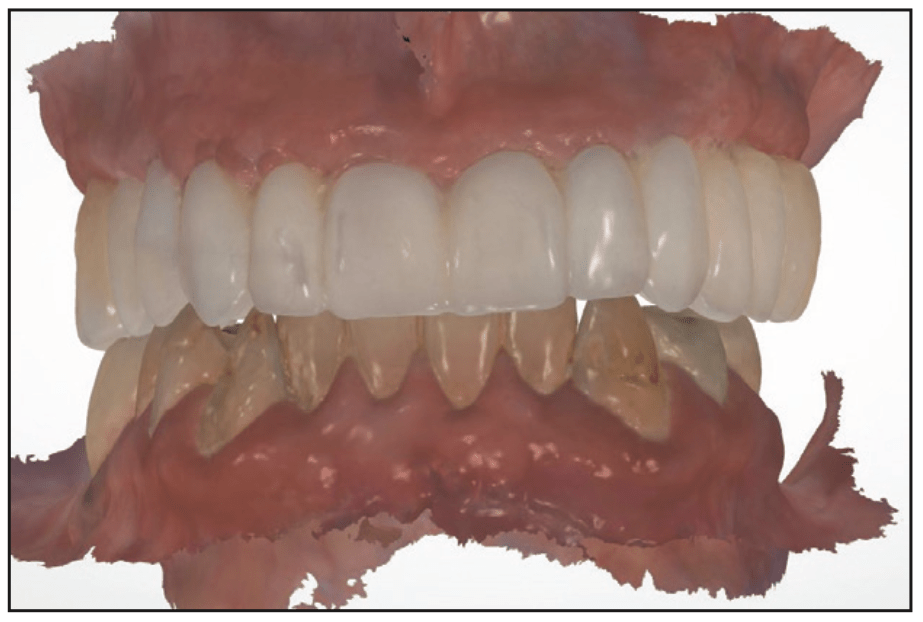
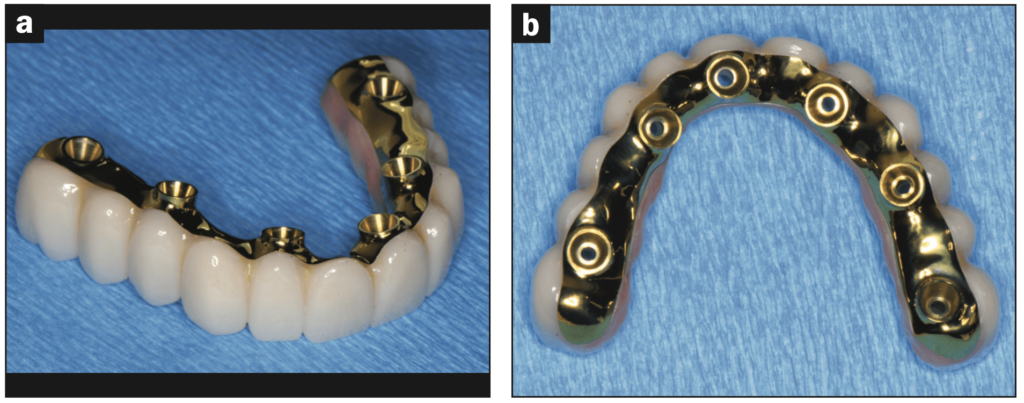
The restoration design is based on a precision-milled titanium framework that sits accurately on multi-unit abutments. There are no Ti-bases, so there are no issues of Ti-base delamination. A monolithic zirconia overlay with or without layered porcelain or an acrylic wraparound completes the prosthesis design. The Nexus prosthesis may be designed as an FP-3 restoration (pink apron) (Figure 1) or an FP-1 design restoration (crown and bridge design) (Figure 2). Only 6 to 8 mm of restorative space is required for the Nexus prosthesis,19 which minimizes the requirement of bone reduction that is frequently needed for restorations requiring 12 to 15 mm of restorative space.20,21
These procedures were developed to produce predictable, passively seating, full-arch, implant-supported restorations to an accuracy of sub-10-µm average linear deviation in a simple 2-to-3-appointment, completely digital workflow.14,15
The workflow is non-complex, requiring a conventional intraoral scanner and a Nexus scan gauge kit (Figure 3). The Nexus restoration is designed to seat on multi-unit abutments. Most currently used multi-unit abutments in North America can be used for the Nexus solution.

There are workflows for the patient with a fixed provisional restoration on multi-unit abutments as well as workflows for patients with removable prostheses seated over multi-unit abutments.
CASE REPORT
A 71-year-old male patient presented for evaluation and treatment of his maxilla (Figure 4). A complete evaluation of the patient was made, including his chief complaint, past medical history, intraoral evaluation, full-mouth series x-rays, IOS scans, CT scans, and photographs. Evaluation of all collected data found extensive caries, dry mouth, fractured teeth, and missing teeth. A treatment plan for extraction of all maxillary teeth, followed by implant placement; immediate provisionalization on the immediate implants; and a full-arch, implant-supported final restoration, was presented and accepted by the patient.
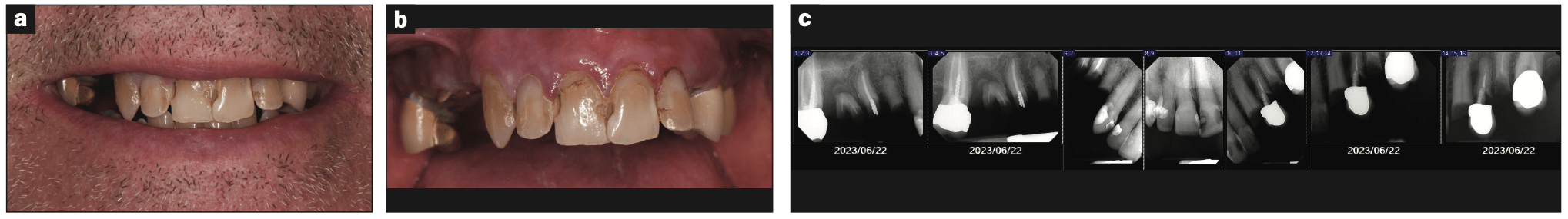
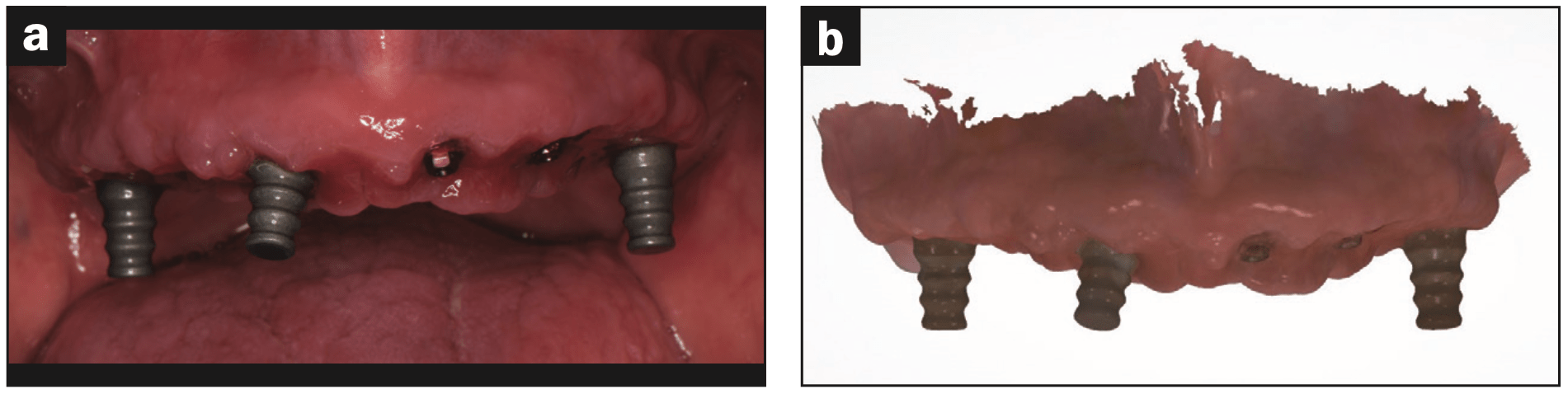
Preparation for surgery included a finalized virtual diagnostic wax-up of the proposed restoration and a CT-designed surgical plan with 3D printed surgical guides for implementation. On the day of surgery, the maxillary teeth were extracted, and Keystone Genesis Active implants were placed and immediately provisionalized with a fixed, screw-retained, provisional restoration supported by Genesis Active multi-unit abutments (Figure 5). Following a 6-month healing period (due to the patient’s long-term steroid usage), the Nexus iOS restorative procedures began (Figures 6 and 7). The Nexus iOS workflow was followed.


Appointment 1
Intraoral scans were taken of the existing teeth and restorations in the patient’s mouth, including the maxilla, mandible, and bite. These are called foundation scans (Figure 8). The foundation scans are utilized to establish vertical dimension and centric occlusal position. If excursive movements are designed into the provisional restoration, these can be copied. The foundation scans are a starting point for restoration design.
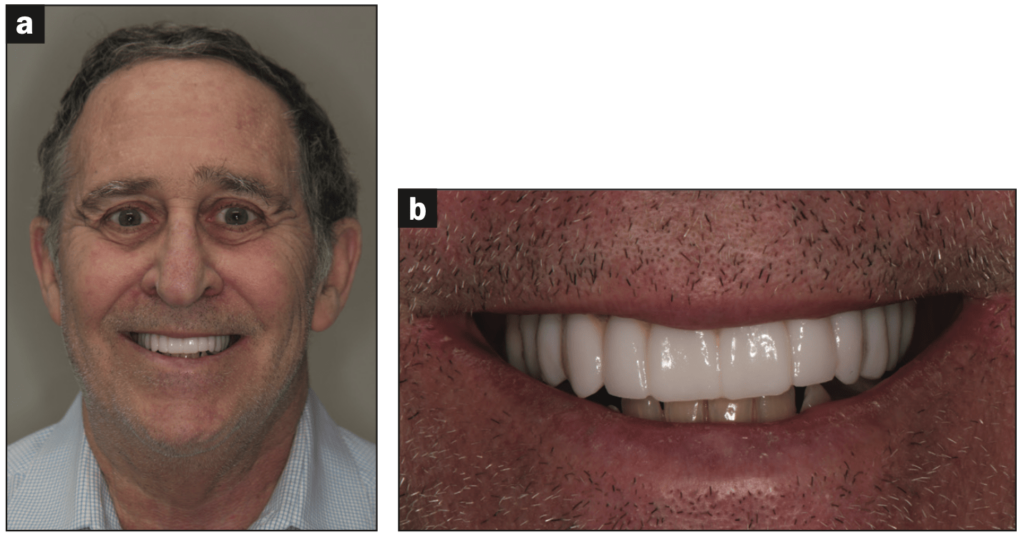
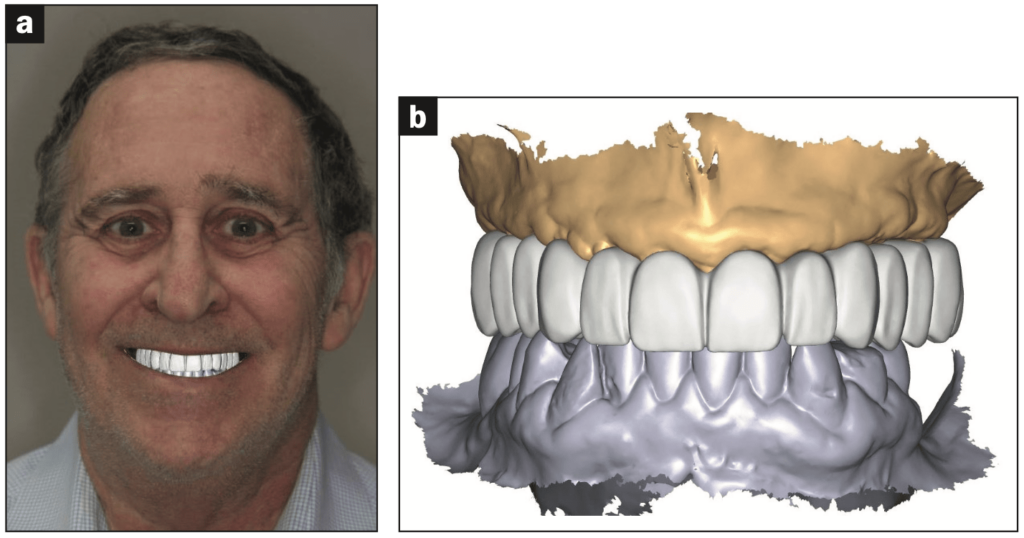
Full-face and close-up smiling photographs were taken with the provisional restoration in place (Figure 9).
The provisional restoration was removed. Three narrow scan bodies (included in the Nexus scan gauge kit) were placed on the multi-unit abutments in as wide of an anterior to posterior spread as possible. The arch was scanned to include all multi-unit abutments, with and without narrow scan bodies, and their surrounding soft tissues. The emergence profile scan that was used to create an accurate design of the intaglio surface and the emergence profile of the restoration is seen in Figure 10.
Three analog scan bodies (from the Nexus scan gauge kit) were attached to the provisional restoration in as wide an anterior-posterior spread as possible (Figure 11). These positions did not need to correspond to the positions used in the emergence profile scan. The provisional was now scanned 360° extraorally. This scan was used to establish vertical dimension, a centric occlusal relationship of the mandible to maxilla, and a starting point for prosthesis design.
The last set of scans taken were to record the multi-unit position. The narrow scan gauges were removed from the multi-unit abutments. Nexus scan gauges were positioned on the multi-unit abutments following the Nexus scan gauge positioning protocol. These rules include having the scan gauges overlap each other. The scan gauges are in close proximity but not touching each other. The scan gauges are placed in close proximity to the soft tissue—but without pressure on the soft tissue. Lastly, the scan gauges should be placed in the same horizontal plane when possible (Figure 12).
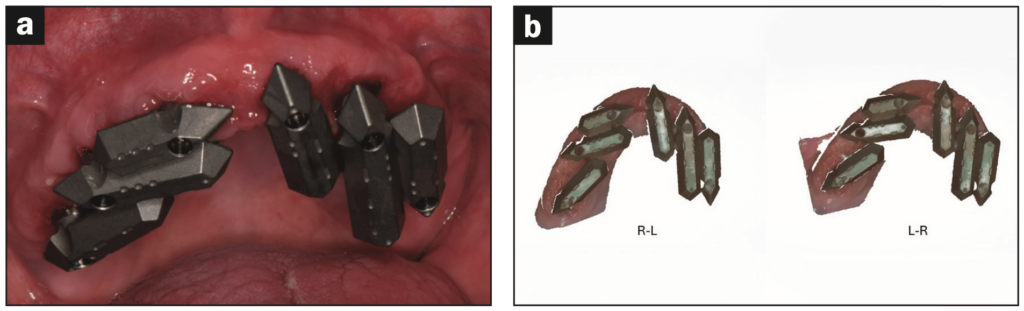
The scan path is easy but critical to follow. When scanning the Nexus scan gauges, a single smooth pass over the scan gauges in one direction (right to left) is the required scan path. This single scanning pass is repeated in the opposite direction (left to right) as a separate scan.
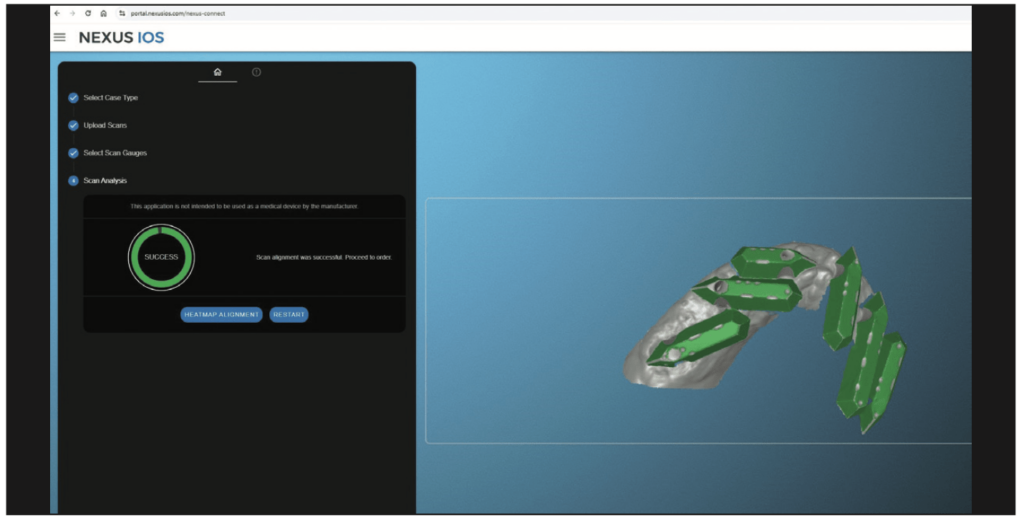
Before removing the scan gauges, a desktop application on the scanner desktop called Nexus Connect was opened. This application ensures that when the restoration is delivered, it will predictably passively seat on the multi-unit abutments. The 2 Nexus scan gauge scans were imported into the Nexus Connect application, and in seconds, the application verified that the scans that were taken accurately recorded the multi-unit abutment positions (Figure 13). If the scanning was not accurate, the Nexus Connect would indicate which scan gauges created an inaccurate recording, possibly due to a loose multi-unit screw retaining the scan gauges or something such as blood or debris on the scan gauges. After a quick evaluation of the problem scan gauge and correction, a new scan would be taken, requiring less than one minute.
All of this data was sent from the IOS to Osteon Medical, and photographs were uploaded to the Nexus iOS portal. The digital prescription was completed in the portal.
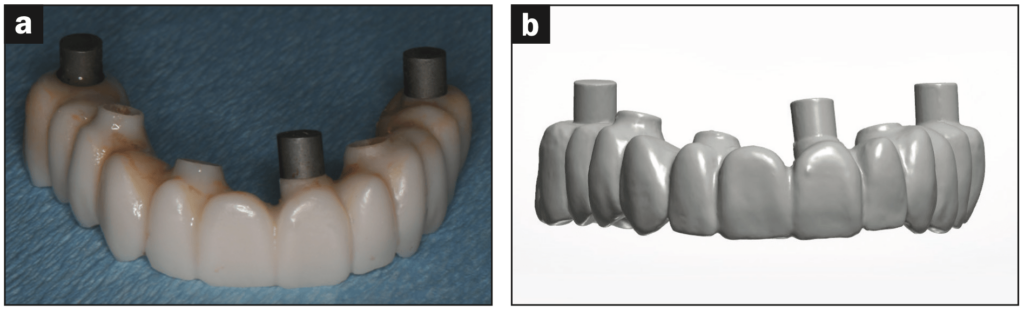
Three days later, an email was received requesting approval of the prosthesis design. In the email, an exocad application was opened showing the prosthesis design in 3D (Figure 14). The STL file of the design was downloaded from this email and 3D printed in our office.
Appointment 2
The patient was appointed and came in for a try-in and evaluation of aesthetics, phonetics, occlusion, and overall prosthesis design. Attention was paid to emergence profile and soft-tissue proximity (Figure 15). The patient gave his approval, and the prosthesis design was approved in the Nexus iOS portal.
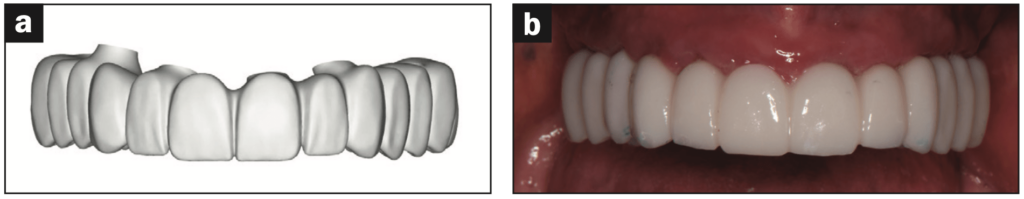
Fifteen working days later, the Nexus final prosthesis arrived in our office (Figure 16).
Appointment 3
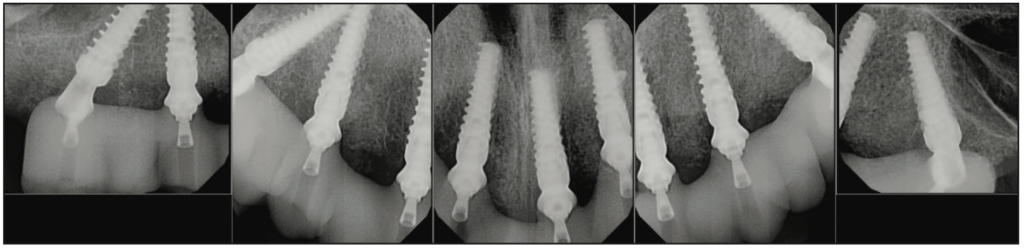
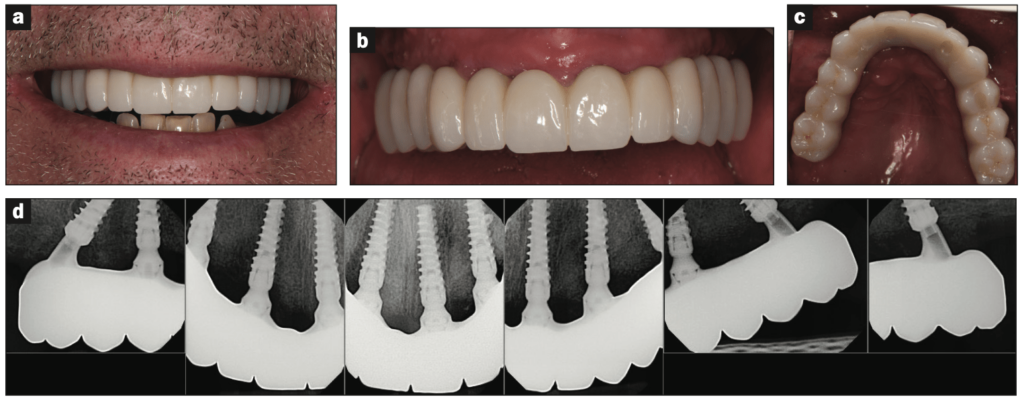
The patient came in for his appointment, and the restoration was tried in. A Sheffield one-screw test was done, confirming passive seating of the restoration. All the remaining multi-unit screws were inserted and torqued to their final positions. The occlusion was evaluated, and the patient gave final approval of the definitive Nexus restoration. The screw-access holes were closed, and final radiographs were taken, completing the Nexus restoration in 3 patient visits (Figure 17).
CONCLUSION
The Nexus full-arch, implant-supported restoration is a simple, efficient workflow that opens the possibilities for expanded use of the full-arch, implant-supported restoration. This is an invaluable service that will significantly improve the quality of life for potentially millions of patients.
REFERENCES
- American College of Prosthodontists. Facts & Figures. https://www.gotoapro.org/facts-figures/
- Yao CJ, Cao C, Bornstein MM, et al. Patient-reported outcome measures of edentulous patients restored with implant-supported removable and fixed prostheses: A systematic review. Clin Oral Implants Res. 2018;29 Suppl 16:241-254. doi:10.1111/clr.13286
- Adell R, Lekholm U, Rockler B, et aI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416. doi:10.1016/s0300-9785(81)80077-4
- Zarb GA, Schmitt A. Osseointegration and the edentulous predicament. The 10-year-old Toronto study. Br Dent J. 1991;170(12):439–44. doi:10.1038/sj.bdj.4807583
- Wright SP, Hayden J, Lynd JA, et al. Factors affecting the complexity of dental implant restoration—what is the current evidence and guidance? Br Dent J. 2016;221(10):615–22. doi:10.1038/sj.bdj.2016.855
- Papaspryidakos P, Yehuda D, Rajput N, et al. Digital Workflow: From guided surgery to final full-arch implant prosthesis in three visits. Compend Contin Educ Dent. 1995;39:e1-e4.
- Sobczak B, Majewski P. An integrated fully digital prosthetic workflow for the immediate full-arch restoration of edentulous patients—a case report. Int J Environ Res Public Health. 2022;19(7):4126. doi:10.3390/ijerph19074126
- Mizumoto RM, Yilmaz B. Intraoral scan bodies in implant dentistry: A systematic review. J Prosthet Dent. 2018;120(3):343–52. doi:10.1016/j.prosdent.2017.10.029
- Motel C, Kirchner E, Adler W, et al. Impact of different scan bodies and scan strategies on the accuracy of digital implant impressions assessed with an intraoral scanner: an in vitro study. J Prosthodont. 2020;29(4):309–14. doi:10.1111/jopr.13131
- Arcuri L, Pozzi A, Lio F, et al. Influence of implant scanbody material, position and operator on the accuracy of digital impression for complete-arch: A randomized in vitro trial. J Prosthodont Res. 2020;64(2):128–36. doi:10.1016/j.jpor.2019.06.001
- Lerner H, Nagy K, Luongo F, et al. Tolerances in the production of six different implant scanbodies: a comparative study. Int J Prosthodont. 2021;34(5):591–9. doi:10.11607/ijp.7379
- Mizumoto RM, Yilmaz B, McGlumphy EA Jr, et al. Accuracy of different digital scanning techniques and scan bodies for complete-arch implant-supported prostheses. J Prosthet Dent. 2020;123(1):96-104. doi:10.1016/j.prosdent.2019.01.003
- Resende CCD, Barbosa TAQ, Moura GF, et al. Influence of operator experience, scanner type, and scan size on 3D scans. J Prosthet Dent. 2021;125(2):294–9. doi:10.1016/j.prosdent.2019.12.011
- Osteon Medical. Full mouth digital implant impressions—A new novel approach [White Paper]. 2020;1.2.
- Klein M, Tuminelli FJ, Sallustio A, et al. Full-arch restoration with the NEXUS IOS® system: A retrospective clinical evaluation of 37 restorations after a one year of follow-up. J Dent. 2023;139:104741. doi:10.1016/j.jdent.2023.104741
- Gelb DA, Klein M, Tuckman M. Immediate implant placement, immediate load with same-day fully digital fabrication of a screw-retained provisional implant prosthesis. Compend Contin Educ Dent. 2023;44(5):256–6.
- Giglio GD, Giglio AB, Tarnow DP. A paradigm shift using scan bodies to record the position of a complete arch of implants in a digital workflow. Int J Periodontics Restorative Dent. 2024;44(1):115–26. doi:10.11607/prd.6733
- Lerner H. Full arch reconstruction with NEXUS iOS. DDS Mag. 2023;1:19-25.
- El-Haddad H, Judge RB, Abduo J, et al. Laboratory evaluation of novel implant metal-acrylic prosthesis design: Influence of monolithic acrylic veneer. Int J Oral Maxillofac Implants. 2020;35(1):100–6. doi:10.11607/jomi.7545
- Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706. doi:10.1016/j.adaj.2019.04.015
- Mijiritsky E, Ben Zaken H, Shacham M, et al. Variety of surgical guides and protocols for bone reduction prior to implant placement: a narrative review. Int J Environ Res Public Health. 2021;18(5):2341. doi:10.3390/ijerph18052341
ABOUT THE AUTHORS
Dr. Klein graduated from the University of Maryland School of Dentistry. He went on to complete a general practice residency program at Woodhull Medical Center in Brooklyn, NY. He received his training in oral implantology by completing a 2-year, full-time Fellowship in Oral Implantology and Biomaterials at the Brookdale University Hospital and Medical Center in Brooklyn. He then completed specialty training in prosthodontics at the University of Medicine and Dentistry of New Jersey. Dr. Klein was a clinical associate professor at the New York University (NYU) College of Dentistry in the Department of Periodontology and Implantology for 17 years. He is a Diplomate of the American Board of Oral Implantology/Implant Dentistry and the International Congress of Oral Implantology. He is a Fellow of the Academy of Osseointegration and the Greater New York Academy of Prosthodontics. He has written numerous book chapters and articles on implant dentistry. Dr. Klein speaks nationally as well as internationally on a variety of topics in oral implantology. He can be reached at mklein@keystonedental.com.
Dr. Waltuch maintains an implant practice in Cedarhurst, NY. Throughout his advanced training and clinical experience, Dr. Waltuch has acquired extensive knowledge and expertise in digital dentistry. He lectures and mentors on innovative digital implant technologies and restorative techniques. His practice is focused on comprehensive digital workflows, from fully guided surgeries to 100% digital full-arch restorations. Dr. Waltuch graduated from the NYU College of Dentistry and completed a 2-year fellowship in oral implantology. He can be reached at allon.waltuch@gmail.com.
Dr. Shulman is a general dentist who graduated from the NYU College of Dentistry. He is an active member of the Nassau County Dental Society, New York State Dental Association, and the ADA. Currently, he is in private practice in Lawrence, NY, where he focuses on restorative dentistry. He can be reached at drtshulman@gmail.com.
Disclosure: Dr. Klein is the CTO of the Keystone Dental Group. Drs. Waltuch and Shulman report no disclosures.



