Today’s dentistry is highly driven by aesthetics and the search for better health and well-being. The literature is rich with studies that address the subject of bone loss following tooth removal (Figures 1 to 4). Ridge defect can result from extraction of teeth, developmental anomalies, accidental trauma, or periodontal disease that leads to both horizontal and vertical bone loss. Ridge defects are noticeable, and prosthetic results are subpar unless the underlying deficiency is properly addressed (Figures 5 to 18).
This article will highlight 2 patient cases in which one case (case 1) will address a ridge deficiency resulting from an agenesis of two lateral incisors, and the other case (case 2) will show how to prevent a ridge deficiency immediately after extraction in a highly aesthetic zone using a rotated pediculated palatal connective tissue graft.
CASE 1
Diagnosis and Treatment Planning
A 14-year-old female presented with missing 2 lateral maxillary incisors while undergoing an orthodontic treatment (Figure 1).
A wax-up of the space was made of the site to address two components; first the symmetry of the space both right and left; and second, to study the prosthetic space providing an aesthetic dimension of the lateral incisor from its gingival margin to its incisal border. The wax-up revealed a short prosthetic spacing as shown (Figure 2). The computed tomography (CT) scan also demonstrated a buccolingual deficiency in the ridge for an ideal dental implant placement (Figure 3).
 |
 |
|
Figure 1. Young teenage patient with agenesis of teeth Nos. 7 and 10. |
Figure 2. The completed diagnostic wax-up. |
 |
 |
|
Figure 3. A cross-cut of the dental computed tomography (CT) scan demonstrating the ridge deficiency. |
Figure 4. After decortication, moldable demineralized allograft putty (Regenaform, Exatech) was placed, covered by a resorbable collagen membrane. |
 |
 |
|
Figure 5. Am ostectomy was conducted to move the crestal bone apically, creating enough spacing from the surgical stent cervical line of the future restoration. |
Figure 6. The dental implants were placed according to the surgical stent. |
 |
 |
|
Figure 7. Clinical view of the two-tapered screw-vent dental implants (Zimmer). |
Figure 8. Second stage procedure completed using the soft-tissue rolling technique. |
 |
 |
|
Figure 9. The zirconium oxide (Zimmer Contour Zirconia Abutment, Zimmer Dental) all-ceramic restorations in place. |
Figure 10. The final result demonstrates excellent aesthetics. |
The treatment plan consisted of the following:
- Ridge augmentation to correct the buccolingual deficiency
- Waiting until developmental growth of patient is complete per primary care physician and order a CT scan
- Creating a surgical stent from the wax-up after the developmental growth is completed
- Perform an ostectomy to increase the prosthetic space incisocoronally using the surgical stent
- Place the dental implant using the same surgical stent
- In 4 months, set up a second stage procedure
- The prosthetic work will be finalized about 6 to 8 weeks post second stage surgery.
Surgical Protocol
A vertical incision on the distal side of the two sites was followed by a crestal incision on the buccal end of the pontic; continuing in the sulcus of both right and left central incisors and stopping at the distal side of the papillae on both sides. A full-thickness flap was then raised and a decortication of the recipient buccal bony ridge was done. Finally moldable demineralized allograft putty (Regenaform, Exatech) was placed, covered by a resorbable collagen membrane, and the flap was laid over and sutured (Figure 4). A year later, when her growth development was achieved per her physician’s confirmation, the site preparation for dental implant placement was initiated. Using a surgical stent that was done from a second wax-up, an ostectomy was done to create a more aesthetic placement of dental implant (Figure 5) and then the dental implant was placed in both sites (Figures 6 and 7).
After 4 months of healing, a second stage procedure was done and 8 weeks of soft-tissue healing (Figure 8) and permanent prosthetic work was initiated. Zirconium oxide all-ceramic crowns (Zimmer Contour Zirconia Abutment, Zimmer Dental) were fabricated in the dental laboratory and cemented into place. In summary, the treatment protocol described above resulted in a successful aesthetic outcome for the patient (Figures 9 and 10).
CASE 2
Diagnosis and Treatment Planning
A 32-year-old female presented with a decayed tooth No. 8 (right central incisor), which was part of a full maxillary fixed prosthetic restoration. Upon removal of the roundhouse bridge, tooth No. 8 was deemed unrestorable due to a root fracture (Figure 11). The patient had a thin periodontium, with very well-defined gingival papillae, had multiple scars apically from a history of repeated apicoectomies. There was no buccal plate present. Any attempt to raise a buccal flap would have led to a serious gingival discrepancy with a complete loss of the gingival scallop.
 |
 |
|
Figure 11. Clinical image of the traumatized and scarred gingival tissues (tooth No. 8). |
Figure 12. Bone graft in place after an atraumatic extraction. |
 |
 |
|
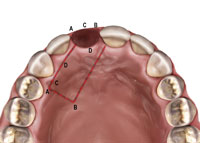
Figure 13. Illustration demonstrating the pediculated connective tissue harvesting site for the graft. |
Figure 14. Clinical application of the illustrated diagram. |
 |
 |
|
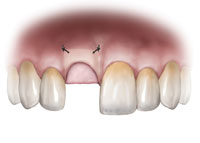
Figure 15. Diagram of the rotated palatal pediculated connective tissue graft. |
Figure 16. Clinical application of the illustrated diagram. |
 |
 |
|
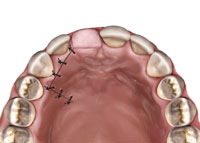
Figure 17. Illustration demonstrating the rotated connective tissue tacked under the buccal tissue pouch that was created without elevating a flap. |
Figure 18. Clinical application of the illustrated procedure. |
 |
 |
|
Figure 19. Illustration of the palatal view. |
Figure 20. The final aesthetic results. |
Surgical Protocol
An atraumatic extraction was done and a Puros Allograft (Zimmer) was placed inside the extraction socket after it was thoroughly debrided and rinsed with an antimicrobial solution (Figure 12). A PPRCT graft was collected from the palate by performing a palatal incision 2 mm from the incisal margin of teeth Nos. 7 and 6 to accommodate the buccolingual dimension of the socket. Then, a cross palate perpendicular incision was done to accommodate the mesiodistal dimension of the socket (Figures 13 and 14). Next, the connective tissue was dissected from the epithelium envelope and kept pediculated; at that point, the connective tissue graft was elevated, rotated, and fitted passively over the socket (Figures 15 and 16). Finally, the graft was then sutured in place by doing 2 horizontal mattress resorbable sutures, joining the graft to the recipient buccal flap (Figures 17 and 18). The sutures were placed on the epithelium envelope on the palate side to cover the donor site (Figure 19).
The temporary bridge was placed and was designed so it would not contact the connective tissue graft. After 8 weeks of healing, the final restorative treatment was completed (Figure 20).
CLOSING COMMENTS
Over the past 35 years, dentistry was mainly in the repair business. Patients and dentist were interested in fixing broken teeth, removing cavities, and treating gingivitis. Today’s dentistry has evolved, driven by aesthetics and the search of better health and well-being. Pictures of beautiful people with perfect smiles inundate patients from the covers of every magazine or tabloid, which can make the dentist’s job more challenging. To enhance professional and patient outcomes, an effective treatment plan that meets the patient’s expected results must be put in place. Current surgical techniques to fix ridge augmentation are getting easier and more predictable. It is incumbent on the clinician to implement implant therapy that is appropriate for achieving optimal anterior aesthetics (Figures 5, 7, 10, and 13).
REFERENCES
-
- Fugazzotto PA. Treatment options following single-rooted tooth removal: a literature review and proposed hierarchy of treatment selection. J Periodontol. 2005;76:821-831.
- Araujo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32:212-218.
- Nevins M, Camelo M, De Paoli S, et al. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006;26:19-29.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313-323.
- Keith JD Jr, Salama MA. Ridge preservation and augmentation using regenerative materials to enhance implant predictability and esthetics. Compend Contin Educ Dent. 2007;28:614-623.
- Park SH, Lee KW, Oh TJ, Misch CE, Shotwell J, Wang HL. Effect of absorbable membranes on sandwich bone augmentation. Clin Oral Impl Res 2008;19:32-41.
- Wang HL, Shotwell JL, Itose T, Neiva RF. Multidisciplinary treatment approach for enhancement of implant esthetics. Implant Dent. 2005;14:21-29.
- Fugazzotto PA. Maintaining primary closure after guided bone regeneration procedures: introduction of a new flap design and preliminary results. J Periodontol. 2006;77:1452-1457.
- Covani U, Barone A, Cornelini R. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets. A case series. J Periodontol. 2003;74:268-273.
- Liu CL. The impact of osseointegrated implants as an adjunct and alternative to conventional periodontal prosthesis. Compend Contin Educ Dent. 2005;26:653-654, 656, 659-660.
- Block MS, Finger I, Lytle R. Human mineralized bone in extraction sites before implant placement. Preliminary results. J Am Dent Assoc. 2002;133:1631-1638.
- Jackson BJ, Morcos I. Socket grafting: a predictable technique for site preservation. J Oral Implantol. 2007;33:353-364.
- Mathews DP. The pediculated connective tissue graft: A novel approach for the “blown-out” site in the esthetic zone. Compend Contin Educ Dent. 2008; 29:350-357.
- Machtei EE. The effect of membrane exposure on the outcome of regenerative procedures in humans: A meta-analysis. J Periodontol. 2001;72:512-516.
- Brugnami F, Then PR, Moroi H, Kabani S, Leone CW. GBR in human extraction sockets and ridge defects prior to implant placement: clinical results and histologic evidence of osteoblastic and osteoclastic activities in DFDBA. Int J Periodontics Restorative Dent. 1999;19:259-267.
- Smukler H, Landi L, Setayesh R. Histomorphometric evaluation of extraction sockets and deficient alveolar ridges treated with allograft and barrier membrane: a pilot study. Int J Oral Maxillofac Implants. 1999;14:407-416
- Wang HL, Tsao YP. Histologic evaluation of socket augmentation with mineralized human allograft. Int J Periodontics Restorative Dent. 2008;28:231-237.
- Minichetti JC, D’Amore JC, Hong AYJ, Cleveland DB. Human histologic analysis of mineralized bone allograft (Puros) placement before implant surgery. J Oral Implantol. 2004;30:74-82.
BIO
Dr. El Chaar oversees a private practice on Park Avenue in New York City that specializes in oral health, dental implants, periodontal and gum disease and oral cosmetic surgery. In addition to his practice, he is a clinical associate professor of periodontics and implant dentistry, surgical director of the continuing education (CE) dental implant program at the New York University (NYU) College of Dentistry, and visiting professor at the Saint Joseph University in Beirut, Lebanon. Dr. El Chaar completed his postgraduate education in advanced periodontics and received his masters degree in oral biology from NYU. He launched the EEC Institute in New York City, a CE program for general practitioners and specialists. In addition to being a diplomate of the American Board of Periodontology, Dr. El Chaar is also a member of the American Academy of Periodontology, the Academy of Osseointegration, and the American Board of Oral Implantology/Implant Dentistry. He can be reached at info@edgardelchaar.com oredgardelchaar.com.











