 |
| Figure 1. Chronic periodontitis. |
 |
| Figure 2. More than “just a prophy.” |
 |
| Figure 3. Healthy gingiva. |
 |
| Figure 4. Gingival inflammation and bleeding upon tooth brushing. |
When you have a periodontal patient seated in your chair, what is your first reaction? Do you get excited about the opportunity to improve your patient’s oral and systemic health? Do you feel privileged for landing a case that will contribute significantly to your practice’s bottom line? Or, do you cringe at the thought of losing money from potential cancellations and the patient’s limited insurance coverage?
Unfortunately, for many dentists, the latter answer is common. While an ideal periodontal treatment plan and subsequent payment could mean bonuses for all the team members, patients and insurance companies aren’t as eager to fork over payment. Not only do patients cancel appointments to save money, but also many insurance companies cover only a limited number of supporting periodontal therapy (SPT) appointments. Many dental practices even shortchange themselves by attempting to bill the periodontal maintenance visit as a prophy. Devaluing a treatment procedure is unheard of in the medical field, so why should we do this?
In the next few pages, I will present 6 points to help your hygiene team improve the oral health of your patients as well as your practice’s financial health.
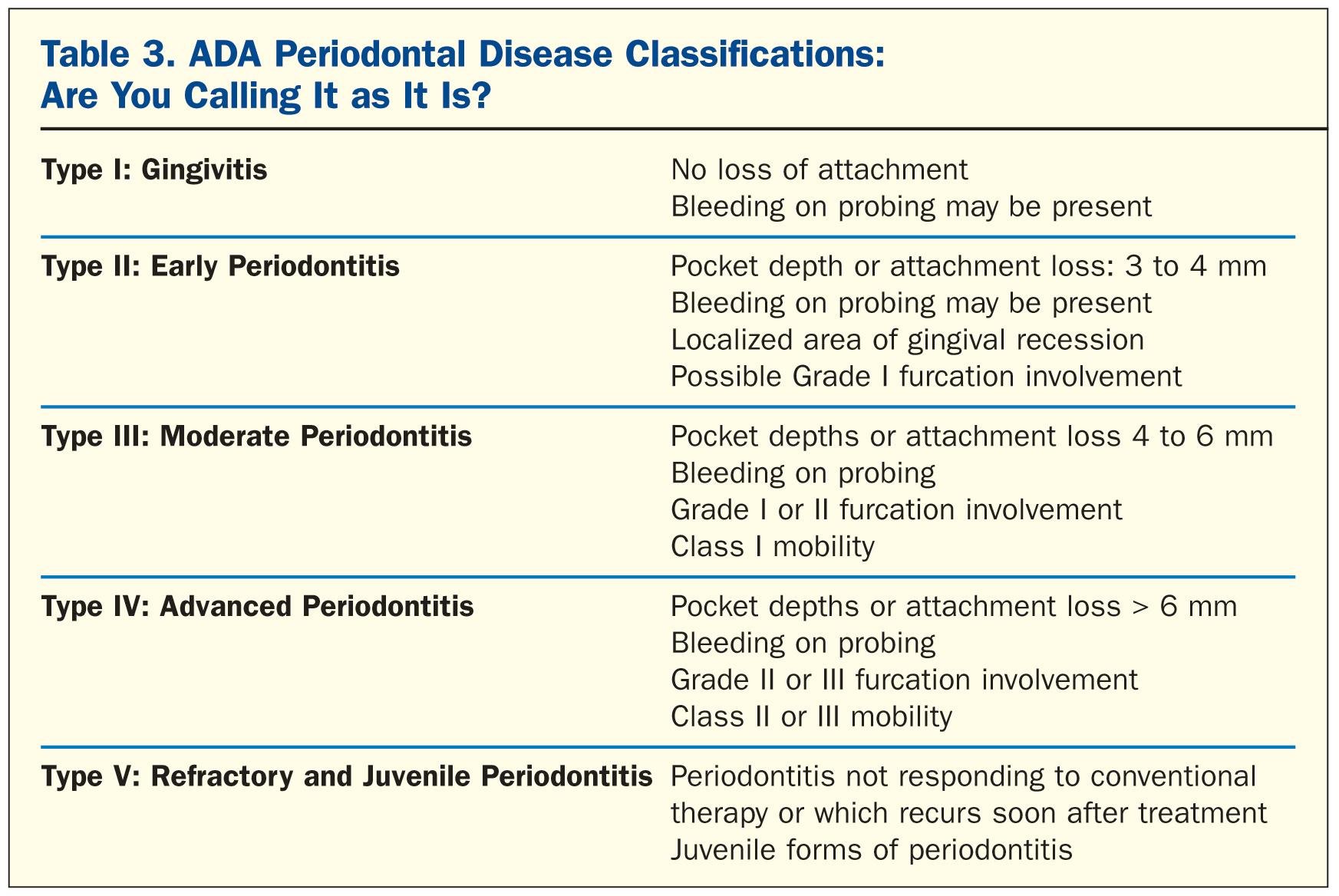
1. Prioritize the Assessment
There are 2 major reasons perio patients fall through the cracks. First, as previously pointed out, is the financial barrier. The hygienist knows that he or she is dealing with a perio patient, but the patient is skipping appointments, or the office is billing for a prophy because that’s what insurance will cover. The second reason is inadequate (or infrequent) assessments. If you are scaling more than 20 minutes during a regular continuing care appointment, your patients need a thorough assessment for periodontal disease before proceeding with any more prophy visits (Figures 1 to 3). Scaling more than 20 minutes is usually a sign that your patient was in need of more than just a prophy appointment. Be vigilant of when you need to pick up the periodontal probe before proceeding with a curette.
I have also seen these 2 reasons combined: many insurance companies won’t cover 4 SPT appointments per year, and the dental office skips periodontal assessments (or even treatments), only providing a glorified prophy. The problem: How, then, does the dental team know whether this patient needs more periodontal therapy?
When periodontal patients fall off the radar, not only does your hygiene profit center suffer, but no one enjoys an office that goes into overdrive when the hygienist feels pressured to take extra time for a prophy. The patient’s systemic health is also a concern. Once a patient has periodontal disease, he or she may face challenges with future systemic diseases. For example, something as simple as the flu can exacerbate periodontal disease.1
If the hygienist doesn’t pick up a probe, the patient may not receive proper treatment. Including thorough oral health assessments in the dental hygiene appointment will catch hidden issues, generating additional profit opportunities for the practice. Also, for the patient’s sake, you want to diagnose disease early and begin nonsurgical periodontal therapy sooner rather than later. The periodontal screening exam should be at the top of your list for every new patient and for every current patient who shows warning signs, such as areas of recession, bleeding upon tooth brushing, gingival inflammation, etc. An annual periodontal screening is key to diagnosing periodontal disease, which will give you the green light for Phase I therapy. When a patient completes Phase I treatment for nonsurgical periodontal therapy, each one is now and forever considered a periodontal patient (Figure 4).
2. Use Effective Communication
When you know the facts, and deliver them clearly to the patient, you are one step closer to sealing the deal on optimal care. We have a responsibility to educate our patients about the state of their oral condition. To avoid getting too technical with the science, use the highlights below:
• Describe what periodontal disease is and how it affects the gums, bone, and teeth. Keep this description under 2 minutes. Using photos is recommended for a stronger impact. Showing patients pictures of diseased areas in their own mouth (or radiographs) leaves quite an impression, too. Use the intraoral camera to take a tour of your patient’s mouth, take photos to show, and this paints a great picture of reality for the patient.
• Explain that periodontal disease is episodic and what that means for the treatment approach. Even if perio patients seem healthy for many years after the scaling and root planing (SRP), the disease process can return at any time. So, from this point indefinitely, they need to return every 12 weeks, or at frequent, appropriate intervals for maintenance. Mention the link between oral health and overall systemic health.
• Many patients are not aware of this connection, so do not assume they know. The US Surgeon General, in March 2011, confirmed this research,2 and you can share this information with your patients to grab their attention. There also are many research citations that link oral health to systemic health such as heart disease, low-birthweight babies, pneumonia, etc.3
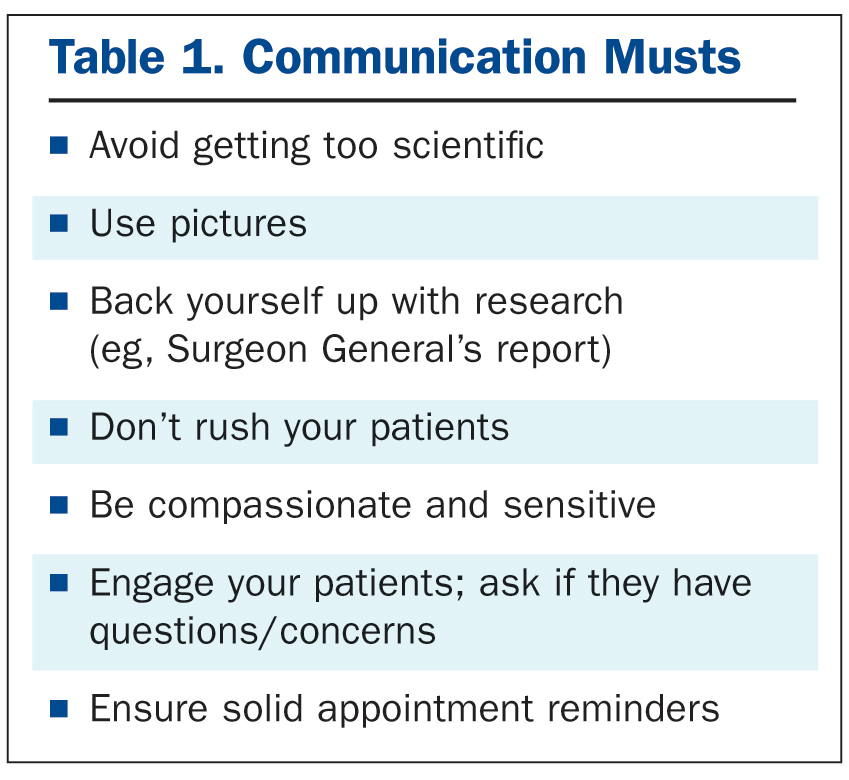 Keep yourself educated about all these systemic links to periodontal disease as they are constantly evolving and changing. When we understand the research regarding periodontal pathogens, we can better communicate to our patients why they need to return every 3 or 4 months. Having a full disclosure of the facts, patients will appreciate your honesty. Many of your patients will want to know all the science, facts, and evidence to support their decisions.
Keep yourself educated about all these systemic links to periodontal disease as they are constantly evolving and changing. When we understand the research regarding periodontal pathogens, we can better communicate to our patients why they need to return every 3 or 4 months. Having a full disclosure of the facts, patients will appreciate your honesty. Many of your patients will want to know all the science, facts, and evidence to support their decisions.
Good and effective communication also includes how you deliver the facts. Although you may feel rushed, it is important to be compassionate and sensitive. No one likes hearing bad news about their teeth, let alone the dental bill that comes along with it. Take a moment to sit your patient up in the chair to avoid the f
eeling that you are giving them a lecture. Tone of voice can make or break the conversation. Patients need to know you are on their side. For example, if a patient is notorious for skipping SPT visits, speak to him or her with genuine concern, as an equal, not as a scolding authority figure. Pause for questions as well. Engage the patient in a dialogue so you know you have his or her attention. Finally, listen to your patient’s concerns. Good listening is a big part of good communication and will help build a lasting relationship (Table 1).
Patients will feel they can trust you when you take time to communicate effectively, at a level they understand and when they know that you care about their well-being. When patients understand you and trust you, they are most likely to follow through with future appointments. They are also more willing to pay in full when they understand the impact of periodontal disease on their overall health. These are the patients who become your raving fans.
A final note on communication: In addition to getting your point across that periodontal maintenance is critical, good communication also comes in the form of appointment reminders and confirmations. If you have trouble with cancelled appointments, consider re-examining this side of your office’s communication system. Today’s technology has some answers that may support you in this area.
 3. Insist on Early Intervention
3. Insist on Early Intervention
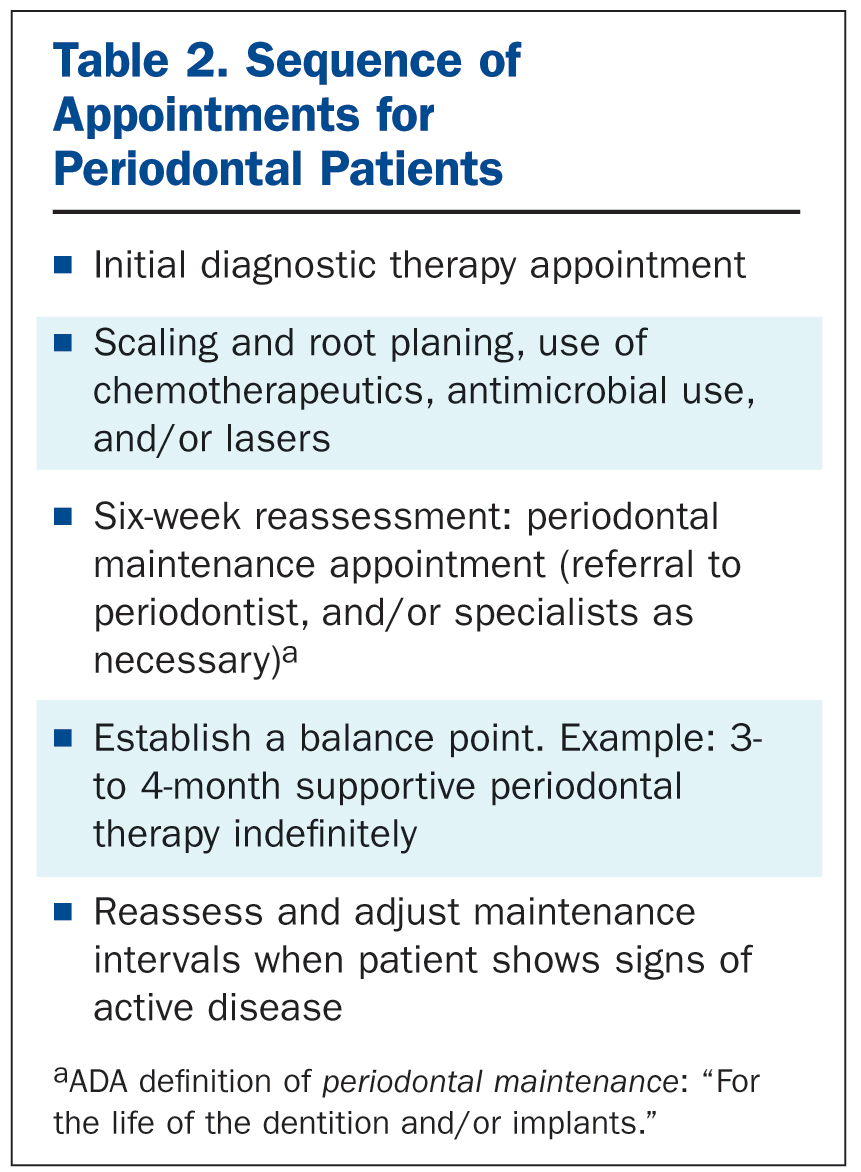
When you assess and diagnose periodontal disease, don’t delay with treatments. Nip the disease progression in the bud with scaling SRP, home care, and supportive micronutrients. Bone loss may already have begun or be waiting right around the corner; if you do not intervene early, it can become aggressive very easily. On the other hand, early nonsurgical intervention can actually reverse periodontal disease for a patient with few risk factors.4
After SRP, keep the ball rolling with the 6-week reassessment appointment and establish the balance point for future SPT visits. This is the first of future periodontal maintenance appointments. If a patient with no risk factors begins treatment during the early stage of periodontal disease, the patient’s periodontium has the greatest chance to quickly heal and halt the progression of further progression of diseases after Phase I is complete (Table 2).5
As part of early intervention (and subsequent periodontal maintenance appointments), removal of biofilm and microbes is a key preventive measure.6 Periodontal pathogens will repopulate a healthy and recently scaled sulcus as early as 9 weeks after scaling.7. Some clinical studies have shown that even after one week, a complex subgingival microbiota can develop—and that’s just with the bacteria from the supragingival environment.8 These startling facts explain why even the most compliant home care routine will not allow patients to escape the episodic nature of periodontal disease.
You may also enhance your clinical outcomes by using adjunctive therapy (following root debridement) with a bactericidal irrigant activated by a cold laser.9 When a patient has a pocket depth of 5 mm or greater, always consider the use of lasers, antimicrobials, and micronutrients.
Early intervention also offers more promise to periodontal patients with coexisting systemic diseases. For example, one study revealed that patients with Crohn’s disease experienced a decrease in the enzymes that would normally increase inflammation in the sulcus (as well as the body) after receiving proper, timely treatment for periodontal disease.10 Even patients with Type 2 diabetes and periodontal disease have been found to experience improved glycemic control after receiving nonsurgical periodontal therapy.11
4. Push for Stellar Home Care
Patients can come in every 3 or 4 months to see their hygienist, but what they do in between appointments contributes to 80% of the final outcome. The same concept works for diet and exercise. If a person sees a personal trainer twice a week, but eats an unhealthy diet at home, all the exercise at the gym loses its value.
Here are a few suggestions to discuss with your patients when talking about home care:
- Appropriate toothpaste to use for each patient’s oral condition(s)
- Product ingredients best for each individual patient
- Which mouthrinse to use and which to avoid (ie, ingredients: alcohol, etc)
- Alcohol versus chlorhexidine versus chlorine dioxide
- Interproximal cleaning aids (what type of floss, proxabrush, etc)
- Tongue cleaners
- Fluoride, xylitol, etc
- Micronutrients
 While on the topic of home care, I want to emphasize that this is the dental professionals’ domain. We need to build a reputation with our patients that we are the “go to” source for questions about the best products to buy, what to avoid, customizing to a patient’s individual needs, etc. Unfortunately, most patients choose their products from the influence of TV ads, the Internet, convenience, or a sales associate at the drug store. Even most pharmacists are not educated about oral health and which one is best to use for what oral condition.
While on the topic of home care, I want to emphasize that this is the dental professionals’ domain. We need to build a reputation with our patients that we are the “go to” source for questions about the best products to buy, what to avoid, customizing to a patient’s individual needs, etc. Unfortunately, most patients choose their products from the influence of TV ads, the Internet, convenience, or a sales associate at the drug store. Even most pharmacists are not educated about oral health and which one is best to use for what oral condition.
We, as dental professionals, will do both our reputations and dental practices a favor if we take a more vocal and proactive approach regarding home care. This is yet one more thing we can do to develop a trusting relationship with our patients, as well as a way we can ensure we’re sending the patient home with good instructions for optimal oral health. In today’s world, many dental offices have opted to carry specific home care products to offer their patients. Compliance is much higher when a patient can conveniently purchase the correct product in the dental office, as opposed to either buying the wrong product at the drug store or forgetting altogether. Plus, having home care products available for your patients to purchase is just one more income source you can add to your bottom line.
5. Practice Appropriate Insurance Billing
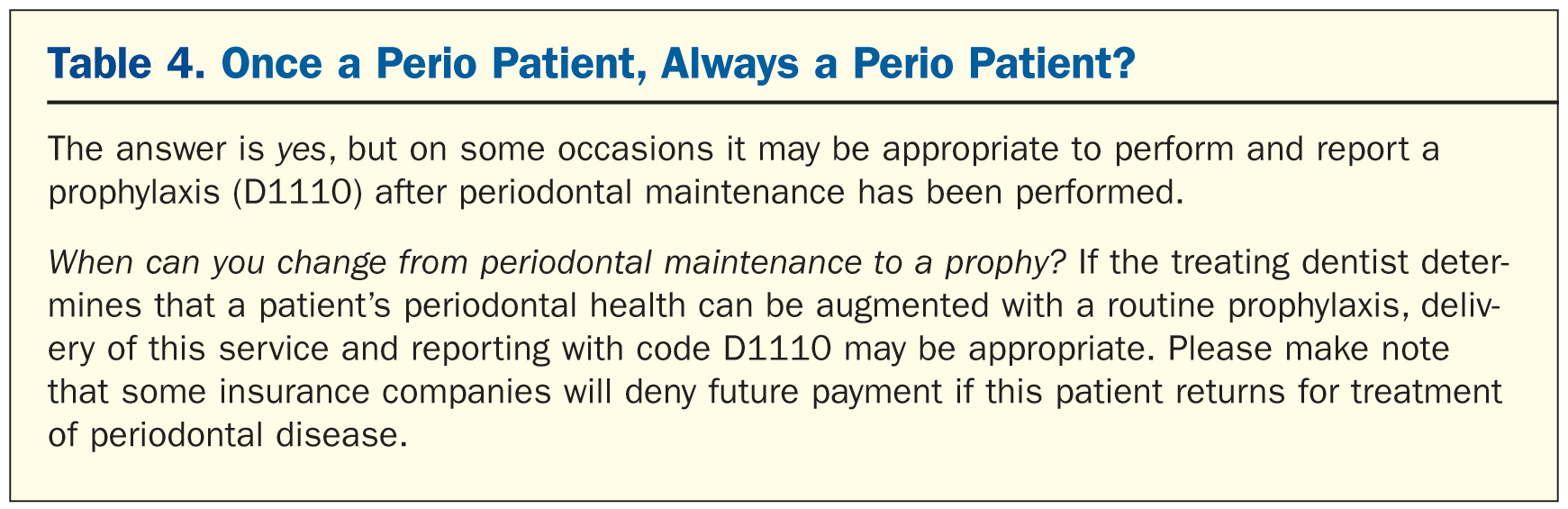
Dental practices are concerned about money in this economic climate, yet in an attempt to boost income, many have actually hurt their incomes by billing insurance for a prophy when the patient actually had a periodontal maintenance visit (Table 3). Many insurance companies will pay for only 2 periodontal maintenance (SPT) appointments per year, so dental offices will often bill the insurance company for a prophy 2 times a year and then the SPT visits 2 times.
The problem with this is that you are selling yourself short of payment for a true SPT visit, and you are selling the patient short of the treatment he or she really needs. When a perio patient receives a prophy, he or she is missing out on necessary scaling in the deep pockets and adjunctive antimicrobial/laser treatments. The patient is also missing out on an important periodontal exam or simple assessment to re-evaluate the areas of previous disease. If a 6-mm pocket measures 4 mm after SRP, the chances of
the pocket quickly returning to 5 mm, 6 mm, or higher are very likely. Therefore, you will always need to pick up a probe to measure before scaling. If the probe is not used prior to scaling on every previously diagnosed periodontal patient, you are likely to miss the episodic disease process.
If you have a periodontal patient seated in your chair for treatment and yet you bill for a prophy to collect what you can, sit down with your team and discuss why this is happening. Is the patient unable to pay? Do you feel obligated to provide “a cleaning” even if a patient can’t pay for a more advanced level of care? Do you believe it’s better to have some reimbursement than none? Discuss how you might change this policy. Perhaps a simple conversation with the patient is all you need. Even if the patient has mentioned financial hardship before, check in with him or her again. Things may have changed.
Utilize a brochure or diagram about periodontal disease and review this at the time of diagnosis, but also take time, when circumstances arise, to review treatment approaches and education to support patients who will need to return for necessary maintenance visits each year. You might also discus with your team creating flexible payment arrangements (Care Credit and other low percentage interest payment options) for patients who can’t afford SPT visits or may not be covered by insurance.
Also some food for thought: When a patient presents with periodontal disease, from a legal and ethical view, you can’t bill for something that has not truly been completed.
In the United States, periodontal maintenance is billed as code D4910, which contains the phrase “for the life of the dentition.” You can take this quite literally as “once a periodontal patient, always a periodontal patient” (Table 4).
6. Use Positive Reinforcement
Periodontal disease is not a fun topic for patients, so be sure to let them know when things are going well. Do not judge your patients, and allow them to feel good about their accomplishments with their overall health. When they are aware of progress and the payoff of returning for routine periodontal maintenance (SPT) appointments, they will be more likely to stay compliant.
Emphasize the benefits of periodontal maintenance (SPT) appointments. Talk with your patients about both short-term and long-term benefits, from improvements in their smile to overall improved health and a longer life. Most people want to feel good and enjoy a longer, healthier life, which is the main reason behind early intervention.
Another positive approach is to involve your patients in goal setting. Create a chart to help measure their successes, and share these results at consecutive appointments. Make a big deal about the positive results your patient achieves. Most dental computer software can create a patient chart of their periodontal disease process. You can also overlap previous appointment results with today’s results utilizing more of the dental software programs. If your computer software allows you to document these exams, share the chart with your patients and print it out for their active participation. Patients can take home printed results and celebrate their concrete results. Use the intraoral camera and take photos to share with the patient.
Finally, support successes—even the small ones. Provide ample positive reinforcement when your patient does something positive, such as improving flossing habits. Appreciate the baby steps your patient has taken. It’s about helping people believe they can conquer the disease process. If you show confidence in your patient, he or she is more likely to keep trying. Check back to see if your patients followed through, be enthusiastic with them, and celebrate their successes when they accomplish any of their goals. It’s the follow-up and the caring that really counts and will keep patients coming through your front door and worry less about the cost. Nothing motivates people as much as knowing someone cares.
References
- Institute of Medicine. Advancing Oral Health in America. Washington DC: The National Academies Press; 2011. hrsa.gov/publichealth/clinical/oralhealth/advancingoralhealth.pdf. Accessed March 13, 2013.
- US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General—Executive Summary. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2011. nidcr.nih.gov/DataStatistics/SurgeonGeneral/Report/ExecutiveSummary.htm. Accessed March 13, 2013.
- Li X, Kolltveit KM, Tronstad L, et al. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13:547-558.
- Personal and provider approaches to oral health. In: US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General—Executive Summary. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2011. nidcr.nih.gov/datastatistics/surgeongeneral/sgr/chap8.htm. Accessed March 13, 2013.
- Newman MG, Takei HH, Klokkevold PR. Carranza’s Clinical Periodontology. 11th ed. St. Louis, MO: Elsevier Saunders; 2012.
- Offenbacher S, Barros SP, Singer RE, et al. Periodontal disease at the biofilm-gingival interface. J Periodontol. 2007;78:1911-1925.
- Mousqués T, Listgarten MA, Stoller NH. Effect of sampling on the composition of the human subgingival microbial flora. J Periodontal Res. 1980;15:137-143.
- Quirynen M, Vogels R, Pauwels M, et al. Initial subgingival colonization of ‘pristine’ pockets. J Dent Res. 2005;84:340-344.
- Andersen R, Loebel N, Hammond D, et al. Treatment of periodontal disease by photodisinfection compared to scaling and root planing. J Clin Dent. 2007;18:34-38.
- Stein JM, Lammert F, Zimmer V, et al. Clinical periodontal and microbiologic parameters in patients with Crohn’s disease with consideration of the CARD15 genotype. J Periodontol. 2010;81:535-545.
- Lang NP, Tonetti MS, Suter J, et al. Effect of interleukin-1 gene polymorphisms on gingival inflammation assessed by bleeding on probing in a periodontal maintenance population. J Periodontal Res. 2000;35:102-107.
Ms. Seidel-Bittke is founder of Dental Practice Solutions, and has successfully designed efficient dental hygiene departments that result in high performance dental teams for more than 13 years. She is an accomplished author who speaks internationally about her signature systems and services for the dental hygiene department. In 1984, she graduated from the University of Southern California (USC) in Los Angeles, Calif, with a bachelors degree in dental hygiene. She is a former clinical assistant professor from USC in Los Angeles. Ms. Seidel-Bittke is also a former denta
l hygiene program director for a school in Portland, Ore. She works with dental practices throughout the world implementing her signature dental hygiene systems and is considered one of the Leaders in Dental Consulting by Dentistry Today. She can be reached at (888) 816-1511, at dentalpracticesolutions.com, or via email at support@dentalpracticesolutions.com.
Disclosure: Ms. Seidel-Bittke reports no disclosures.


